NATIONAL PATHOLOGY ACCREDITATION ADVISORY
COUNCIL
REQUIREMENTS FOR GYNAECOLOGICAL (CERVICAL)
CYTOLOGY
(Second Edition 2014)
NPAAC Tier 4 Document
Print ISBN: 978-1-74186-004-7
Online ISBN: 978-1-74186-005-4
Publications approval number: 10207
Paper-based publications
© Commonwealth of Australia 2014
This work is copyright. You may reproduce the whole or part of this work in unaltered form for
your own personal use or, if you are part of an organisation, for internal use within your
organisation, but only if you or your organisation do not use the reproduction for any commercial
purpose and retain this copyright notice and all disclaimer notices as part of that reproduction.
Apart from rights to use as permitted by the Copyright Act 1968 or allowed by this copyright
notice, all other rights are reserved and you are not allowed to reproduce the whole or any part of
this work in any way (electronic or otherwise) without first being given the specific written
permission from the Commonwealth to do so. Requests and inquiries concerning reproduction and
rights are to be sent to the Online, Services and External Relations Branch, Department of Health,
GPO Box 9848, Canberra ACT 2601, or via e-mail to copyright@health.gov.au.
Internet sites
© Commonwealth of Australia 2014
This work is copyright. You may download, display, print and reproduce the whole or part of this
work in unaltered form for your own personal use or, if you are part of an organisation, for internal
use within your organisation, but only if you or your organisation do not use the reproduction for
any commercial purpose and retain this copyright notice and all disclaimer notices as part of that
reproduction. Apart from rights to use as permitted by the Copyright Act 1968 or allowed by this
copyright notice, all other rights are reserved and you are not allowed to reproduce the whole or any
part of this work in any way (electronic or otherwise) without first being given the specific written
permission from the Commonwealth to do so. Requests and inquiries concerning reproduction and
rights are to be sent to the Online, Services and External Relations Branch, Department of Health,
GPO Box 9848, Canberra ACT 2601, or via e-mail to copyright@health.gov.au.
First published 2006
Second edition 2014
(reprinted with revisions and combining Requirements for
Gynaecological (Cervical) Cytology and Guidelines for the use of
Liquid Based Collection Systems and Semi-Automated Screening Devices in
the Practice of Gynaecological (Cervical) Cytology
Australian Government Department of Health
Contents
Scope............................................................................................................................................. 3
Abbreviations .............................................................................................................................. 4
Definitions .................................................................................................................................... 4
Introduction ................................................................................................................................. 5
1.
Staff ..................................................................................................................................... 6
Pathologists.......................................................................................................................... 6
Scientific and technical staff ............................................................................................... 7
Staff establishment .............................................................................................................. 7
Education ............................................................................................................................. 8
2.
Facilities .............................................................................................................................. 8
3.
Specimens ........................................................................................................................... 8
Adequacy ............................................................................................................................. 8
Retention.............................................................................................................................. 8
4.
Quality assessment............................................................................................................. 8
5.
Reporting ............................................................................................................................ 9
Appendix A
Australian Modified Bethesda System 2004 (AMBS 2004) (Normative)10
Appendix B
Cytology Code Schedule (Informative)...................................................... 16
Appendix C
Summary of guidelines for the Management of Asymptomatic Women with
Screen Detected Abnormalities (Informative) .............................................................. 19
Bibliography .............................................................................................................................. 31
Acknowledgements ................................................................................................................... 18
Further information.................................................................................................................. 18
The National Pathology Accreditation Advisory Council (NPAAC) was established in 1979 to
consider and make recommendations to the Australian, state and territory governments on matters
related to the accreditation of pathology Laboratories and the introduction and maintenance of
uniform Standards of practice in pathology Laboratories throughout Australia. A function of
NPAAC is to formulate Standards and initiate and promote guidelines and education programs
about pathology tests.
Publications produced by NPAAC are issued as accreditation material to provide guidance to
Laboratories and accrediting agencies about minimum Standards considered acceptable for good
Laboratory practice.
Failure to meet these minimum Standards may pose a risk to public health and patient safety.
Scope
The Requirements for Gynaecological (Cervical) Cytology is a Tier 4 NPAAC document and must
be read in conjunction with the Tier 2 document Requirements for Medical Pathology Services.
The latter is the overarching document broadly outlining standards for good medical pathology
practice where the primary consideration is patient welfare, and where the needs and expectations
of patients, Laboratory staff and referrers (both for pathology requests and inter-Laboratory
referrals) are safely and satisfactorily met in a timely manner.
Whilst there must be adherence to all the Requirements in the Tier 2 document, reference to
specific Standards in that document are provided for assistance under the headings in this
document.
The Requirements for Gynaecological (Cervical) Cytology sets out the Standards for using
conventional methods as well as Liquid Based Collection Systems and Semi-Automated Screening
Devices. While the main workload of lower female genital tract cytology reporting relates to the
cervix, the Standards set forth in this document are applicable also to Specimens collected from the
cervical vault post-hysterectomy and from the vagina.
Abbreviations
AIS
AS
CIN
HPV
HSIL
LSIL
NATA
NHMRC
NPAAC
QAP
RCPA
RCPA QAP
Adenocarcinoma in situ
Australian Standard
Cervical intraepithelial neoplasia
Human Papillomavirus
High grade squamous intraepithelial lesion
Low grade squamous intraepithelial lesion
National Association of Testing Authorities, Australia
National Health and Medical Research Council
National Pathology Accreditation Advisory Council
Quality Assurance Program
Royal College of Pathologists of Australasia
Royal College of Pathologists of Australasia Quality Assurance
Program
Definitions
Abnormal report
Cytologist
Negative Specimen
Non-screening
(diagnostic)
Requirements for
Medical Pathology
Services (RMPS)
means those reports including all technically satisfactory reports
which were not negative
means a person holding a qualification which designates
competency in cytology
means those Specimens in which no abnormal cells were detected
plus smears in which benign reactive and/or inflammatory cellular
change was reported. Reports of atypia and/or HPV effect are not
considered negative
means a diagnostic test that is used to classify people as having or
not having disease, where there is an indication disease may be
present e.g. signs (visually abnormal cervix, etc.) or symptoms
(abnormal bleeding, excess pain, etc.). This classification is also
used for specific tests taken after treatment to ensure effectiveness
of treatment
means the overarching document broadly outlining standards for
good medical pathology practice where the primary consideration
is patient welfare, and where the needs and expectations of
patients, Laboratory staff and referrers (both for pathology requests
and inter-Laboratory referrals) are safely and satisfactorily met in a
timely manner.
The standard headings are set out below –
Standard 1 – Ethical Practice
Standard 2 – Governance
Standard 3 – Quality Management
Standard 4 – Personnel
Standard 5 – Facilities and Equipment
A – Premises
B – Equipment
Standard 6 – Request-Test-Report Cycle
A – Pre-Analytical
B – Analytical
C – Post-Analytical
Standard 7 – Quality Assurance
Scientist
Screening
Specimen
Senior Cytologist
means the same as the definition in the NPAAC Requirements for
the Supervision of Pathology Laboratories.
means testing of apparently healthy people who are at risk of
developing a certain disease. Screening tests can predict the
likelihood of someone having or developing a particular disease.
means any tissue or fluid from a patient that is submitted to the
Pathology Service for testing.
means a person having the equivalent of 5 years full-time
experience in cytology and holding a qualification which
designates competence in cytology.
Introduction
This document, Requirements for Gynaecological (Cervical) Cytology, together with the
Requirements for Medical Pathology Services, sets out the minimum requirements for best
practice in relation to the operation of gynaecological cytology services.
This document combines the previous two documents Requirements for Gynaecological (Cervical)
Cytology and Guidelines for the use of Liquid Based Collection Systems and Semi-Automated
Screening Devices in the Practice of Gynaecological (Cervical) Cytology. Many Laboratories
report cervical cytology using conventional as well as liquid based methods and the Standards that
pertain to each of those methods have much in common.
These requirements should be regarded as minimum acceptable Standards for good laboratory
practice. Good administration, adequate staff with appropriate qualifications and training in
gynaecological cytology, and internal quality assurance procedures are important requirements
for achieving the required level of laboratory service.
The performance standards for Laboratories reporting cervical cytology previously managed by the
National Cervical Screening Program are now addressed in the NPAAC Requirements for
Gynaecological (Cervical) Cytology and Performance Measures for Australian Laboratories
Reporting Cervical Cytology.
This document must be read within the national pathology accreditation framework including the
current versions of the following NPAAC documents:
Tier 2 Document
Requirements for Medical Pathology Services
All Tier 3 Documents
Tier 4 Document
Performance Measures for Australian Laboratories Reporting Cervical Cytology
In addition to these Standards, Laboratories must comply with all relevant state and territory
legislation (including any reporting requirements).
In each section of this document, points deemed important for practice are identified as either
‘Standards’ or ‘Commentaries’.
A Standard is the minimum requirement for a procedure, method, staffing resource or
facility that is required before a Laboratory can attain accreditation — Standards are printed
in bold type and prefaced with an ‘S’ (e.g. S2.2). The use of the word ‘must’ in each
Standard within this document indicates a mandatory requirement.
A Commentary is provided to give clarification to the Standards as well as to provide
examples and guidance on interpretation. Commentaries are prefaced with a ‘C’ (e.g. C1.2)
and are placed where they add the most value. Commentaries may be normative or
informative depending on both the content and the context of whether they are associated
with a Standard or not. Note that when Comments are expanding on a Standard or referring
to other legislation, they assume the same status and importance as the Standards to which
they are attached. Where a Commentary contains the word ‘must’ then that Commentary is
considered to be normative.
Please note that any Appendices attached to this document may be either normative or
informative and should be considered to be an integral part of this document.
All NPAAC documents can be accessed at NPAAC Website
While this document is for use in the accreditation process, comments from users would be
appreciated and can be directed to:
The Secretary
NPAAC Secretariat
Department of Health
GPO Box 9848 (MDP 951)
CANBERRA ACT 2601
Phone:
+61 2 6289 4017
Fax:
+61 2 6289 4028
Email:
npaac@health.gov.au
Website:
NPAAC Website
1.
Staff
(Refer to Standard 4 in Requirements for Medical Pathology Services)
Pathologists
S1.1 A pathologist involved in gynaecological cytology must be competent in cytology and
histology of gynaecological Specimens and possess documentary evidence of
appropriate training and experience in this field.
S1.2
To maintain competence, as a minimum, the pathologist must see either 20 abnormal
smears per month or 60 abnormal smears per quarter. If the number of abnormal
cases reported by a pathologist is insufficient, the pathologist must take part in
documented supplementary activities designed to maintain competence.#
C1.2 Where pathologists perform primary screening of cervical smears, these shall only be
performed by pathologists who have appropriate training or have completed an
approved course. Competency in primary screening must be demonstrated.
Scientific and technical staff
S1.3 Where scientific and technical staff are employed for screening gynaecological smears,
the screening must be supervised by at least one (1) appropriately qualified and
trained pathologist, scientist or senior cytologist.
S1.4
Screening staff must either be scientists or cytologists who hold qualifications which
designate competence in cytology or appropriately supervised trainees in cytology.
Staff establishment
S1.5 The maximum workload for any person involved in primary screening is 70 slides per
day. Where an individual undertakes duties in addition to primary screening, or is
employed part time, the maximum rate when screening should not exceed 10 slides per
hour.
C1.5(i)
Persons screening smears must not exceed this Standard regardless of the number
of sites at which they are employed
C1.5(ii) These limits are NOT a recommended optimal or average workload and must
NOT be employed as a performance target for each screener.
S1.6
The maximum workload for any person reporting using semi-automated imaging
techniques must not exceed 150 slides per day.
C1.6(i) Persons screening smears must NOT exceed this Standard regardless of the
number of sites at which they are employed
C1.6(ii) These limits are NOT a recommended optimal or average workload and must
NOT be employed as a performance target for each screener.
S1.7
A pathologist who is competent in gynaecological (cervical) cytology must be available
on site to consult with and advise scientific staff and consult with clinicians.
C1.7
There must be ready access to an adequate conference microscope Facility
enabling simultaneous viewing, discussion and diagnosis by more than one
observer.
For the purpose of this requirement abnormal will include: Squamous abnormalities – possible low grade squamous
intraepithelial lesion; low-grade squamous intraepithelial lesion; possible high-grade squamous lesion; squamous cell
carcinoma; Glandular abnormalities – atypical endocervical cells of undetermined significance; atypical glandular cells of
undetermined significance; possible high-grade glandular lesion; endocervical adenocarcinoma in situ; adenocarcinoma.
These may be derived from supplementary educational material and/or a system of slide exchange with other laboratories.
#
Education
S1.8 Pathologists or scientists involved with the use of liquid based collection systems must
retain documentation confirming they have undertaken continued training specific to
the use of liquid based collection systems and semi-automated devices being employed
within the Laboratory for the preparation and screening of gynaecological slides.
2.
Facilities
(Refer to Standard 5A in Requirements for Medical Pathology Services)
S2.1
Any processing, evaluation and reporting of cytology smears must be in premises
accredited by NATA/RCPA or equivalent.
3.
Specimens
(Refer to Standard 6A in Requirements for Medical Pathology Services)
Adequacy
S3.1
Advice must be available for procedures on taking satisfactory cervical and vaginal
smears for gynaecological cytology. The Laboratory must have information available
on the general principles of taking cervical and vaginal Specimens.
S3.2
Instructions for the taking of liquid based samples for cervical gynaecological
Specimens must make reference to the recommendations for Specimen collection
issued by the suppliers of sampling devices.
S3.3
Instructions must include adherence to expiry dates of any media used, and to storage
and transport procedures recommended by the suppliers of media.
Retention
S3.4
The residual liquid based cytology sample must be retained for a period of at least one
month.
4.
Quality assessment
(Refer to Standard 7 in Requirements for Medical Pathology Services)
S4.1
Records must be kept of results, which allow separate identification of the results
obtained using conventional cytology, new technologies or combination of technologies
to ensure aggregated data can be determined for each methodology used.
S4.2
Each Laboratory must document its procedures for internal audit which cover all its
activities including:
a) a system of follow-up for correlating the results of gynaecological cytology with
relevant histopathology
b) a system within the Laboratory for monitoring the performance of the
Laboratory as a whole and also the performance of individual screeners and
pathologists
c) a review of past negative cytology smears from patients with current abnormal
cytology/histology
d) a system for secondary screening of negative cervical Specimens, (e.g. targeted
re-screening or rapid re-screening).
C4.2
Each of these activities must be regularly monitored and the results or outcomes
recorded.
5.
Reporting
(Refer to Standard 6C in Requirements for Medical Pathology Services)
S5.1
The content and format of the cytology report must comply with the Australian
Modified Bethesda System (AMBS 2004) (see Appendix A).
S5.2
Laboratories must provide results to the cervical cytology registries for all patients
whose test request shows that they have not opted off, in the required format (see
Appendix B) in accordance with relevant jurisdictional requirements.
S5.3
The report must specify if liquid based collection systems and/or semi-automated
instruments have been used and identify the technologies used in generating the result.
S5.4
The report must provide results, interpretation and recommendations.
The recommendations must either be consistent with the NHMRC Publication
Screening to Prevent Cervical Cancer: Guidelines for the Management of Asymptomatic
Women with Screen Detected Abnormalities or be appropriate to the specific clinical
circumstances for that patient where the NHMRC Guidelines might not be directly
applicable (see Appendix C).
C5.4
“However, while the guidelines are based on good population data, it is important
to note that they are only a guide to clinical practice. Clinicians must make
individual decisions in consultation with their patients based on individual clinical
circumstances. The Royal Australian and New Zealand College of Obstetricians
and Gynaecologists has issued management guidelines for women with
intermenstrual and postcoital bleeding (RANZCOG 2002), which take precedence
over these guidelines for such cases”. (Abstract from the foreword of the NHMRC
document.)
S5.5
All cytological reports indicating a cellular abnormality must be confirmed by a
pathologist.
S5.6
Ninety (90) per cent of cervical cytology Specimens must be reported within ten (10)
working days of their receipt by the Laboratory.
S5.7
Laboratories must provide smear-takers with a summary of Specimen results at least
annually. Such a summary is to include the numbers and proportions of
unsatisfactory smears and those with an endocervical component.
Appendix A
Australian Modified Bethesda System
2004 (AMBS 2004) (Normative)
Abstracted from Chapter 4 (Terminology),
Screening to Prevent Cervical Cancer: Guidelines for the Management of Asymptomatic
Women with Screen Detected Abnormalities.
NHMRC 2005.
4.1 Background
In 1991, the United States National Cancer Institute (NCI) sponsored a multidisciplinary meeting
in Bethesda, Maryland to consider Pap smear terminology. Pathologists, cytotechnologists,
gynaecologists and family practitioners, predominantly from the United States but also from other
countries, participated in the workshop. The participants agreed on a consistent system for
reporting Pap smears, The Bethesda System 1991 (TBS 1991).
Problems with TBS 1991
TBS 1991 had three major problems. First, the three-tier system for assessing whether or not a
smear was satisfactory meant that Pap smears could be designated as ‘satisfactory’, ‘satisfactory
but limited by …’, or ‘unsatisfactory’. The category of ‘satisfactory but limited by …’ created
substantial difficulties in the United States by forcing clinicians to treat these smears as
unsatisfactory, resulting in a large number of early repeat smears.
Second, TBS 1991 did not formally recognise adenocarcinoma in situ (AIS). These cases were
placed in a category of ‘atypical glandular cells of undetermined significance’ (AGUS),
together with cases in which much less atypia was observed in glandular cells. It is now
regarded as unsafe to include smears that show evidence of AIS under this heading, since most
smears in this category require less aggressive follow-up than AIS smears.
Third, the heading ‘atypical squamous cells of undetermined significance’ (ASCUS) included
possible high-grade abnormalities together with a much larger number of cases of possible lowgrade abnormalities. The follow-up of women in whom a high-grade lesion is suspected but cannot
be confidently predicted on the basis of a Pap test needs to be more aggressive than the follow-up
of women whose smears show changes suggesting the possibility of a low-grade abnormality.
NHMRC-endorsed Australian terminology
As part of preparing the first National Health and Medical Research Council guidelines for the
management of women with screen-detected abnormalities (NHMRC 1994), the Australian
working party considered the Bethesda terminology and recommended a range of modifications
to overcome the three major problems outlined above. This resulted in a unique Australian
terminology system.
Revised Bethesda System (TBS 2001)
In 2001, the NCI reviewed TBS terminology and a number of changes were made to overcome the
previous problems, bringing the system closer to the NHMRC-endorsed reporting system
developed in Australia (Solomon and Nayer 2004).
TBS 2001 includes a two-tiered classification in relation to whether or not Pap smears are
satisfactory, and a category that accommodates a definite prediction of AIS. Unlike TBS 1991, it
also includes two separate categories for undetermined cases:
when a possible low-grade abnormality is suspected, it is called ‘atypical squamous cells of
undetermined significance’ (ASC-US)
when a possible high-grade lesion is suspected, it is called ‘atypical squamous cells,
possible high-grade lesion’ (ASC-H).
4.2 Australian Modified Bethesda System 2004 (AMBS 2004)
The previous NHMRC-approved Australian terminology (NHMRC 1994) had structural differences
from TBS 2001. The major difference related to the structure of the low-grade abnormalities. This
difference is particularly important because TBS 2001 has been adopted internationally by the
United States and a large number of other countries, and women with low-grade abnormalities are
currently the subjects of a number of clinical trials investigating the optimal management of these
cases. Applicability of international research to the Australian context is exceedingly difficult while
structural differences in terminology systems persist. Finally, the NHMRC Australian terminology
system, which was based on human papillomavirus (HPV)/cervical intraepithelial neoplasia (CIN)
terminology, contained subdivisions between HPV and CIN 1 that are not supported by evidence
that the distinctions are reasonably reproducible (see Section 4.5) or by different clinical outcomes.
After extensive consultation undertaken by the Australian Society of Cytology, with the
introduction of these guidelines, Australia will adopt a revised terminology system, to be known as
the Australian Modified Bethesda System 2004 (AMBS 2004).
In adopting the new Australian terminology, consensus has been reached to accept the
underlying structure of TBS 2001 but to relabel a number of categories. In particular, there was
strong opposition from some to the ‘atypical squamous cells of undetermined significance’
category.
One remaining substantial difference between TBS 2001 and the previous NHMRC-endorsed
terminology related to the structure of the low-grade abnormalities. AMBS 2004 incorporates the
separation of suspected from confidently predicted low-grade abnormalities. AMBS 2004 reflects
a modern understanding of HPV infection, and cervical cancer and its precursors. It is compatible
with terminology systems used internationally and it does not mandate distinctions for which
there is poor evidence for reproducibility or clinical significance.
Note: The AMBS 2004 terminology described here relates only to cervical cytology. Terminology
for reporting cervical tissue specimens (histopathology) remains unchanged.
Therefore, in these guidelines, intraepithelial lesions confirmed histologically will still be
reported according to the CIN terminology and other SNOMED terms.
4.3 Explanation and definition of AMBS 2004 terminology
This section outlines AMBS 2004 terminology. Table 4.1 shows a comparison of AMBS
2004 with the previous NHMRC-endorsed Australian terminology (NHMRC 1994) and
TBS 2001.
Squamous abnormalities
Possible low-grade squamous intraepithelial lesion
The category of possible low-grade squamous intraepithelial lesion is to be used when the reporting
scientist/pathologist observes changes in squamous cells that may represent a low-grade squamous
intraepithelial lesion, but the changes are not so clear-cut as to justify a ‘definite’ diagnosis. This
category specifically excludes changes that are within the scope of reactive processes. It
corresponds to ‘nonspecific minor squamous cell changes’ in the previous Australian NHMRCendorsed terminology (NHMRC 1994).
Low-grade squamous intraepithelial lesion
The low-grade squamous intraepithelial lesion (LSIL) category is the morphological correlate of
productive viral infection. It is to be used when the scientist/pathologist observes changes that
would have been described as ‘HPV effect’ or ‘CIN 1’ in the
previous Australian terminology and represents part of the previous ‘low-grade squamous epithelial
abnormality’ category.
Possible high-grade squamous lesion
The category of possible high-grade squamous lesion is to be used when the reporting
scientist/pathologist suspects the presence of a high-grade squamous abnormality, such as
possible CIN 2, CIN 3 or squamous cell carcinoma (SCC), but the changes are insufficient to
justify a confident cytological prediction of a high-grade lesion. It corresponds to the
‘inconclusive possible high-grade squamous abnormality’ category in the previous Australian
terminology.
High-grade squamous intraepithelial lesion
The high-grade squamous intraepithelial lesion (HSIL) category is the morphological
correlate of a true preneoplastic change occurring in squamous cells as a result of HPV
infection. It is to be used when the scientist/pathologist observes changes that would have
previously been described as CIN 2 or CIN 3. Cases in this category would have accounted
for almost all cases in the ‘high-grade squamous epithelial abnormality’ category in the
previous Australian terminology.
If, in addition to the presence of a definite intraepithelial high-grade abnormality, there are
features that suggest the presence of an invasive component, this should be noted in the ‘specific
diagnosis’ section of the report.
Squamous cell carcinoma
The SCC category is self-explanatory. In the previous Australian terminology, these cases would
have fallen under the heading of ‘high-grade epithelial abnormality’.
Glandular abnormalities
Atypical endocervical cells of undetermined significance Atypical glandular cells of
undetermined significance
These categories encompass those changes in glandular cells that the reporting
scientist/pathologist believes are outside the scope of a definite reactive process. It has been
well documented that productive HPV infection does not exist in glandular cells, and therefore
there is no glandular correlate to the low-grade squamous abnormality.
Nevertheless, the morphological changes observed in glandular cells encompass a spectrum of
changes. These categories should be used when such changes are insufficient to raise the
possibility of a neoplasm, such as AIS, but are beyond those accepted as definitely representing a
reactive process. Cells in this category are to be designated as follows:
atypical glandular cells when the reporting scientist/pathologist is not sure whether the cells
are endocervical
atypical endocervical cells when the reporting scientist/pathologist is confident that the cells
are endocervical.
Possible high-grade glandular lesion
This category is to be used when the reporting scientist/pathologist suspects the presence of a highgrade glandular abnormality such as possible AIS, possible endocervical adenocarcinoma or
possible endometrial adenocarcinoma, but is unable to make a confident prediction. It corresponds
to the ‘inconclusive possible high-grade glandular abnormality’ category in the previous Australian
terminology.
Endocervical adenocarcinoma in situ
The endocervical AIS category is self-explanatory. The diagnosis is to be used when the reporting
scientist/pathologist is confident of the presence of AIS.
Adenocarcinoma
The adenocarcinoma category is self-explanatory. The reporting scientist/ pathologist has the
option of designating whether they believe the adenocarcinoma is endocervical, endometrial or
extrauterine in origin.
Table 4.1 Comparison of the Australian Modified Bethesda System (AMBS 2004) with
previous Australian terminology and The Bethesda System (TBS 2001)
AMBS 2004
Australian
TBS 2001
Incorporates
NHMRC
endorsed
terminology1994
Squamous abnormalities
Possible low-grade
Low grade
squamous
epithelial
intraepithelial lesion abnormality
Atypical
squamous
cells,undetermined
significance
(ASC-US)
Nonspecific
minor squamous
cell changes.
Changes that
suggest but fall
short of HPV/
CIN 1
Low-grade
squamous
intraepithelial lesion
Low-grade
epithelial
abnormality
Low-grade
squamous
intraepithelial
lesion
HPV effect, CIN
1
Possible high-grade
squamous lesion
Inconclusive,
possible highgrade squamous
abnormality
Changes that
suggest, but fall
short of, CIN 2,
CIN 3 or SCC
High-grade
squamous
intraepithelial lesion
High-grade
epithelial
abnormality
Atypical
squamous cells,
possible highgrade lesion
(ASC-H)
High-grade
squamous
intraepithelial
lesion
Squamous cell
carcinoma
High-grade
epithelial
abnormality
Squamous cell
carcinoma
Squamous cell
carcinoma
Glandular abnormalities
Atypical
Low-grade
endocervical cells of epithelial
undetermined
abnormality
significance
Atypical
endocervical cells,
undetermined
significance
Nonspecific
minor cell
changes in
endocervical cells
Atypical glandular
cells of
undetermined
significance
Low-grade
epithelial
abnormality
Atypical glandular
cells,
undetermined
significance
Nonspecific
minor cell
changes in
glandular cells
Possible high-grade
glandular lesion
Inconclusive,
possible highgrade glandular
abnormality
Atypical
endocervical cells,
possibly
neoplastic
Changes that
suggest, but fall
short of, AIS or
adenocarcinoma
Endocervical
adenocarcinoma in
situ
High-grade
epithelial
abnormality
Endocervical
Adenocarcinoma
adenocarcinoma in in situ
situ
CIN 2, CIN 3
Adenocarcinoma
High-grade
epithelial
abnormality
Adenocarcinoma
Adenocarcinoma
4.4 Preparation of cervical cytology reports using AMBS 2004
Cervical cytology reports should contain the following components.
Specimen type and site
Indicate conventional Pap smear versus liquid-based versus other.
Indicate that the specimen is cervical in origin.
In the case of split samples, a single combined report should be issued and this field should
indicate that the report is based on, for example, a conventional Pap smear and a ThinPrep or an
Autocyte Prep sample.
Interpretation/result
This should consist of the appropriate category heading, selected from the section below.
A statement regarding the presence or absence of an endocervical component should be included.
The laboratory may, at its discretion, also include a more specific diagnosis. Some practitioners
have expressed a strong preference that laboratories continue to distinguish between CIN 2 and CIN
3 within the HSIL category (see Section 4.5).
Recommendation
•
Concise management recommendations, as set out in the following sections of these
guidelines, should be included in the report. Explicit reference to these guidelines can be
included in the report.
Categories of results
Unsatisfactory for evaluation (specify reason)
Negative for intraepithelial lesion or malignancy
Organisms
Trichomonas vaginalis
fungal organisms morphologically consistent with Candida spp
shift in flora suggestive of bacterial vaginosis
bacteria morphologically consistent with Actinomyces spp
cellular changes consistent with herpes simplex virus.
Other non-neoplastic findings (optional to report; list not exclusive)
•
reactive cellular changes associated with:
o
inflammation and repair
o
radiation
o
intrauterine contraceptive device
o
o
glandular cells after hysterectomy
atrophy
Epithelial cell abnormalities
Squamous abnormalities:
possible low-grade squamous intraepithelial lesion
low-grade squamous intraepithelial lesion
possible high-grade squamous lesion
high-grade squamous intraepithelial lesion
squamous cell carcinoma.
Glandular abnormalities:
atypical endocervical cells of undetermined significance
atypical glandular cells of undetermined significance
possible high-grade glandular lesion
endocervical adenocarcinoma in situ
adenocarcinoma.
Note: ‘Atypical’ cells are those that deviate from a normal or typical state. In cytology, this
includes any deviation from normal cellular appearances, but conveys no information about
aetiology. Atypical cells may be due to physiological processes such as repair or response to
radiation, or to disease processes such as dysplasia or cancer. The term should therefore not be used
alone, but should be further qualified and accompanied by a clear recommendation for
management.
Examples of reports conforming to the new terminology requirements are presented in Appendix 5
of the full version of Australian Modified Bethesda System 2004.
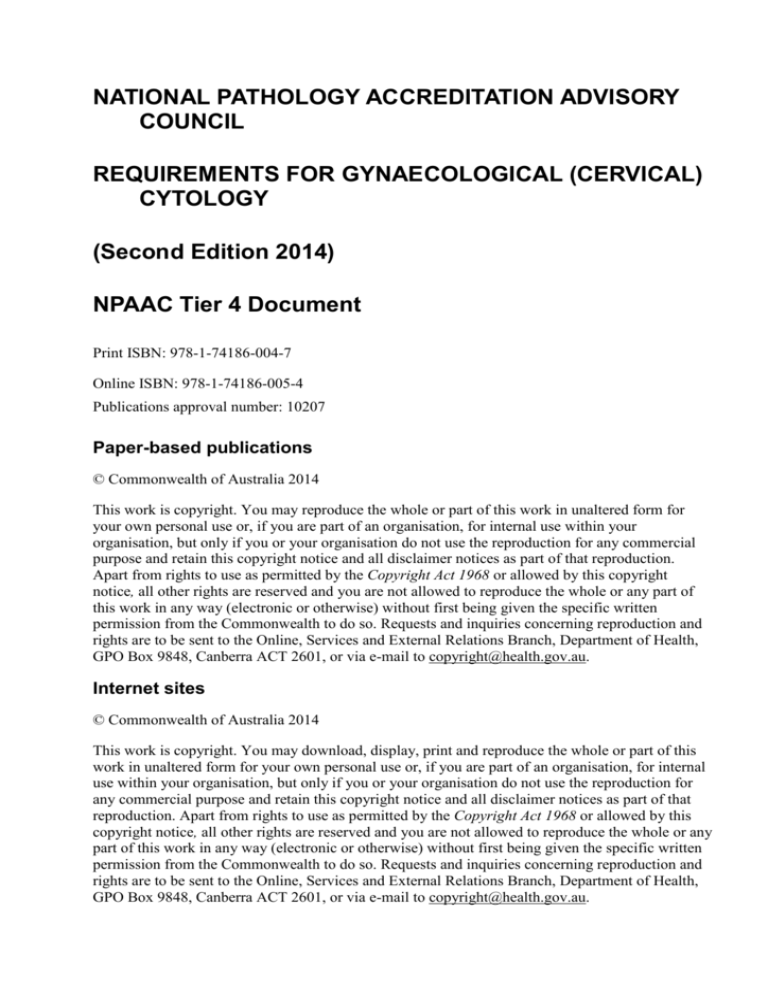
Appendix B Cytology Code Schedule (Informative)
Cytology Code Schedule below is the recommended format to be reported to cervical registries.
Figure 1An Image of the Code Schedule as information should be presented
Appendix C Is a Summary of guidelines for the Management of
Asymptomatic Women with Screen Detected Abnormalities
(Informative)
Abstracted from Screening to Prevent Cervical Cancer: Guidelines for the Management of
Asymptomatic Women with Screen Detected Abnormalities. NHMRC 2005.
Bibliography
0.Australian Modified Bethesda System 2004 (AMBS 2004). Abstracted from Chapter 4
(Terminology) – Screening to Prevent Cervical Cancer: Guidelines for the Management of
Asymptomatic Women with Screen Detected Abnormalities, National Health and Medical Research
Council (NHMRC), Canberra (2005).
Acknowledgements
Professor Yee Khong (Chair)
Associate Professor Chris Carter
Associate Professor Margaret Cummings
Professor Annabelle Farnsworth
Associate Professor Dorota Gertig
Professor Ruth Salom
Dr Paul Shield
Professor Gordon Wright
Members of the NPAAC Document Review & Liaison Committee (DRL)
Members of the National Pathology Accreditation Advisory Council (NPAAC)
Further information
Other NPAAC documents are available from:
NPAAC Secretariat
Primary Care, Diagnostics & Radiation Oncology Branch
Department of Health
GPO Box 9848 (MDP 951)
CANBERRA ACT 2601
Phone:
(02) 6289 4017
Fax:
(02) 6289 4028
Email:
npaac@health.gov.au
Website: NPAAC Website