pubdoc_3_25636_1660
advertisement

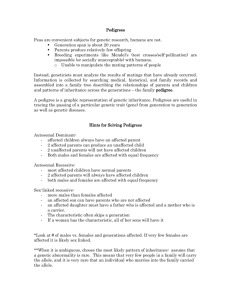
MOLECULAR AND GENETIC MEDICINE Lec:2 Dr.Mohammed Alhamdany Patterns of disease inheritance Autosomal dominant inheritance Autosomal dominant disorders are caused by inheritance of a genetic abnormality in only one of the two copies (alleles) of a single gene. The risk of an affected individual transmitting an autosomal disease to his or her offspring is 50% for each pregnancy, since half the affected individual gametes (sperm or egg cells) will contain the affected chromosome and half will contain the normal chromosome. However, even within a family, individuals with the same mutation rarely have identical patterns of disease due to variable penetrance and/or expressivity. Penetrance is defined as the proportion of individuals bearing a mutated allele who develop the disease phenotype. The mutation is said to be fully penetrant if all individuals who inherit a mutation develop the disease. Expression is the variation of disease severity for the same genotype. Neurofibromatosis type 1 is an example of a disease that is fully (100%) penetrant but which shows extremely variable expressivity. Autosomal recessive inheritance In autosomal recessive disorders, both alleles of a gene must be mutated before the disease is manifest in an individual, and an affected individual must inherit one mutant allele from each parent. The distinguishing feature of recessive diseases is that carrying one mutant allele does not produce a phenotype (carrier). Autosomal recessive disorders are rare in most populations. For example, the most common serious autosomal recessive disorder in the UK is cystic fibrosis, which has a birth incidence of 1:2500. Genetic risk calculation for a fully penetrant autosomal recessive disorder is straightforward. Each subsequent pregnancy of a couple who have had a previous child affected by an autosomal recessive disorder will have a 25% (1:4) risk of 1 being affected; a healthy individual who has a sibling with an autosomal recessive disorder will have 2/3 chance of being a carrier.(why? Please look to the figure in the last of the lecture) X-linked inheritance Genetic diseases caused by mutations on the X chromosome have specific characteristics. X-linked diseases are mostly recessive and restricted to males who carry the mutant allele. This is because males have only one X chromosome, whereas females have two. Thus females who carry a single mutant allele are generally unaffected. Occasionally, female carriers may exhibit signs of an X-linked disease due to a phenomenon called skewed X-inactivation. All females will inactivate one of their two X chromosomes in each cell at a point during development. This process is random in each cell but if, by chance, there is a disproportionate inactivation of normal X chromosomes carrying the normal allele, then an affected female carrier will be more likely. X-linked recessive disorders have a recognisable pattern of inheritance, with transmission of the disease from carrier females to affected males and absence of father-to son transmission. The risk of a female carrier having an affected child is 25% (1:4; half her male offspring). Q: write the conditions in which the female can affected by X linked recessive genetic disorder? ( 3 ) Mitochondrial inheritance The inheritance of mtDNA disorders is characterised by transmission from females, but males and females are generally equally affected. Unlike all the other inheritance patterns mentioned above, mitochondrial inheritance has nothing to do with meiosis but reflects the fact that mitochondrial DNA is transmitted by oöcytes. Mitochondrial disorders tend to be very variable in penetrance and expressivity within families. 2 Classes of genetic variant There are many different classes of variation in the human genome . Rare genetic variations which result in a disease are generally referred to as mutations, whereas common variations and those which do not cause disease are referred to as polymorphisms. These different types of variation are further categorised by the size of the DNA segment involved and/or by the mechanism giving rise to the variation. it include: 1-Nucleotide substitutions The substitution of one nucleotide for another is the most common type of variation in the human genome. Depending on their frequency and functional consequences, these changes are known as a point mutation or a single nucleotide polymorphism. When these substitutions occur within ORFs of a protein-coding gene, they are further classified into: • synonymous (resulting in a change in the codon but no change in the amino acid and thus no phenotype) • missense (altering a codon, resulting in an amino acid change in the protein) • nonsense (introducing a premature stop codon, resulting in truncation of the protein). 2-Insertions and deletions One or more nucleotides may be inserted or lost in a DNA sequence, resulting in an insertion/deletion (in-del) polymorphism or mutation . If an indel change affects one or two nucleotides within the ORF of a protein- coding gene, this can have serious consequences because the triple nucleotide sequence of the codons is disrupted, resulting in a frameshift mutation. The effect upon the gene is typically severe because the amino acid sequence is totally disrupted. 3-Simple tandem repeat mutation Variations in the length of simple tandem repeats of DNA are thought to arise as the result of slippage of DNA during meiosis and are termed microsatellite (small) or minisatellite (larger) 3 repeats. These repeats are unstable and can expand or contract in different generations. This instability is related to the size of the original repeat, many doesn't had effect ,However, some genetic diseases, including Huntington disease and myotonic dystrophy, are caused by microsatellite repeats which result in duplication of amino acids . 4-Copy number variations Variation in the number of copies of an individual segment of the genome from the usual diploid (two copies) content can be categorised by the size of the segment involved. Rarely, individuals may gain or lose a whole chromosome. Such numerical chromosome anomalies most commonly occur by a process known as meiotic non-dysjunction . This is the most common cause of Down’s syndrome, known as trisomy (three copies) of chromosome 21. Examples of chromosome and contiguous disorders: 1-Numerical chromosomal abnormalities gene Down’s syndrome (trisomy 21) 47,XY,+21 :,Characteristic facies, IQ usually < 50, congenital heart disease Klinefelter’s syndrome 47,XXY :Phenotypic male, infertility, gynaecomastia, small testes Turner’s syndrome 45,X :Phenotypic female, short stature, webbed neck, coarctation of the aorta, primary amenorrhoea 2-Recurrent deletions, microdeletions Di George/velocardiofacial syndrome :Cardiac outflow tract defects, distinctive facial appearance, thymic hypoplasia, cleft palate and hypocalcaemia. 3-Diseases associated with triplet and other repeat sequences Coding repeat expansion: Huntington disease Non-coding repeat expansion: Myotonic dystrophy, Friedreich’s ataxia. 4 General principles of diagnosis of genetic disease: 1- Clinical history and examination, routine Ix, for patient and his family. 2-Constructing a family tree: include detail about 3 generations. 3-Polymerase chain reaction (PCR) and DNA sequencing: Almost any tissue can be used to extract DNA for PCR analysis, but most commonly, a sample of peripheral blood is used. 4-Assessing DNA copy number: Visible microscopy for detecting the gain or loss of whole chromosomes or large chromosomal segments (> 4 million bp). Detection of submicroscopic chromosome anomalies requires special techniques for identification . Fluorescent in situ hybridisation (FISH) and multiplex ligation-dependent probe amplification (MLPA) are two of the most widely used techniques to identify such syndromes. However, the availability of whole-genome microarrays has revolutionised chromosome analysis, as it allows the rapid detection of gain or loss of any segment of DNA throughout the genome. 5-Non-DNA-based methods of assessment: Although DNAbased diagnostic tools are used in the vast majority of patients with suspected genetic disease, it may sometimes be more economical or convenient to measure enzyme activity rather than sequencing the coding region of the genes involved. Genetic testing in pregnancy Methods used in prenatal testing 1-Ultrasound: in 1st trimester onwards as increased nuchal translucency (an edematous flap of skin at the base of the neck) for trisomies and Turner’s; all major abnormalities such as neural tubal defect, congenital heart disease. 2-Chorionic villus biopsy: From 11 weeks complicated by 2% risk of miscarriage; it used for early chromosomal, DNA and biochemical analysis. 3-Amniocentesis: From 14 weeks complicated by < 1% risk of miscarriage; it used for chromosomal and some biochemical analysis, e.g. alpha-fetoprotein for NTD. 4-Cordocentesis: From 19 weeks complicated by 2–3% risk of miscarriage; a highly specialised test; used for chromosomal and DNA analysis. Indication of prenatal test: 1-Advanced maternal age and a high-risk serum screening result. 2- A previous child with a detectable chromosome abnormality. 5 3- A parent or child with a genetic disease for which testing is available. 4-Abnormal antenatal scan 6