Acute Diarrhoea and Gastroenteritis in Childhood
advertisement

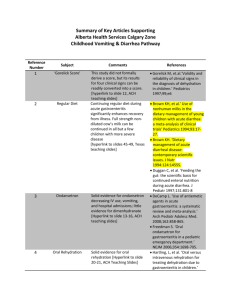
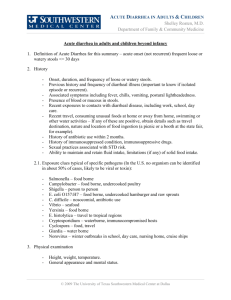
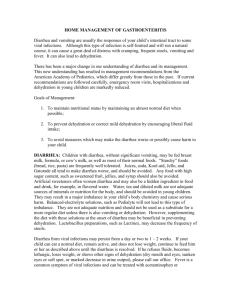
Acute Gastroenteritis in pediatric population Definitions and Terms: Acute Gastroenteritis (AGE): diarrheal disease of rapid onset, with or without accompanying symptoms, signs, such as nausea, vomiting, fever, or abdominal pain Diarrhea: the frequent passage of unformed liquid stools (3 or more loose, watery stool per day) Dysentery: blood or mucus in stools Diarrhea Acute diarrhea: Short in duration (less than 2 weeks). Chronic diarrhea: 6 weeks or more Statistics in the United States: • • • • • > 1.5 million outpatient visits/year 200,000 hospitalizations/year 300 deaths/year 9% of all hospitalizations of children <5yo Children <3yo estimated at 1.3-2.3 episodes/child/year Statistics Worldwide: • diarrheal disease is leading cause of pediatric morbidity and mortality • 1.4 billion episodes of diarrhea annually • 1.5-2.5 million deaths annually in children <5yo (19% of all child deaths- 98% of these deaths occurring in the developing world) Etiologies: Viral 70-85% of AGE in developed countries • Rotavirus: 1/3 of all pediatric AGE hospitalizations in U.S. Seasonal variation: increased in winter and decreased in summer. • Caliciviruses, astroviruses, and enteric adenoviruses Presentaion: • Low-grade fever • Vomiting followed by copious watery diarrhea (up to 1020 bowel movements per day) • Symptoms persisting for 3-8 days Etiologies: Bacterial Campylobacter, Salmonella, Shigella, E. coli, Yersinia, Clostridium difficile Presentation: High fevers Shaking chills Bloody bowel movements (dysentery) Abdominal cramping & fecal leukocytes *ETEC is unlikely to cause dysentery. Etiologies: Parasitic Giardia and Cryptosporidium <10% of cases Presentation: • Watery stools • Low-grade fever • differentiated from viral gastroenteritis by a protracted course or history of travel to endemic areas Pathophysiology The 2 primary mechanisms (1) Damage to the villous brush border of the intestinemalabsorption of intestinal contents an osmotic diarrhea (2) Release of toxins that bind to specific enterocyte receptorsrelease of chloride ions into the intestinal lumensecretory diarrhea Sign & Symptoms • • • • • • • • • • • • Nausea & Vomiting Diarrhea Loss of appetite Fever Headaches Abdominal pain Abdominal cramps Bloody stools Fainting and Weakness Heartburn Dehydration Lethargic Complication • Dehydration Excessive loss of fluids and minerals (electrolytes) from the body Common in infants and young children with viral gastroenteritis or bacterial infection Kidney failure, eg in infection by E.coli • Electrolyte deficiency • Irritation DDX • • • • • • • • • • • • • • • • • Food poisoning Lactose intolerance Malabsorption syndromes Irritable bowel syndrome Diabetic Ketoacidosis Appendicitis Peptic Ulcer Disease Foreign Body Ingestion Intussusception Volvulus Hemolytic Uremic Syndrome Pyloric Stenosis Hepatitis Urinary Tract Infections and Pyelonephritis Inflammatory Bowel Disease Septic shock Pancreatitis Work-Up Diagnosing gastroenteritis is mainly an exclusion procedure History & Physical 2 vital functions: (1) Differentiating gastroenteritis from other causes of vomiting and diarrhea in children (2) Estimating the degree of dehydration. Consider: Duration, frequency, quality, quantity, last episode, +/- factors, associated symptoms, diet/med/travel/sick contact hx. Work-Up Assessment of Dehydration Ideally, acute change in weight is the best way to determine degree of dehydration. Clinical signs and symptoms can be utilized to determine degree of dehydration Work-Up Labs The vast majority of children presenting with acute gastroenteritis do not require serum or urine tests Moderate-severe dehydration: Electrolytes, bicarbonate, and urea/creatinine Fecal leukocytes and stool culture Evidence of systemic infection-complete workup: CBC and blood cultures. If indicated, urine cultures, chest radiography, and/or LP Treatment Factors: Severe or prolonged episode Fever Repeated vomiting, Refusal to drink fluids Severe abdominal pain Blood or mucus in stool Sign of dehydration Dry, sticky mouth Few or no tears when crying Sunken eyes Lack urine or wet diaper Dry, cool skin Fatigue or dizziness Treatment Fluid Management Factors: Status of patient & dehydration degree Oral rehydration therapy -as effective as IV fluids in treatment of mild to moderate dehydration both OP & IP. Delivered po or ng. • Some studies have demonstrated decreased ER stays and increased parent satisfaction with ORS therapy over IV • NO difference in duration of illness or hospitalization rates. Treatment Fluid Management Oral rehydration solutions (ORS) -carbohydrate (glucose or rice syrup) & electrolytes (Na, K, Cl, citrate, HCO3-) -Takes advantage of a specific sodium-glucose transporter (SGLT-1) to increase the reabsorption of sodium, which leads to the passive reabsorption of water. Treatment Fluid Management Rehydration protocols: Mild: 50-100 cc/kg of ORS plus replacement over 4 hours** Moderate: 100cc/kg of ORS plus replacement over 4 hours Severe: Bolus of 20-30 cc/kg lactated Ringer's (LR) or normal saline (NS). 20cc/kg of isotonic IV fluids over one hour Repeat as necessary Continue replacement for stools ** ongoing losses can be matched at approximately 10cc/kg for each stool & 2cc/kg for each emesis episode. Treatment Feeding and nutrition -Normal diet as rapidly as possible. -Early feeding reduces illness duration and improves nutritional outcome. Breastfed infants -Continue breastfeeding throughout the rehydration and maintenance phases. Formula fed infants -Restart feeding once the rehydration phase is complete (ideally in 2-4 h). - Fatty foods and foods high in simple sugars should be avoided. -Lactose-free formulas are unnecessary; 80% of children could tolerate full strength milk. -“BRAT” diet and other restrictive diets are unnecessary and provide suboptimal nutrition Treatment Medication: Antimicrobials Generally not indicated C difficile- stop antibiotic & start metronidazole Cholera-tetracycline and doxycycline Giardia-metronidazole Cryptosporidium-metronidazole or Nitazoxanide Treatment Medication: Antidiarrheals are not recommended Antiemetics are not recommended Some clinical studies have demonstrated that ondansetron can decrease vomiting and hospitalization. Probiotics (e.g. Lactobacillus GG) alter the composition of gut flora and assist in restoring normal gut function. Prevention • • • • Vaccination-RotaTeq & Rotarix Probiotics Washing hands. Clean food preparation & preservation. Reference • Dennehy PH. Acute diarrheal disease in children: epidemiology, prevention, and treatment. Infect Dis Clin North Am. Sep 2005;19(3):585-602. • "NHS Direct: Gastroenteritis". http://www.nhsdirect.nhs.uk/checksymptoms/topics/gastroenteritis. Retrieved 12/16/2010. • World Health Organization – WHO http://www.who.int/topics/diarrhoea/en • Kosek M, Bern C, Guerrant RL. The global burden of diarrhoeal disease, as estimated from studies published between 1992 and 2000. Bull World Health Organ. 2003;81(3):197-204. • King CK, Glass R, Bresee JS, Duggan C. Managing acute gastroenteritis among children: oral rehydration, maintenance, and nutritional therapy. MMWR. 2003; 52(RR16): 116.