Potassium Balance
advertisement

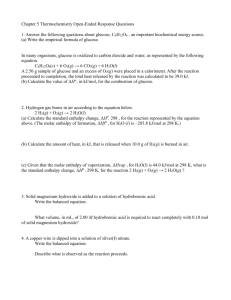
Potassium Balance & Urea Transport Learning Objectives: 1) Describe the effects of changes in K+ intake on serum [K+] and body [K+] content a. Distribution of potassium in tissues i. K+ intake 100 mEq/day 1. Muscle 2550 mEq - largest store 2. Bone 300 mEq 3. ECF 70 mEq - small shifts from tissue will dramatically increase ECF a. Extensive cell damage can lead to potentially fatal hyperkalemia 4. Liver 250 mEq 5. RBC 250 mEq ii. K+ excretion 90-95 mEq/day in urine + 5-10 mEq/day in feces b. Hyperkalemia normally does not occur because ingested K+ enters the liver and skeletal muscle c. Potassium directly stimulates the adrenal cortex to release aldosterone (does not need renin) i. This influences the collecting duct to reabsorb sodium and water but secrete potassium ii. More K+ in the serum means more K+ excreted in the urine 1. Small changes in serum [K+] create large changes in aldosterone secretion 2) Name 2 hormones that stimulate uptake of potassium by liver and skeletal muscle a. K+ is stimulated for uptake out of the ECF by the stimulated of Na+, K+, ATPase by: i. Insulin – after a meal ii. Epinephrine – during exercise 3) Explain the mechanism of potassium reabsorption in the proximal tubule a. K+ reabsorption in the proximal tubule occurs by passive diffusion along concentration gradients similar to Cl- & urea reabsorption 4) Give the percentage of the filtered load of potassium reabsorbed in the proximal tubule and the loop of Henle a. Proximal tubule – 67% of filtered K+ is reabsorbed 5) Compare the fraction of the filtered load of potassium delivered to the cortical collecting duct to the fraction excreted in the urine, in normal and K+ depleted animals a. The fraction of filtered K+ delivered to the cortical collecting duct is about 13% b. The fraction excreted in the urine depends on whether there is high or low [K+] i. During high intake, 15-80% of amount filtered load may be excreted ii. During low intake, 1% of the filtered load may be excreted 6) Show approximate values for the electrical and concentration gradients affecting K+ diffusion across the luminal and peritubular cell membranes of the collecting duct a. In the collecting duct: i. Electrical gradient 1. Urine – -30mV 2. Cell – -80mV 3. Blood – 0mV ii. Concentration gradient 1. Urine – 15 mEq/L 2. Cell – 150 mEq/L 3. Blood – 5 mEq/L b. K+ secretion in the urine occurs because --- concentration gradient driving K+ out of the cell is greater than electrical gradient bringing K+ into the cell 7) Describe the effect of changes in serum [K+] on cell [K+] and K+ secretion in principal cells in the collecting duct a. Aldosterone acts on the principal cells to increase K+ secretion and excretion 8) Describe the effect of changes in serum [K+] on aldosterone secretion a. K+ secretion is stimulated by increased serum [K+] and aldosterone i. Aldosterone acts by increasing the number of K+ channels in the luminal membrane (short-term) and stimulating synthesis of Na+, K+, ATPase (long-term) 9) Explain how normal Na+ balance in maintained when there is a change in dietary K+ intake a. Increased K+ intake leads to increased serum [K+] which does 2 things: i. Increased aldosterone secretion 1. Leads to increased Na+ reabsorption and increased blood volume a. This leads to increased ANP and urodilatin, decreased renal nerve activity, and decreased FF 2. Leads to increased K+ secretion ii. Increase in cell [K+] in principal cells 1. Leads to increased K+ secretion a. Increased urinary K+ excretion and restores K+ balance b. In response to an increase in K+ intake, K+ excretion increases and K+ balance is restored, but there is a transient Na+ retention 10) Name the segment of the nephron that is most important for adjusting K+ excretion to match K+ intake under normal conditions a. Collecting duct – has principal cells and intercalated cells i. Intercalated cells – K+ secretion by principal cells is decreased 1. H+, K+, ATPase in intercalated cells is activated 2. Net K+ reabsorption in intercalated cells occurs via primary active K+ transport 3. Intercalated cells also secrete H+ via an H+ ATPase 11) Describe the mechanism for reabsorption of urea in the proximal tubule and medullary collecting duct: include the effect of ADH on urea transport a. Filtered load of urea = 100% b. 50% reabsorbed in the proximal tubule i. 50% delivered to the Loop c. 60% passively secreted from interstitium into the thin limbs i. Urea that diffuses out of the medullary collecting duct re-enters the tubules in the thin limbs; this path is called UREA RECYCLING d. Thick ascending limb – no transport of urea e. 110% is present at the beginning of the distal tubule i. Reabsorption of H2O in the cortical and medullary collecting duct concentrates urea ii. At the bottom of the MCD, 70% of urea is reabsorbed into vasa recta and thin limbs of Loop 1. 60% into interstitium & 10% into vasa recta f. Urea permeability depends on [ADH] i. As urine flow increases in a water diuresis (remember this would happen with a decreased serum [ADH]) urea reabsorption in MCD decreases and excretion and clearance increase ii. In an antidiuresis, urine flows slowly, urea is almost completely reabsorbed, and BUN increases g. Urea crosses cell membranes by facilitated diffusion h. 40% of the original is excreted 12) List three factors that increase serum urea concentration (blood urea nitrogen, BUN) i. BUN = 4-8 mmol/L b. Protein digestion i. Catabolism of tissues (steroids, fever, burns, wasting) c. Reabsorption of urea from kidney d. Intestinal hemorrhage and bacterial catabolism of blood 13) Define the term, prerenal azotemia and explain how the BUN/creatinine ratio changes in prerenal azotemia a. Prerenal Azotemia – normal BUN/creatinine ratio = 10 to 15 i. Ratio of > 20 indicates prerenal azotemia ii. The BUN/creatinine ratio will increase if the degree of volume depletion is not sufficient to decrease GFR and thus creatinine clearance 1. Such as during a decrease in volume leads to increased ADH and increased FF all leading to increased urea reabsorption b. Azotemia – an excess of urea and other nitrogenous waste in the blood c. BUN > 20x serum creatinine i. Decreased GFR, increased stimulus for reabsorption of urea and: 1. Increased protein ingestion 2. GI hemorrhage 3. Increased tissue catabolism d. BUN < 10x serum creatinine i. Very low protein intake and renal parenchymal disease ii. Repeated dialysis iii. Vomiting or diarrhea iv. Hepatic insufficiency plus renal insufficiency