eSelf-help for AM Protocol
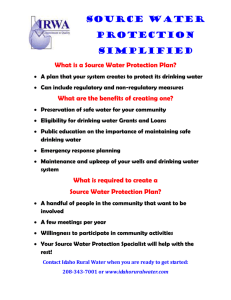
advertisement

Evidence-based Synthesis Program Systematic Review Protocol Project Title: Online Self-help Programs for Alcohol Misuse Investigators: Eric Dedert, PhD; Caroline Freiermuth, PhD; Adam Hemminger; J. Murray McNeil, PhD; Isabel Ross, MD; Roy Stein, MD ESP Investigators: Jennifer McDuffie, PhD; John W. Williams Jr., MD, MHSc ESP Core Staff: Avishek Nagi, Liz Wing Search Librarian: Megan Von Isenburg Nominator: Ken Weingardt, PhD, National Director, Mental Health Web Services Operational Partner: Mental Health Services; Mental Health Services (Daniel R. Kivlahan, PhD, Director, Addictive Disorders); National Center for Prevention (Margaret Dundon, PhD. National Program Manager for Health Behavior) I. Background The economic and health burden of alcohol use disorders is widely recognized,1 as is the need for effective interventions to reduce this burden.2,3 Broad public access to the internet is now a reality, and this has opened many new avenues to reach individuals who misuse alcohol.4 Types of alcohol problems, for the purpose of this review, will be guided by the definitions in Table 1. Table 1. Definitions of the Spectrum of Alcohol Misusea Term Risky or hazardous use Harmful use Alcohol abuse Definition Consumption of alcohol above recommended daily, weekly, or per occasion amounts. Consumption levels that increase the risk for health consequences. A pattern of drinking that is already causing damage to health. The damage may be either physical (e.g., liver damage from chronic drinking) or mental (e.g., depressive episodes secondary to drinking). A maladaptive pattern of alcohol use leading to clinically significant impairment or distress, as manifested by 1 of the following within a 12-month period: Recurrent alcohol use resulting in a failure to fulfill major obligations at work, school, or home (e.g., repeated absences or poor work performance related to alcohol use; alcohol-related absences, suspensions, or expulsions from school; or neglect of children or household) Recurrent alcohol use in situations in which it is physically hazardous (e.g., driving an automobile or operating a machine) Recurrent alcohol-related legal problems (e.g., arrests for alcohol-related disorderly conduct) Continued use despite persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of alcohol (e.g., arguments with spouse about consequences of intoxication or physical fights) (And) the symptoms have never met the criteria for alcohol dependence. 1 Term Alcohol dependence (alcoholism, alcohol addiction) Definition A maladaptive pattern of alcohol use leading to clinically significant impairment or distress, as manifested by 3 of the following at any time in the same 12-month period: Tolerance, as defined by either of the following: o A need for markedly increased amounts of alcohol to achieve intoxication or desired effect o Markedly diminished effect with continued use of the same amount of alcohol Withdrawal, as manifested by either of the following: o The characteristic withdrawal syndrome for alcohol o Alcohol (or a closely related drug) is taken to relieve or avoid withdrawal symptoms Alcohol is often taken in larger amounts or over a longer period than was intended A persistent desire or unsuccessful efforts to cut down or control alcohol use A great deal of time is spent in activities necessary to obtain alcohol, use alcohol, or recover from its effects Important social, occupational, or recreational activities are given up or reduced because of alcohol use Use continues despite knowledge of a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by alcohol (e.g., continued drinking despite recognition that an ulcer was made worse by alcohol consumption) a Reproduced with permission from Jonas DE, Garbutt JC, Amick HR, et al. Behavioral counseling after screening for alcohol misuse in primary care: a systematic review and meta-analysis for the U.S. Preventive Services Task Force. Ann Intern Med. 2012;157(9):645-54. Meta-analyses have shown that face-to-face screening and brief interventions (SBIs) are effective.5-7 The wide use of SBIs is hampered, however, by barriers such as adequate funding, time, and adequately trained personnel.8,9 On the other hand, self-help for problem drinking provided over the internet (i.e., electronic self-help or e-self-help) may prove to be a useful extension of the reach of SBIs. E-self-help is available in brief and longer forms. Single-session, electronic, personalized normative feedback is one type of brief intervention for problem drinking available over the internet. Feedback is provided on the individual’s alcohol consumption in relation to recommended guidelines for low-risk drinking behavior in a relevant age and sex cohort.10 Such comparison of the individual’s drinking pattern to their peer group could help them to realize they have a problem and seek further help.11 More extended forms of e-self-help are also available and are based on behavioral self-control, cognitive behavioral therapy (CBT), motivational interviewing, or a combination of these models.12-14 It is recommended that these extended interventions be used for up to 6 weeks to initiate a change in drinking behavior.15 E-self-help interventions have the potential to reach individuals with drinking problems who wish to remain anonymous, have little time for traditional therapy, need therapy to be available during nonstandard business hours due to shift work, live at a great distance from traditional therapy, or cannot afford such therapy.16,17 This is especially true of “no-contact” interventions; i.e., those in which participants work through the intervention without contact with a mental health professional.18,19 2 Most studies evaluating the efficacy of e-self-help programs have been conducted in college students.20-22 Generally, these studies have found that e-self-help has a favorable impact on problem drinking among youth. Studies evaluating the efficacy of e-self-help programs among adult, noncollegiate populations are fewer in number, but show promising results as well.23 However, to date, there are no such studies evaluating the efficacy of these programs in Veterans24 and current reviews in the non-college student population are out of date. Given that Veterans can encounter most if not all of the barriers to accessing care for problem drinking listed above, e-self-help may prove to be a promising avenue, especially for the younger, more internet-savvy Veterans returning from OIF/OEF. The VA/DoD Integrated Mental Health Strategy consists of a series of 28 Strategic Actions designed to help both agencies better meet the unique mental health needs of OIF/OEF Veterans. One of these strategic actions resulted in the creation of a series of web-based self-help programs. The purpose of this report is to conduct a systematic review of randomized controlled trials assessing CD-based, web-based, and mobile applications of e-self-help for problem drinking. We will evaluate these studies for changes in alcohol consumption and effects on the medical health and social and legal consequences of problem drinking. This evidence synthesis will be used to inform the decision about whether to implement e-self-help for alcohol misuse, and how best to implement these programs. Project Timeline: Kickoff call: October 30, 2013 Project start: November 7, 2013 Anticipated draft report due: June 6, 2014 Anticipated final report submitted: July 31, 2014 II. Key Questions The key research questions for this systematic review were developed after a topic refinement process that included a preliminary review of published, peer-reviewed literature; consultation with internal partners and investigators; and consultation with content experts and key VA stakeholders. During the topic refinement process, the scope of this review was narrowed to focus on alcohol misuse and alcohol use disorder. This study protocol was reviewed by a broader group, including representatives from Mental Health Web Services (Ken Weingardt), Mental Health Services (Daniel Kivlahan), and National Center for Prevention (Margaret Dundon). The key questions (KQs) for this systematic review are: KQ 1: For electronic self-help (e-self-help) interventions targeting adults who misuse alcohol or who have a diagnosis of alcohol use disorder (AUD), what level, type, and modality of user support is provided (e.g., daily telephone calls, weekly email correspondence), by whom (e.g., professional counselor, technical support staff); and in what clinical context (adjunct to therapy or primary intervention)? KQ 2: For adults who misuse alcohol but do not meet diagnostic criteria for AUD, what are the effects of e-self-help interventions compared with inactive controls? 3 KQ 3: For adults at high risk for AUD (e.g., AUDIT-C >8), or who have a diagnosis of AUD, what are the effects of e-self-help interventions compared with inactive controls? KQ 4: For adults who misuse alcohol, are at high risk for AUD, or who have a diagnosis of AUD, what are the effects of e-self-help interventions alone or used in combination with face-toface therapy compared with face-to-face therapy alone? A. Population The population will be adults (age 18 years and older) across the spectrum of risk related to alcohol misuse, ranging from risky or hazardous use to severe AUD. We will take care to consider the type of assessment used for alcohol misuse and the differences in standards for alcohol consumption between countries. For KQ 1 and KQ 2, anyone with a positive AUDIT-C or equivalent using established thresholds but who have not been assessed for or diagnosed with an AUD. For KQ 1, KQ 3 and KQ 4, anyone with an AUDIT-C or equivalent who score above a threshold that is associated with a high risk for AUD (e.g., AUDIT-C ≥8), or with a diagnosis of AUD. We will include studies that enroll patients with dual diagnosis (e.g., depression and alcohol use) or dual substance abuse (e.g. ETOH and other SUD) as these studies are relevant to the Veteran population. We will exclude studies that enroll pregnant women, but will identify any studies in this population, so that stakeholders will have information on the number of studies conducted in this population. B. Intervention The intervention may be designed for self-guided treatment or with the support of a clinician, but it must be a therapy delivered primarily by a computer-based mechanism or as an adjunct to therapy, as follows: Delivery mode: CD-ROM, web-based, interactive voice response (IVR) and electronic devices including mobile phones (e.g., text messaging) and “Health Buddy.” Treatment model: We will include all interventions derived from evidence-based therapeutic models designed to reduce alcohol use. Evidence-based therapeutic models include brief motivational interviewing, CBT, behavioral self-control, and 12-step programs. We will exclude interventions based on psychodynamic or family therapy and therapies that are not targeted at an individual (e.g., parent–child dyads). KQ 4 includes e-self-help interventions used in combination with face-to-face therapy. For these studies, the computer-based intervention may be as simple as computer-based self-monitoring. Treatment phase: The intervention is designed for treatment, not primary prevention. An example of an intervention that does not meet these criteria is: computerized screening only without any computer-based treatment component. 4 C. Comparators A list of the acceptable comparators follows, with the key idea being that we must be able to isolate the effect of the e-self-help intervention from the comparator intervention: KQ 1: Descriptive, no comparator KQ 2 and KQ 3: Usual care, waitlist control, and information or attention control KQ 4: Face-to-face therapy D. Outcomes Adherence to the intervention (e.g., number of planned sessions completed, proportion completing the planned intervention) Effects on alcohol consumption patterns such as standard drinks/week, heavy drinking episodes, and achieved recommended drinking limits Effects on associated health problems such as mortality, alcohol-related liver problems, alcohol-related accidents (motor vehicle accidents or injuries) Legal problems such as assault, battery, child abuse, or resisting or obstructing an officer Medical utilization such as emergency department visits or hospital admissions (number of admissions, hospital days) related to the disorder being treated Effects on validated functional status measures of global or mental health functioning such as SF-36, Sheehan Disability Scale Adverse effects such as onset of or increase in illegal substance use, smoking, anxiety, interference with the physician-patient relationship E. Timing Follow-up is measured at 6 months or greater following randomization. F. Settings Patients may be identified from general medical (including emergency departments), mental health, or community populations. Patients do not have to be engaged in treatment with a clinician and may be identified through self-assessments without a definitive clinical diagnosis. 5 III. Analytic Framework: IV. Methods A. Criteria for inclusion and exclusion of studies in this systematic review Inclusion criteria Study design: RCTs with N ≥50. The sample size requirement is designed to exclude small pilot studies that typically are underpowered and have more methodological problems than larger trials. Studies with small samples sizes and no treatment effect are also less likely to be published than those finding a treatment effect, increasing the risk of publication bias. However, we will track citations excluded due to n<50 at the request of our stakeholders. Adults aged 18 years or older with alcohol misuse (KQ2), at high risk of AUD or diagnosis of AUD (KQ3). Outpatients in any setting (general medical setting, emergency department, and community or patients not engaged in clinical care who are enrolled through selfassessments). We will include studies where patients are enrolled during a hospitalization if the majority of the intervention is delivered on an outpatient basis. Intervention must be a computer-based therapy adhering to evidence-based treatment principles and used for individually delivered treatment. Examples of interventions that do not meet the intervention criteria are interventions designed for primary prevention; interventions that are primarily telemedicine-based (e.g., therapy via video chat or 6 telephone interactions); disease management interventions where treatment for alcohol misuse is only one component of a more comprehensive intervention; interventions targeted at dyads (e.g. parent-child); and therapies that are delivered primarily in face-toface encounters with only minor computerized supplementation (e.g., limited text messages or online materials that are purely informational). In addition, we will exclude interventions that utilize computerized screening, but do not use a computerized component for treatment. The comparator for KQ 2 and KQ 3 is usual care not involving psychotherapy; waitlist; information or attention control. For KQ 4, the comparator is face-to-face treatment. Study must report effects on at least one of the following relevant outcomes at least 6 months after randomization and initiation of intervention: o Alcohol consumption patterns o Associated health problems (e.g., mortality, alcohol-related liver disease) o Legal problems o Medical utilization (e.g., emergency department visits or hospital admissions related to the disorder being treated) o Validated functional status measures of global or mental health functioning (e.g., SF-36, Sheehan Disability Scale) o Adverse effects (e.g., illegal substance use, smoking, anxiety, interference with the physician-patient relationship) Article is a full publication in a peer-reviewed journal. Examples of reports that are not included are meeting abstracts and dissertations. Article is an English-language publication. Study is conducted in North America, Western Europe, Australia/New Zealand (rationale is to include economically developed countries with sufficient similarities in health care system and culture to be applicable to U.S. medical care). Studies are conducted since 2000 (rationale is that brief interventions emerged in the 1980s, personal computers in the early 1980s, and the internet in the 1990s). Based on our assessment of studies included in existing systematic reviews, the earliest relevant publication was in 2004. Exclusion criteria Not an English-language publication Inpatient settings 7 B. Literature search strategies We will conduct a primary search of MEDLINE® (via PubMed®), the Cochrane Registry, Embase®, and PsycINFO from 2000 to present. We will further evaluate the bibliographies of systematic or nonsystematic reviews for relevant studies. We anticipate using a combination of MeSH keywords and selected free-text terms to search titles and abstracts. To ensure completeness, search strategies will be developed in consultation with a master librarian. To assess for publication bias, we will search ClinicalTrials.gov to identify completed but unpublished studies meeting our eligibility criteria, an indicator of possible publication bias. Using prespecified inclusion/exclusion criteria, titles and abstracts of articles included in the existing reviews and identified through our primary search will be reviewed by two reviewers for potential relevance to the KQs. Articles included by either reviewer will undergo full-text screening. At the full-text screening stage, two independent reviewers must agree on a final inclusion/exclusion decision. Articles meeting eligibility criteria will be included for data abstraction. All results will be tracked in both DistillerSR, a web-based data synthesis software program (Evidence Partners Inc., Manotick, ON, Canada), and EndNote® reference management software (Thomson Reuters). C. Data abstraction and data management Data from published reports will be abstracted into a customized DistillerSR database by one reviewer and overread by a second reviewer. Disagreements will be resolved by consensus or by obtaining a third reviewer’s opinion when consensus cannot be reached. Data elements include descriptors to assess applicability, quality elements, intervention/exposure details, and outcomes. Key characteristics abstracted will include patient descriptors (including age, gender, race, education, and experience with therapy), setting, features and dose of the computer-assisted intervention, features of the comparator, and outcomes as described previously. We will place special emphasis on describing the key components of the intervention including the modes and intensity of support, the clinical discipline and training of the interventionist, the clinical context, and the intervention dose. Multiple reports from a single study will be treated as a single data point. When critical data are missing or are unclear in published reports, we plan to request supplemental data from the study authors. Key features relevant to applicability include the match between the sample and target populations (e.g., comorbidity, age, education level) and the training and experience of the clinician. D. Assessment of methodological quality of individual studies Quality assessment will be performed by the researcher abstracting or evaluating the included article; this initial assessment will then be overread by a second, highly experienced reviewer. Disagreements will be resolved between the two reviewers or when needed by arbitration from a third reviewer. We will use the key quality criteria described in the Agency for Healthcare Research and Quality’s (AHRQ’s) “Methods Guide for Effectiveness and Comparative Effectiveness Reviews”25 adapted to this specific topic and customized to RCTs. For RCTs, these criteria 8 are adequacy of randomization and allocation concealment, the comparability of groups at baseline, blinding, the completeness of followup and differential loss to followup, whether incomplete data were addressed appropriately, the validity of outcome measures, and conflict of interest. We will assign a summary quality score (good, fair, or poor) to individual studies. E. Data synthesis We will summarize the primary literature by abstracting relevant data. We will develop a summary table describing the key outcomes and the types of study designs used to evaluate computer-based alcohol interventions. We will then determine the feasibility of completing a quantitative synthesis (i.e., meta-analysis) to estimate summary effects. Feasibility depends on the volume of relevant literature, conceptual homogeneity of the studies, and completeness of results reporting. We will aggregate outcomes when there are at least three studies with the same outcome, based on the rationale that one or two studies do not provide adequate evidence for summary effects. If meta-analyses are feasible, we will explore the possibility of subgroup analyses to explore the consistency of effects across conditions (e.g., mild severity of alcohol misuse vs. moderate-severe alcohol misuse). Analyses will be conducted separately for intervention vs. inactive control, interventions using computerized alcohol treatment as an adjunct to face-to-face therapy vs. face-to-face therapy, and interventions comparing two different intensities or levels of clinical support for computerized therapy. We will stratify analyses for effects on alcohol use into the following groups: college students, adults, and older adults. We will also conduct subgroup analyses and meta-regression analyses to examine effects of key intervention components. We recognize that subgroup analyses involve indirect comparisons (across studies) and are subject to confounding. These moderator analyses will evaluate the effects of: intervention dose, level of clinical support, and commercially available versus non-commercially available programs. Results of these moderator analyses will be interpreted cautiously and be considered hypothesis generating. For other variables of interest (e.g., gender) that are not amenable to valid subgroup comparisons as part of our meta-analyses, we will abstract subgroup analyses from the primary studies and conduct a qualitative synthesis of these findings. We anticipate that studies may report both dichotomous outcomes (e.g., proportion achieving a prespecified treatment response) and continuous outcomes (e.g., change in drinks per week). If quantitative synthesis is possible, dichotomous outcomes will be combined using risk ratio or odds ratio, and continuous outcomes will be combined using mean differences in a random-effects model. Since symptom scales are likely to vary across studies, we anticipate using the standardized mean difference (Hedges g) for continuous outcomes. Change in symptoms is often measured by both self- and interviewer-administered scales. When studies report more than one measure of symptom response (e.g., self-report of alcohol consumption and self-report of alcohol-related consequences), we will use the mean effect of the two outcome measures. We will explore potential sources of heterogeneity including the specific mental illness, symptom severity, the context of the intervention (e.g., therapy as an adjunct vs. computer-based therapy as the primary intervention but in a clinical context vs. computer aided therapy without other clinical care), comfort with computers (or age as a proxy), and the comparator (e.g., waitlist control vs. more active control). We will evaluate for statistical heterogeneity using visual inspection and Cochrane’s Q and I2 statistics. Publication bias will 9 be assessed using findings from the ClinicalTrials.gov search (described previously) and using funnel plots (when there are >10 studies in an analysis). If a quantitative synthesis is not feasible, we will analyze the data qualitatively. We will give more weight to the evidence from higher quality studies with more precise estimates of effect. A qualitative synthesis would focus on documenting and identifying patterns in efficacy and safety of the intervention across conditions and outcome categories. We will analyze potential reasons for inconsistency in treatment effects across studies by evaluating differences in the study population, intervention, comparator, and outcome definitions. F. Grading the evidence for each key question The strength of evidence for each key question will be assessed using the approach described in AHRQ’s “Methods Guide.”25 In brief, this approach requires assessment of four domains: risk of bias, consistency, directness, and precision. Additional domains are to be used when appropriate: coherence, dose-response association, impact of plausible residual confounders, strength of association (magnitude of effect), and publication bias. These domains will be considered qualitatively, and a summary rating will be assigned after discussion by two reviewers as high, moderate, or low strength of evidence. In some cases, high, moderate, or low ratings will be impossible or imprudent to make. In these situations, a grade of insufficient will be assigned. G. References 1. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591-608. 2. Institute of Medicine. Broadening the base of treatment of alcohol problems: Report of a study by a committee of the Institute of Medicine. Washington, DC: National Academies Press. 1990. 3. Cuijpers P, Riper H, Lemmers L. The effects on mortality of brief interventions for problem drinking: a meta-analysis. Addiction. 2004;99(7):839-45. 4. Hester RK, Miller JH. Computer-based tools for diagnosis and treatment of alcohol problems. Alcohol Res Health. 2006;29(1):36-40. 5. Moyer A, Finney JW, Swearingen CE, et al. Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatmentseeking populations. Addiction. 2002;97(3):279-92. 6. Kaner EF, Beyer F, Dickinson HO, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev. 2007(2):CD004148. 7. Wechsler H, Lee JE, Kuo M, et al. Trends in college binge drinking during a period of increased prevention efforts. Findings from 4 Harvard School of Public Health College Alcohol Study surveys: 1993-2001. J Am Coll Health. 2002;50(5):203-17. 8. Nilsen P. Brief alcohol intervention--where to from here? Challenges remain for research and practice. Addiction. 2010;105(6):954-9. 10 9. Williams EC, Johnson ML, Lapham GT, et al. Strategies to implement alcohol screening and brief intervention in primary care settings: a structured literature review. Psychol Addict Behav. 2011;25(2):206-14. 10. Chan KK, Neighbors C, Gilson M, et al. Epidemiological trends in drinking by age and gender: providing normative feedback to adults. Addict Behav. 2007;32(5):967-76. 11. Lapham GT, Hawkins EJ, Chavez LJ, et al. Feedback from recently returned veterans on an anonymous web-based brief alcohol intervention. Addict Sci Clin Pract. 2012;7(1):17. 12. Hester RK. Self-control training. In: Hester RK, Miller WR, editors. Handbook of Alcoholism Treatment Approaches: Effective Alternatives. Needham Heights, MA: Allyn & Bacon. 2003:152-164. 13. Kalden R, Caroll K, Donovan D, et al. Cognitive behavioral coping skillstherapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. In: Mattson M, editor. Mattson MEM, editor. NIAAA Project MATCH Monograph Series. Rockville, MD: National Institute on Alcoholism and Alcohol Abuse. 1992. 14. Miller W, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd edition. New York, NY: Guilford. 2002. 15. Breslin FC, Sobell MB, Sobell LC, et al. Toward a stepped care approach to treating problem drinkers: the predictive utility of within-treatment variables and therapist prognostic ratings. Addiction. 1997;92(11):1479-89. 16. Cunningham JA, Selby PL, Kypri K, et al. Access to the Internet among drinkers, smokers and illicit drug users: is it a barrier to the provision of interventions on the World Wide Web? Med Inform Internet Med. 2006;31(1):53-8. 17. Vernon ML. A review of computer-based alcohol problem services designed for the general public. J Subst Abuse Treat. 2010;38(3):203-11. 18. Riper H, Kramer J, Conijn B, et al. Translating effective web-based self-help for problem drinking into the real world. Alcohol Clin Exp Res. 2009;33(8):1401-8. 19. Bewick BM, Trusler K, Barkham M, et al. The effectiveness of web-based interventions designed to decrease alcohol consumption--a systematic review. Prev Med. 2008;47(1):17-26. 20. Carey KB, Scott-Sheldon LA, Elliott JC, et al. Computer-delivered interventions to reduce college student drinking: a meta-analysis. Addiction. 2009;104(11):1807-19. 21. Carey KB, Scott-Sheldon LA, Elliott JC, et al. Face-to-face versus computer-delivered alcohol interventions for college drinkers: a meta-analytic review, 1998 to 2010. Clin Psychol Rev. 2012;32(8):690-703. 22. Khadjesari Z, Murray E, Hewitt C, et al. Can stand-alone computer-based interventions reduce alcohol consumption? A systematic review. Addiction. 2011;106(2):267-82. 23. Riper H, Spek V, Boon B, et al. Effectiveness of E-self-help interventions for curbing adult problem drinking: a meta-analysis. J Med Internet Res. 2011;13(2):e42. 11 24. Brief DJ, Rubin A, Keane TM, et al. Web intervention for OEF/OIF veterans with problem drinking and PTSD symptoms: a randomized clinical trial. J Consult Clin Psychol. 2013;81(5):890-900. 25. Agency for Healthcare Research and Quality. Methods Guide for Effectiveness and Comparative Effectiveness Reviews. Rockville, MD: Agency for Healthcare Research and Quality. Available at: http://www.effectivehealthcare.ahrq.gov/index.cfm/search-forguides-reviews-and-reports/?pageaction=displayproduct&productid=318. Accessed November 13, 2013. 12