File
advertisement

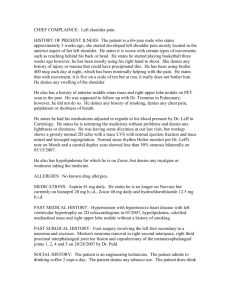
S- Subjective Data: S.U. - new visit, established patient 47 y/o Caucasian male, married History obtained from patient CC: “I’ve had coughing and chest congestion for one month.” HPI: Patient reports experiencing cough and chest congestion for three weeks. Coughing began while at home. Describes cough as productive with minimal white and yellow sputum. States cough is intermittent, worse in the morning when he wakes up and improves throughout the day, but worsens again in the evenings. Aggravating factors include exposure to heat as the patient works outside periodically throughout the day on a daily basis. States he has tried OTC Robitussin DM x 4 days with minimal relief. Denies pain with coughing. Denies any nasal congestion, sore throat, or headache. Denies sinus pain or ear pain. Denies recent travel or exposure to illness. Past Medical History: Medications: Allegra 180 mg PO daily- taking x 2 years for seasonal allergies. Crestor 10 mg PO daily- taking x 5 years for hypercholesterolemia. Prevacid 30 mg delayed-release capsule PO daily- taking x 5 years for GERD. Synthroid 25 mcg PO daily- taking x 9 years for hypothyroidism. Patient denies problems/side effects with any of his medications. States he takes his medications as prescribed on a daily basis. Allergies: Keflex- since 2003, causes rash; Penicillin- since 1978, causes hives Prior Illnesses/Injuries: Hypercholesterolemia x 5 years; well controlled with medications GERD x 5 years; well controlled with medications Hypothyroidism x 9 years; well controlled with medications Seasonal Allergies x 2 years; well controlled with medications Chicken Pox as a child; denies any other major childhood illnesses Previous Injuries: Patient denies any previous injuries Previous Operations: Appendectomy- 1984; no complications Cholecystectomy- 1996; no complications Bilateral Carpal Tunnel Release- 2004; no complications Previous Hospitalizations: Pt denies previous hospitalizations Flu vaccine: October 2013 Pneumococcal vaccine: December 2012 PPD Test- December 2013 normal Family History: Mother- age 73- Type II Diabetes Mellitus, Chronic back pain, Hypothyroidism Father- age 74- CHF, GERD, Hyperlipidemia Brother- age 54- Hyperlipidemia Daughter- age 24- no medical problems Son- age 22- no medical problems Social History: Patient is married, one brother- age 54. Pt has one daughter, age 24, and one son, age 22. Pt lives with his wife; two members of household. Patient has a two-year college degree and employed as an electrician for Jacksonville State University and works outside five days a week. Pt has an optimal support system. Patient regularly sees his primary care physician on a regular basis. Last dental visit- 2014. Pt reports he drinks 3-4 beers/week. Patient denies use of smokeless tobacco or cigarette/cigars. Denies past or present use of recreational drugs. Nutrition: Pt eats a lowered cholesterol diet. States he tries to avoid spicy foods as they worsen his GERD. Pt eats three meals daily, once in the morning, once at lunch, and once in the evening. Patient states he snacks throughout the day usually consuming 2-3 snacks daily, mainly consisting of crackers, fruit, and sodas Review of Symptoms: 1. Constitutional: Patient denies fatigue or weakness, recent weight loss or gain, denies fever. 2. Eyes: Patient denies vision changes, blurry vision, eye drainage/tearing, eye pain/itching or eye redness. Denies photophobia. Last eye exam- December 2013 with no abnormal findings. Does not wear glasses or contacts. 3. ENMT: Patient denies vertigo, hearing loss, tinnitus, or use of assistive hearing devices. Denies ear pain, ear drainage. Denies nasal discharge or nosebleeds. Denies difficulty smelling. Pt denies facial/sinus pain or sinus drainage. Denies dental pain. Last dental visit- March 2014 with normal findings. Denis bleeding of gums, mouth odor, ulcers, or sores of the tongue. Denies sore throat, hoarseness, or difficulty swallowing. 4. Cardiovascular: Patient denies chest pain, changes in blood pressure, palpitations, or peripheral edema. Denies claudication or cyanosis of extremities. Denies leg redness or tenderness. 5. Respiratory: Patient denies SOB at rest or upon exertion, orthopnea, or dyspnea. Denies wheezing. Reports exposure to second-hand smoke at work. Complains of intermittent coughing that is worse in the mornings and evening and worsened when exposed to heat. Describes cough as productive with minimal white and yellow sputum. Last CXR- January 2014 with normal findings. CXR done at today’s visit, showing increased bronchial markings with no areas of consolidation. 6. Gastrointestinal: Patient denies any episodes of abdominal pain, nausea, vomiting, or diarrhea. Reports regular, daily BM’s. Last normal BM was today. Denies blood in stool, rectal bleeding, hemorrhoids, or constipation. Denies hematemesis. Denies heartburn. Reports normal appetite with food intolerances to spicy and greasy foods. 7. Genitourinary: Patient denies dysuria, burning, urgency, hematuria, or frequency. Denies flank pain or suprapubic pain. Denies recent urinary tract or bladder infections. Denies penile discharge, incontinence, or history of STD. Currently sexually active with one sexual partner. Reports three lifetime sexual partners. 8. Musculoskeletal: Patient denies body aches, muscle or joint pain, swelling, or stiffness. Denies recent injury or trauma. Denies muscle cramps or muscle weakness. Reports he is physically active on a daily basis and exercises three times a week. Denies neck pain or stiffness. Denies changes in range of motion of upper and lower extremities. 9. Skin: Patient denies skin lesions, rash, itching, moles, hair loss, or dryness. Reports daily sun exposure, but uses sunscreen when working outdoors. 10. Neurologic: Patient denies headaches, dizziness, or vertigo. Denies syncopal episodes, fatigue, or weakness. Denies muscle tremors, numbness, involuntary movements, or tingling. Denies sleep disturbances. 11. Psychiatric: Patient denies decrease in memory or recent mood changes. Denies history of depression, anxiety, hallucinations, or paranoia. 12. Endocrine: Patient denies intolerance to heat or cold, excessive sweating, thirst, or hunger. Denies any unexplained changes in weight. 13. Hematologic/Lymphatic: Patient denies excessive bleeding, bruising, or history of anemia. Denies any previous blood transfusions. Denies swollen lymph nodes or lymph node tenderness. Denies previous history of blood clots. 15. Allergic/Immunologic: Patient reports previous history of seasonal allergies. Denies previous allergy testing. Reports allergies are worse in the spring and fall. Denies hives, rashes, or itchy, watery eyes. No exposure to blood or body fluids. Denies history of immunosuppression. O- Objective Data: 1. Constitutional/General appearance: Patient appears in no acute distress, well developed, well nourished. Appears stated age. Dressed appropriately and behaving in an appropriate manner. Alert and oriented x 3. Vital Signs: T- 98.1 oral, BP- 132/76 mm/Hg, HR-61 bpm, Respirations- 20/ minute, unlabored, Oxygen sat- 99% on room air, Height- 73 inches, Weight- 270 lbs, BMI- 35.62. Physical Examination: 2. Eyes: Sclera normal. No drainage or tearing noted from eyes, no redness. PERRLA. 4 mm bilaterally. 3. ENT/Mouth: Tympanic membranes normal, no bulging or redness noted, light reflex present. Hearing intact to whispered voice. Nasal turbinates reddened and swollen, no nasal drainage noted, no deviated septum, no lesions noted. Maxillary sinuses tender upon light palpation bilaterally. Frontal sinuses nontender upon light or deep palpation. Oral cavity mucosa pink and moist. No dental caries noted. Pharynx reddened with no exudate visualized, tonsils present and normal, uvula midline. No evidence of bleeding of gums or foul odor, no ulcers or sores. Cardiovascular: Apical pulse normal. Regular rate and rhythm noted. Normal S1 and S2. No S3 or S4. No murmurs, clicks, or gallops. Peripheral pulses with normal rate and rhythm. No JVD. No carotid bruits auscultated. No edema noted to upper or lower extremities. Capillary refill brisk, < 3 seconds. No discoloration noted to extremities. No varicose veins. Respiratory: Equal rise and fall of chest visualized. No tenderness upon palpation. Patient with normal rate and effort. Normal tactile fremitus. No hyperresonnance or dullness noted upon palpation. Wheezing auscultated in upper lobes bilaterally; normal breath sounds auscultated in lower lobes bilaterally. No rhonchi auscultated. No clubbing noted. Abdomen: Abdomen soft and nondistended. Bowel sounds normal in all four quadrants. No tenderness noted upon light or deep palpation. No guarding. Genitourinary: No CVA tenderness present. Musculoskeletal: Normal ROM noted in upper and lower extremities. Pt denies pain upon movement. Patient denies calf tenderness. Normal muscle strength in upper and lower extremities. No abnormal curvature of spine. Skin: Skin warm, dry, pink. No bruising noted. No discolored or uneven moles, open wounds, no redness or rashes noted. Neurological: Patient is alert and oriented x 3. Hand grips strong and equal bilaterally. Speech is clear. No tremors or involuntary movements. Psychiatric: Pt is calm, cooperative, behaving in an appropriate manner, answering questions appropriately. Normal affect. Hematologic/Lymphatic/Immunologic: No bruising noted. No enlarged lymph nodes palpated. Patient denies tenderness upon palpation of thyroid. Results of Diagnostic Tests: Chest, 2 View- Increased bronchial markings with no consolidated areas to suggest pneumonia. Sinus X-ray (Waters view) - Clouding and mucosal thickening of maxillary sinuses. CBC- WBC- 11.2, otherwise wnl. A- Assessment/Analysis: Level of Visit: Level 3 Diagnoses: 1. 466.0 Acute Bronchitis 2. 461.0 Acute Maxillary Sinusitis 3. 786.2 Cough P- Plan: 1,2. Dekasol 1 mg/1 unit- 10 mg IM injection given in office 1,2. Clindamycin 300 mg/unit- 600 mg IM injection given in office 1,2. Rx for Levaquin 500 mg tablets, One tablet PO once daily x 10 days, dispense 10 with no refills. (product selection permitted) 2. Mucinex D 60 mg/ 600 mg, extended release tablets, One tablet PO BID PRN congestion, dispense 30 with no refills (product selection permitted) 1,3- ProAir HFA 90 mcg/actuation aerosol inhaler, 2 puffs QID PRN wheezing, dispense one unit with no refills. (product selection permitted) 1,3- Promethazine DM 6.25 mg-15 mg/5 ml syrup, Take 1-2 teaspoons PO QID PRN cough, dispense 6 ounces with no refills. (product selection permitted) Follow-up- Patient is instructed to follow up if symptoms are not improved in 48-72 hours. If symptoms resolved, patient is to follow up in two weeks for repeat CXR, sooner if condition worsens. Patient Education1. Patient is instructed to take all medications as prescribed and in their entirety. Importance of taking full course of antibiotics stressed to patient. Medication education provided for patient at time of discharge from clinic. 2. Patient instructed to rest and avoid the heat x 3 days, work excuse given. 3. Patient is instructed to increase PO fluid intake. 4. Patient educated on importance of good handwashing techniques. 5. Patient is instructed to avoid antihistamines 6. Patient is encouraged to use a humidifier at night while sleeping. Levaquin (Levofloxacin)- prescribed for this patient for treatment of acute bronchitis and acute maxillary sinusitis due to symptoms lasting > 21 days with allergy to PCN. MOA- Levaquin is a fluourinated quinolone that exerts a broad-spectrum bactericidal effects. It inhibits DNA gyrase which is required for DNA replication and transcription, DNA repair, recombination, and transposition within the bacteria. Usual dosage- 10-20 mg/kg/day PO every 12-24 hours x 7-10 days. Available as name brand, Levaquin. Also available as generic, Levofloxacin. Cost for 10 day supply- Wal-Mart Jacksonville, Alabama: Brand: $263.25, Generic: $8.56 CVS, Jacksonville, Alabama: Brand: $270.47, Generic: $41.25 Walgreen’s, Jacksonville, Alabama: Brand: $264.54, Generic: $11.89