RENAL MALIGNANCIES IN KIDNEY TRANSPLANT RECIPIENTS
advertisement

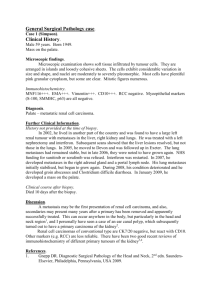
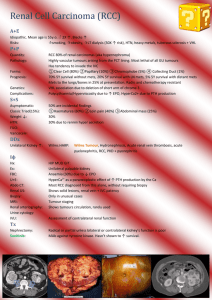
RENAL MALIGNANCIES IN KIDNEY TRANSPLANT RECIPIENTS S. Şen1, B. Sarsık1, S.S. Özbek2, C. Hoşçoşkun3, M. Yılmaz4, H. Töz4. Departments of Pathology1, Radiology2, Surgery3, and Nephrology4, Ege University, School of Medicine, İzmir, Turkey Objectives: Kidney transplantation has consistently become a primary therapeutic option in patients with end-stage renal disease. The preservation of allograft function has only become possible through immunosuppressive agents. However, immunosuppressive therapy increases the incidence of posttransplantation cancer. The risk of renal cell carcinoma (RCC) development in renal transplant recipients (RTRs) is 15–100 times higher. Primary RCC represents 5% of all cancers in transplant recipients. The treatment options for malignancy in a renal allograft include radical nephrectomy or nephron-sparing surgery. We report two patients who underwent radical nephrectomy and nephronsparing surgery in the grafted kidney. Case 1: A 48-year-old man underwent renal transplantation in 2000 for treatment of renal failure secondary to hypertensive nephropathy. After an uncomplicated 8-year posttransplant course, during ultrasonographic evaluation of the graft, a solid, round mass, 4 cm in diameter was found. Tru-cut biopsy showed malign epithelial neoplasm in the medulla was not compatible with RCC. The renal mass was visualized by abdominal computed tomography (CT). Further workup was suspected for metastatic lung and liver disease. We made an interdisciplinary decision for a allograft nephroureterectomy. Histology of the specimen was consistent with a metastatic carcinoma associated localize amyloidosis. The donor history was evaluated and found she died metastatic carcinoma with unknown primary. Detailed histopathological work up for donor and recipients tumor was consistent with metastatic neuroendocrine carcinoma (medullary carcinoma). After the surgery and interruption of immunosuppressive therapy, the concomitant metastatic findings resolved. At follow-up of 3 years, the patient is alive with no signs of distant disease. Case 2: A 31-year-old man underwent renal transplantation in 1997 for treatment of renal failure secondary to vesicoureteral reflux. After an uncomplicated 12-year posttransplant course, during ultrasonographic evaluation of the graft revealed a solid, round mass, 4 cm in diameter. Tru-cut biopsy showed malign papillary RCC. The mass was visualized by abdominal computed tomography. It was welldemarcated from the surrounding renal parenchyma. We made an interdisciplinary decision for a partial nephrectomy. Using sharp dissection, a resection of the mass was performed with clear margins. Pathologic diagnosis indicated grade II, stage pT1, papillary RCC. At follow-up of 2 years, the patient is doing well with no signs of recurrence or distant disease. Conclusion: Routine ultrasonographic screening should be done for early renal carcinoma. Allograft biopsy might be useful for therapy options. Our limited results imply that partial nephrectomy may be a safe and effective treatment protocol for RCC in allograft kidneys. Metastatic donor carcinoma in the recipient may be cured without chemotherapy.