DOCX ENG
advertisement

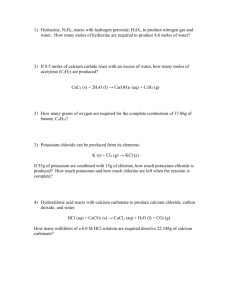
B- CRF : Nutritional complications E- 01 : Primitive hypertension Daily potassium intake and sodium-to-potassium ratio in the reduction of blood pressure: a meta-analysis of randomized controlled trials Binia, Aristeaa; Jaeger, Jonathanb; Hu, Youyoub; Singh, Anuragb; Zimmermann, Dianec Correspondence to Dr Aristea Binia, Nestlé Research Center, P.O. Box 44, Vers-chez-les-Blanc, CH-1000 Lausanne 26, Switzerland. Tel: +41 21 785 8278; fax: +41 21 785 8554; e-mail: aristea.binia@rdls.nestle.com Journal : Journal of Hypertension Year: 2015 / Month : August Volume : 33 Pages : 1509–1520 doi: 10.1097/HJH.0000000000000611 ABSTRACT Objective To evaluate the efficacy of daily potassium intake on decreasing blood pressure in non-medicated normotensive or hypertensive patients, and to determine the relationship between potassium intake, sodium-to-potassium ratio and reduction in blood pressure. Design Mixed-effect meta-analyses and meta-regression models. Data sources Medline and the references of previous meta-analyses. Studies eligibility criteria Randomized controlled trials with potassium supplementation, with blood pressure as the primary outcome, in non-medicated patients. Results Fifteen randomized controlled trials of potassium supplementation in patients without antihypertensive medication were selected for the meta-analyses (917 patients). Potassium supplementation resulted in reduction of SBP by 4.7 mmHg [95% confidence interval (CI) 2.4–7.0] and DBP by 3.5 mmHg (95% CI 1.3–5.7) in all patients. The effect was found to be greater in hypertensive patients, with a reduction of SBP by 6.8 mmHg (95% CI 4.3–9.3) and DBP by 4.6 mmHg (95% CI 1.8–7.5). Meta-regression analysis showed that both increased daily potassium excretion and decreased sodium-to-potassium ratio were associated with blood pressure reduction (P < 0.05). Increased total daily potassium urinary excretion from 60 to 100 mmol/day and decrease of sodium-to-potassium ratio were shown to be necessary to explain the estimated effect. Conclusion Potassium supplementation is associated with reduction of blood pressure in patients who are not on antihypertensive medication, and the effect is significant in hypertensive patients. The reduction in blood pressure significantly correlates with decreased daily urinary sodium-to-potassium ratio and increased urinary potassium. Patients with elevated blood pressure may benefit from increased potassium intake along with controlled or decreased sodium intake. COMMENTS Diets high in sodium (>4 g/day) and low in potassium (<2 g/day) have been associated with an increased risk of high BP. High dietary potassium (>3.5 g/day) is associated with a decrease in BP. The unique focus of the present study was to analyse available randomized controlled trials (RCTs) for the effect of potassium supplementation on BP in patients without antihypertensive medication. The authors investigated the dose response of potassium, as well as the relationship of the sodiumto-potassium ratio (Na/K) with BP. This metanalyse was conducted according to Cochrane Collaboration guidelines. Finally, 15 studies fulfilling the inclusion criteria and having the necessary information contributed to this meta-analyses. Most of the studies used potassium chloride (KCl) tablets or elixirs for potassium supplementation Most of the studies had a potassium intervention of 60–65 mmol/day. Increased potassium intake leads to a decrease in SBP by 4.7 mmHg (95% CI 2. –7.0) and DBP by 3.5 mmHg (95% CI 1.3–5.7) in all patients. A greater reduction was seen in hypertensive patients with a reduction of SBP by 6.8 mmHg (95% CI 4.3–9.3) and DBP by 4.6 mmHg (95% CI 1.8–7.5). In conclusion, the BP-lowering effect of ingested potassium cannot be assessed alone, but must be considered in relation to sodium in the diet. The evidence from clinical trials with a potassium and/or sodium intervention and from the meta-analyses of these trials indicates that early dietary modifications towards a Na/K molar ratio of about one unit could make a valuable contribution to preventive measures for hypertension. Pr. Jacques CHANARD Professor of Nephrology