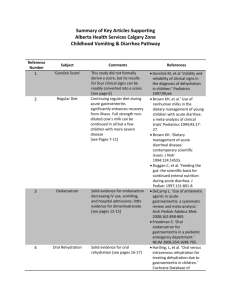
Summary of Key Articles Supporting
advertisement

Summary of Key Articles Supporting Alberta Health Services Calgary Zone Childhood Vomiting & Diarrhea Pathway Reference Number Subject Comments References 1 ‘Gorelick Score’ Gorelick M, et.al.‘Validity and reliability of clinical signs in the diagnosis of dehydration in children.’ Pediatrics 1997;99;e6 2 Regular Diet This study did not formally derive a score, but its results for four clinical signs can be readily converted into a score. [hyperlink to slide 12, ACH teaching slides] Continuing regular diet during acute gastroenteritis significantly enhances recovery from illness. Full strength nondiluted cow’s milk can be continued in all but a few children with more severe disease [hyperlink to slides 45-49, Texas teaching slides] 3 Ondansetron Solid evidence for ondansetron decreasing IV use, vomiting, and hospital admissions; little evidence for dimenhydranate [Hyperlink to slide 13-16, ACH teaching slides] 4 Oral Rehydration Solid evidence for oral rehydration [Hyperlink to slide 20-21, ACH Teaching Slides] Brown KH, et al.‘ Use of nonhuman milks in the dietary management of young children with acute diarrhea: a meta-analysis of clinical trials’ Pediatrics 1994;93:1727. Brown KH. ‘Dietary management of acute diarrheal disease: contemporary scientific issues. J Nutr 1994:124:1455S. Duggan C, et al. ‘Feeding the gut: the scientific basis for continued enteral nutrition during acute diarrhea. J Pediatr 1997;131:801-8 DeCamp L. ‘Use of antiemetic agents in acute gastroenteritis: a systematic review and meta-analysis.’ Arch Pediatr Adolesc Med. 2008;162:858-865. Freedman S. ‘Oral ondansetron for gastroenteritis in a pediatric emergency department.’ NEJM 2006;354:1698-705. Hartling, L, et al. ‘Oral versus intravenous rehydration for treating dehydration due to gastroenteritis in children.’ 5 Choice of oral rehydration fluid 6 Assessment of Dehydration 7 Rapid Rehydration 8 Nasogastric Rehydration Solid Evidence for low-sodium (75 meq/l) WHO formulation (superior to 90 mg/l Na), but no evidence for Pedialyte (45 meq/l). However Pathway Committee elected to use Pedialyte for several practical reasons: 1) Low sodium WHO formulation not available in Canada, 2) Pedialyte used in virtually all Canadian Children’s Hospitals, 3) Pedialyte widely available in community pharmacies, 4) No published evidence of adverse effects, 5) Based on blinded test by Committee members, Pedialyte judged to be best tasting, and 6) Pedialyte provided to AHS free of charge by Ross. No single sign is very accurate. However signs on physical exam are best (capillary refill, poor overall appearance, dry mucuous membrance) in contrast with reported symptoms by parents. No RCTs have been published (one RCT likely to be published soon) [Hyperlink to slide 24, ACH teaching slides] If IV access cannot be obtained in children with either severe dehydration who are clinically stable or moderate dehydration who have failed oral rehydration, consider NG Cochrane Database of Systematic Reviews 2006, Issue 1. Spandorfer P. ‘Oral versus intravenous rehydration of moderately dehydrated children: a randomized, controlled trial.’ Pediatrics 2005;115:295–301. Hahn S, et al. ‘Reduced osmolarity oral rehydration solution for treating dehydration caused by acute diarrhoea in children.’ Cochrane Database of Systematic Reviews 2002, Issue 1. Steiner M, et. al. ‘Is This Child Dehydrated?’ JAMA. 2004;291:2746-2754 Gorelick M. ‘Rapid intravenous rehydration in the ED: a systematic review.’ PemDatabase.Org Nager et al. ‘Comparison of nasogastric and intravenous methods of rehydration in pediatric patients with acute dehydration.’ Pediatrics 9 Hypo/Hypernatremia 10 Addition of glucose to IV fluid 11 Probiotics 12 Dioctahedral smectite 13 Loperamide hydration as an option to IV rehydration. [Hyperlink to slide 23, ACH teaching slides] Administration of hypotonic IV fluids to children with dehydration occasionally results in profound hyponatremia which can be fatal. Administer only isotonic IV fluids to children with dehydration. [Hyperlink to slide 25, ACH teaching slides] While there is some evidence (one retrospective case-control study) to suggest treating patients with dehydration with glucose containing IV fluids reduces rate of return to care, the pathway committee thought the evidence was not sufficiently strong to recommend its routine use. Routinely adding D5 to IV hydration fluids is not recommended. While some strains have been shown to be effective at reducing duration of diarrhea, products available in Canada have either known significant adverse effects (risk of sepsis), inadequate quality control, or not proven to be effective. Not recommended. [Hyperlink to slide 19 and 20, ACH teaching slides] Widely used in Europe for children with diarrhea. Evidence supports its benefit but no commercial products are available in Canada. [Hyperlink to slide 20, ACH Teaching Slides] Effective at reducing duration 2002;109:566–72 Choong K. ‘Hypotonic versus isotonic saline in hosptialised c 24ildren: a systematic review.’ Arch Dis Child 2008;91:828-835. Reynolds R, et al. ‘Disorders of sodium balance.’ BMJ 2006;332:702–5. Moritz M, et al. ‘Disorders of water metabolism in children: hyponatremia and hypernatremia.’ 2002;23:371. Levy J, et al. ‘Intravenous dextrose during outpatient rehydration in pediatric gastroenteritis.’ Acad Emerg Med. 2007;14:324-331. Allen S, et al. ‘Probiotics for treating infectious diarrhoea.’ Cochrane Database of Systematic Reviews. 2004 Szajewska H, et al. ‘Metaanalysis: Smectite in the treatment of acute infectious diarrhoea in children.’ Aliment Pharmacol Ther 2006;23:217 Li S, et al. ‘Loperamide of diarrhea, but associated with significant side effects. Not recommended. [Hyperlink to slide 17, ACH Teaching Slides] therapy for acute diarrhea in children: systematic review and Meta-Analysis.’ PloS Med 2007;4: e98.