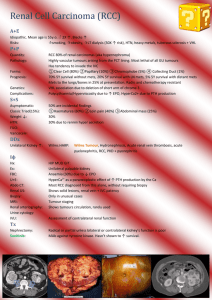
RENAL CELL CARCINOMA
advertisement

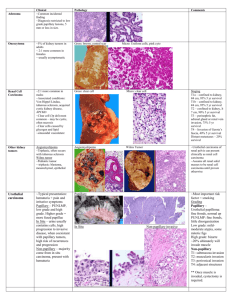
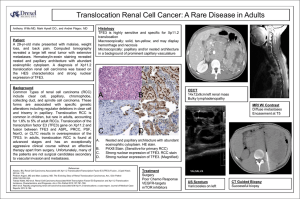
RENAL CELL CARCINOMA GENETIC BASIS BACKGROUND • 3% of adult malignancies • 90-95% of neoplasms arising from the kidney [tissue of origin - proximal renal tubular epithelium] • Lack of early warning signs, diverse clinical manifestations • Resistance to radiation and chemotherapy, infrequent but reproducible responses to immunotherapy viz. IFN-alpha and IL-2 • Targeted therapy [anti angiogenic] Genetics • structural alterations of ch.3p • tumor suppressors (VHL, TSC) or oncogenes (MET) • 4 hereditary syndromes associated: 1. von Hippel-Lindau (VHL) syndrome, 2. hereditary papillary renal carcinoma (HPRC), 3. familial renal oncocytoma (FRO) associated with Birt-Hogg-Dube syndrome (BHDS), and 4. hereditary renal carcinoma (HRC). von Hippel-Lindau syndrome • • • • Autosomal dominant Multiple cancers RCC in nearly 40% of patients del (3p) or t (3;6) or t (3;8) => VHL gene (3p26-p25) mutated => accumulation of hypoxia inducible factors (HIFs) that stimulate angiogenesis through VEGF and VEGFR Hereditary papillary renal carcinoma • AD • bilateral, multifocal papillary renal carcinoma • Germline missense mutations in the tyrosine kinase domain of the MET gene (7q31) => constitutive activation • TFE3 mutation • t(X;1)(p11;q21) • Papillary renal cell tumours divided into two groups 1. Tumours with a combined trisomy of chromosomes 7 and 17 as well as loss of the Y chromosome are papillary renal cell adenomas 2. Tumours with additional trisomies such as trisomy 16, 20 or 12 are papillary renal cell carcinomas 3. Chromophobe renal cell carcinomas show a combination of allelic losses, which do not occur in other types of renal tumours MET • β-subunit of c-Met product is the cellsurface receptor for hepatocyte growth factor • amplified during the transition between primary tumors and metastasis • metastatic potential relies on the properties of its multifunctional docking site • PRC commonly show trisomy of ch.7 Familial renal oncocytoma • usually benign tumors • Ultrastructural characterization exhibits dense packing of the cells with mitochondria that show morphologic differences from those in normal cells [larger, abnormally shaped] • Mutation in mtDNA within the CyC oxidase subunit I gene FRO • do not show loss of alleles at loci on 3p • Loss of ch.1 and ch.Y represent at least 1 subset of oncocytomas. • Rearrangements involving 11q13 characterize another subset BIRT-HOGG-DUBE SYNDROME • BHD gene 17p11.2 [TS] • Adult onset • male-to-male transmission Molecular markers for RCC • Not very well characterised 1. CAIX – VHL mediated For patients with nonmetastatic RCC and at high risk for progression, low CAIX predicts worse outcome Overall expression of CAIX with development of metastasis 2. Alpha-methylacyl-CoA racemase – significant increase of AMACR mRNA levels in papillary renal cell carcinomas only – Also molecular marker for prostate cancer 3. B7-H1 – expression may indicate worse survival, possibly through impaired host antitumor immunity 4. Microsatellite instabilities General Diagnosis • • • • Immunohistochemistry Biochemical analysis Molecular techniques – microarray, PCR Cytogenetics – Karyotyping, FISH N RCC Use? • • • • Staging Prognostic marker Differential diagnosis of RCC subtypes Pattern of DNA alterations in urine, but not serum, found in benign renal masses - basis to help differentiate malignant from benign tumors and identify patients who might benefit from a watchful waiting approach • Likely target for therapy Questions?