Top 10 Cancers Affecting Young Adults
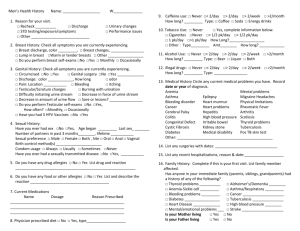
advertisement
Every 8 minutes, a young adult is diagnosed with cancer. That’s over 70,000 people in their 20s and 30s each year. Awareness is power. B REAST breasts) before age 30 are at an increased risk of breast cancer. This includes women treated with radiation for Hodgkin lymphoma. Studies show that the younger a woman was when she received radiation treatment, the higher her risk of breast cancer later in life. CANCER Breast Cancer is cancer that forms in tissues of the breast, usually the ducts (tubes that carry milk to the nipple) and lobules (glands that make milk). It occurs in both men and women, although male breast cancer is rare. Reproductive and menstrual history: o RISK FACTORS Some of the risk factors for breast cancer include: o o Personal health history: Having breast cancer in one breast increases your risk of getting cancer in your other breast. Also, having certain types of abnormal breast cells (atypical hyperplasia, lobular carcinoma in situ [LCIS], or ductal carcinoma in situ [DCIS]) increases the risk of invasive breast cancer. These conditions are found with a breast biopsy. Family health history: Your risk of breast cancer is higher if your mother, father, sister, or daughter had breast cancer. The risk is even higher if your family member had breast cancer before age 50. Having other relatives (in either your mother's or father's family) with breast cancer or ovarian cancer may also increase your risk. Certain genome changes: Changes in certain genes, such as BRCA1 or BRCA2, substantially increase the risk of breast cancer. Tests can sometimes show the presence of these rare, specific gene changes in families with many women who have had breast cancer, and health care providers may suggest ways to try to reduce the risk of breast cancer or to improve the detection of this disease in women who have these genetic changes. Radiation therapy to the chest: Women who had radiation therapy to the chest (including the The older a woman is when she has her first child, the greater her chance of breast cancer. Women who never had children are at an increased risk of breast cancer. Women who had their first menstrual period before age 12 are at an increased risk of breast cancer. Breast density: Breasts appear on a mammogram (breast x-ray) as having areas of dense and fatty (not dense) tissue. Women whose mammograms show a larger area of dense tissue than the mammograms of women of the same age are at increased risk of breast cancer. History of taking DES: DES was given to some pregnant women in the United States between about 1940 and 1971. (It is no longer given to pregnant women.) Women who took DES during pregnancy may have a slightly increased risk of breast cancer. The possible effects on their daughters are under study. Lack of physical activity Drinking alcohol SYMPTOMS Early breast cancer usually doesn't cause symptoms. But as the tumor grows, it can change how the breast looks or feels. The common changes include: A lump or thickening in or near the breast or in the underarm area A change in the size or shape of the breast Dimpling or puckering in the skin of the breast A nipple turned inward into the breast Discharge (fluid) from the nipple, especially if it's bloody Scaly, red, or swollen skin on the breast, nipple, or areola (the dark area of skin at the center of the breast). The skin may have ridges or pitting so that it looks like the skin of an orange. B RAIN CENTRAL & OTHER NERVOUS SYSTEM TUMORS not shown consistent links between these possible risk factors and brain tumors, but additional research is needed. SYMPTOMS The symptoms of a brain tumor depend on tumor size, type, and location. Symptoms may be caused when a tumor presses on a nerve or harms a part of the brain. Also, they may be caused when a tumor blocks the fluid that flows through and around the brain, or when the brain swells because of the buildup of fluid. Brain cancer is the result of the growth of abnormal cells in the tissues of the brain. Brain tumors can be benign (not cancer) or malignant (cancer). When most normal cells grow old or get damaged, they die, and new cells take their place. Sometimes, this process goes wrong. New cells form when the body doesn't need them, and old or damaged cells don't die as they should. The buildup of extra cells often forms a mass of tissue called a growth or tumor. These are the most common symptoms of brain tumors: RISK FACTORS Studies have found the following risk factors for brain tumors: Ionizing radiation: Ionizing radiation from high dose x-rays (such as radiation therapy from a large machine aimed at the head) and other sources can cause cell damage that leads to a tumor. People exposed to ionizing radiation may have an increased risk of a brain tumor, such as meningioma or glioma. Family history: It is rare for brain tumors to run in a family. Only a very small number of families have several members with brain tumors. Researchers are studying whether using cell phones, having had a head injury, or having been exposed to certain chemicals at work or to magnetic fields are important risk factors. Studies have Headaches (usually worse in the morning) Nausea and vomiting Changes in speech, vision, or hearing Problems balancing or walking Changes in mood, personality, or ability to concentrate Problems with memory Muscle jerking or twitching (seizures or convulsions) Numbness or tingling in the arms or legs C ERVICAL CANCER Cervical Cancer is cancer that forms in tissues of the cervix (the organ connecting the uterus and vagina). It is usually a slow-growing cancer that may not have symptoms but can be found with regular Pap tests (a procedure in which cells are scraped from the cervix and looked at under a microscope). RISK FACTORS Infection with HPV (human papillomavirus) is the main cause of cervical cancer. HPV infection and other risk factors may act together to increase the risk even more: HPV infection: HPV is a group of viruses that can infect the cervix. An HPV infection that doesn't go away can cause cervical cancer in some women. HPV is the cause of nearly all cervical cancers. HPV infections are very common. These viruses are passed from person to person through sexual contact. Most adults have been infected with HPV at some time in their lives, but most infections clear up on their own. Some types of HPV can cause changes to cells in the cervix. If these changes are found early, cervical cancer can be prevented by removing or killing the changed cells before they can become cancer cells. Lack of regular Pap tests: Cervical cancer is more common among women who don't have regular Pap tests. The Pap test helps doctors find abnormal cells. Removing or killing the abnormal cells usually prevents cervical cancer. Smoking: Among women who are infected with HPV, smoking cigarettes slightly increases the risk of cervical cancer. Weakened immune system (the body's natural defense system): Infection with HIV (the virus that causes AIDS) or taking drugs that suppress the immune system increases the risk of cervical cancer. Sexual history: Women who have had many sexual partners have a higher risk of developing cervical cancer. Also, a woman who has had sex with a man who has had many sexual partners may be at higher risk of developing cervical cancer. In both cases, the risk of developing cervical cancer is higher because these women have a higher risk of HPV infection. Using birth control pills for a long time: Using birth control pills for a long time (5 or more years) may slightly increase the risk of cervical cancer among women with HPV infection. However, the risk decreases quickly when women stop using birth control pills. Having many children: Studies suggest that giving birth to many children (5 or more) may slightly increase the risk of cervical cancer among women with HPV infection. DES (diethylstilbestrol): DES may increase the risk of a rare form of cervical cancer in daughters exposed to this drug before birth. DES was given to some pregnant women in the United States between about 1940 and 1971. (It is no longer given to pregnant women.) SYMPTOMS Early cervical cancers usually don't cause symptoms. When the cancer grows larger, women may notice one or more of these symptoms: Abnormal vaginal bleeding o Bleeding that occurs between regular menstrual periods o Bleeding after sexual intercourse, douching, or a pelvic exam o Menstrual periods that last longer and are heavier than before Increased vaginal discharge Pelvic pain Pain during sex C OLON CANCER Colon Cancer is cancer that forms in the tissues of the colon (the longest part of the large intestine). Most colon cancers are adenocarcinomas (cancers that begin in cells that make and release mucus and other fluids). RISK FACTORS Studies have found the following risk factors for colorectal cancer: Colorectal polyps: Polyps are growths on the inner wall of the colon or rectum. They are common in people over age 50. Most polyps are benign (not cancer), but some polyps (adenomas) can become cancer. Finding and removing polyps may reduce the risk of colorectal cancer. Family history of colorectal cancer: Close relatives (parents, brothers, sisters, or children) of a person with a history of colorectal cancer are somewhat more likely to develop this disease themselves, especially if the relative had the cancer at a young age. If many close relatives have a history of colorectal cancer, the risk is even greater. Personal history of cancer: A person who has already had colorectal cancer may develop colorectal cancer a second time. Also, women with a history of cancer of the ovary, uterus (endometrium), or breast are at a somewhat higher risk of developing colorectal cancer. Ulcerative colitis or Crohn disease: A person who has had a condition that causes inflammation of the colon (such as ulcerative colitis or Crohn's disease) for many years is at increased risk of developing colorectal cancer. Diet: Studies suggest that diets high in fat (especially animal fat) and low in calcium, folate, and fibermay increase the risk of colorectal cancer. Also, some studies suggest that people who eat a diet very low in fruits and vegetables may have a higher risk of colorectal cancer. Cigarette smoking: A person who smokes cigarettes may be at increased risk of developing polyps and colorectal cancer. L Having diarrhea or constipation Feeling that your bowel does not empty completely Finding blood (either bright red or very dark) in your stool EUKEMIA Leukemia is cancer that starts in the tissue that forms blood. In a person with leukemia, the bone marrow makes abnormal white blood cells. The abnormal cells are leukemia cells. Unlike normal blood cells, leukemia cells don't die when they should. They may crowd out normal white blood cells, red blood cells, and platelets. This makes it hard for normal blood cells to do their work. RISK FACTORS The risk factors may be different for the different types of leukemia: Radiation: People exposed to very high levels of radiation, such as from radiation therapy for medical treatments and diagnostic x-rays, are much more likely than others to get acute myeloid leukemia, chronic myeloid leukemia, or acute lymphocytic leukemia Smoking: Smoking cigarettes increases the risk of acute myeloid leukemia. Benzene: Exposure to benzene in the workplace can cause acute myeloid leukemia. It may also cause chronic myeloid leukemia or acute lymphocytic leukemia. Benzene is used widely in the chemical industry. It's also found in cigarette smoke and gasoline. Chemotherapy: Cancer patients treated with certain types of cancer-fighting drugs sometimes later get acute myeloid leukemia or acute lymphocytic leukemia. For example, being treated with drugs known asalkylating agents or topoisomerase inhibitors is SYMPTOMS A common symptom of colorectal cancer is a change in bowel habits. Symptoms include: Finding your stools are narrower than usual Frequently having gas pains or cramps, or feeling full or bloated Losing weight with no known reason Feeling very tired all the time Having nausea or vomiting linked with a small chance of later developing acute leukemia. Down syndrome and certain other inherited diseases: Down syndrome and certain other inherited diseases increase the risk of developing acute leukemia. Myelodysplastic syndrome and certain other blood disorders: People with certain blood disorders are at increased risk of acute myeloid leukemia. Human T-cell leukemia virus type I (HTLV-I): People with HTLV-I infection are at increased risk of a rare type of leukemia known as adult T-cell leukemia. Although the HTLV-I virus may cause this rare disease, adult T-cell leukemia and other types of leukemia are not contagious. Family history of leukemia: It's rare for more than one person in a family to have leukemia. When it does happen, it's most likely to involve chronic lymphocytic leukemia. However, only a few people with chronic lymphocytic leukemia have a father, mother, brother, sister, or child who also has the disease. SYMPTOMS Like all blood cells, leukemia cells travel through the body. The symptoms of leukemia depend on the number of leukemia cells and where these cells collect in the body. People with chronic leukemia may not have symptoms. The doctor may find the disease during a routine blood test. People with acute leukemia usually go to their doctor because they feel sick. If the brain is affected, they may have headaches, vomiting, confusion, loss of muscle control, or seizures. Leukemia also can affect other parts of the body such as the digestive tract, kidneys, lungs, heart, or testes. Common symptoms of chronic or acute leukemia may include: Swollen lymph nodes that usually don't hurt (especially lymph nodes in the neck or armpit) Fevers or night sweats Frequent infections Feeling weak or tired Bleeding and bruising easily (bleeding gums, purplish patches in the skin, or tiny red spots under the skin) Swelling or discomfort in the abdomen (from a swollen spleen or liver) Weight loss for no known reason Pain in the bones or joints L YMPHOMA There are two types of lymphoma: Hodgkin Lymphoma and NonHodgkin Lymphoma. Hodgkin Lymphoma is a cancer of the immune system that is marked by the presence of a type of cell called the ReedSternberg cell. The two major types of Hodgkin lymphoma are classical Hodgkin lymphoma and nodular lymphocytepredominant Hodgkin lymphoma. Non-Hodgkin Lymphoma is any of a large group of cancers of lymphocytes (white blood cells). Non-Hodgkin lymphomas can occur at any age and are often marked by lymph nodes that are larger than normal, fever, and weight loss. There are many different types of nonHodgkin lymphoma. These types can be divided into aggressive (fast-growing) and indolent (slow-growing) types, and they can be formed from either B-cells or T-cells. Bcell non-Hodgkin lymphomas include Burkitt lymphoma, chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL), diffuse large B-cell lymphoma, follicular lymphoma, immunoblastic large cell lymphoma, precursor B-lymphoblastic lymphoma, and mantle cell lymphoma. Tcell non-Hodgkin lymphomas include mycosis fungoides, anaplastic large cell lymphoma, and precursor T-lymphoblastic lymphoma. Lymphomas that occur after bone marrow or stem cell transplantation are usually B-cell non-Hodgkin lymphomas. person. The following are the main types of infection that can increase the risk of lymphoma: o Human immunodeficiency virus (HIV): HIV is the virus that causes AIDS. People who have HIV infection are at much greater risk of some types of non-Hodgkin lymphoma. o Epstein-Barr virus (EBV): Infection with EBV has been linked to an increased risk of lymphoma. In Africa, EBV infection is linked to Burkitt lymphoma. o Helicobacter pylori: H. pylori are bacteria that can cause stomach ulcers. They also increase a person's risk of lymphoma in the stomach lining. o Human T-cell leukemia/lymphoma virus type 1 (HTLV-1): Infection with HTLV-1 increases a person's risk of lymphoma and leukemia. o Hepatitis C virus: Some studies have found an increased risk of lymphoma in people with hepatitis C virus. More research is needed to understand the role of hepatitis C virus. RISK FACTORS The risk factors for Hodgkin Lymphoma include the following: Certain viruses: Having an infection with the Epstein-Barr virus (EBV) or the human immunodeficiency virus (HIV) may increase the risk of developing Hodgkin lymphoma. However, lymphoma is not contagious. You can't catch lymphoma from another person. Weakened immune system: The risk of developing Hodgkin lymphoma may be increased by having a weakened immune system (such as from an inherited condition or certain drugs used after an organ transplant). Age: Hodgkin lymphoma is most common among teens and adults aged 15 to 35 years and adults aged 55 years and older. Family history: Family members, especially brothers and sisters, of a person with Hodgkin lymphoma or other lymphomas may have an increased chance of developing this disease. In general, the risk factors for Non-Hodgkin Lymphoma include the following: Weakened immune system: The risk of developing lymphoma may be increased by having a weakened immune system (such as from an inherited condition or certain drugs used after an organ transplant). Certain infections: Having certain types of infections increases the risk of developing lymphoma. However, lymphoma is not contagious. You cannot catch lymphoma from another Age: Although non-Hodgkin lymphoma can occur in young people, the chance of developing this disease goes up with age. Most people with non-Hodgkin lymphoma are older than 60. Researchers are studying obesity and other possible risk factors for NonHodgkin Lymphoma. People who work with herbicides or certain other chemicals may be at increased risk of this disease. Researchers are also looking at a possible link between using hair dyes before 1980 and NonHodgkin Lymphoma. SYMPTOMS Hodgkin Lymphoma symptoms: can cause many Swollen lymph nodes (that do not hurt) in the neck, underarms, or groin Becoming more sensitive to the effects of alcohol or having painful lymph nodes after drinking alcohol Weight loss for no known reason Fever that does not go away Soaking night sweats Itchy skin Coughing, trouble breathing, or chest pain Weakness and tiredness that don't go away Studies have shown that the following are risk factors for melanoma: Sunlight: Sunlight is a source of UV radiation. It's the most important risk factor for any type of skin cancer. The sun's rays cause skin damage that can lead to cancer. Severe, blistering sunburns: People who have had at least one severe, blistering sunburn are at increased risk of skin cancer. Although people who burn easily are more likely to have had sunburns as a child, sunburns during adulthood also increase the risk of skin cancer. Lifetime sun exposure: The total amount of sun exposure over a lifetime is a risk factor for skin cancer. Tanning: Although a tan slightly lowers the risk of sunburn, even people who tan well without sunburning have a higher risk of skin cancer because of more lifetime sun exposure. Non-Hodgkin Lymphoma can also cause many similar symptoms: Swollen, painless lymph nodes in the neck, armpits, or groin Unexplained weight loss Fever Soaking night sweats Coughing, trouble breathing, or chest pain Weakness and tiredness that don't go away Pain, swelling, or a feeling of fullness in the abdomen M Sunlight can be reflected by sand, water, snow, ice, and pavement. The sun's rays can get through clouds, windshields, windows, and light clothing. In the United States, skin cancer is more common where the sun is strong. For example, more people in Texas than Minnesota get skin cancer. Also, the sun is stronger at higher elevations, such as in the mountains. ELANOMA Melanoma is a form of skin cancer that begins in melanocytes (cells that make the pigment melanin). It may begin in a mole (skin melanoma), but can also begin in other pigmented tissues, such as in the eye or in the intestines. Melanoma can occur on any skin surface. In men, it's often found on the skin on the head, on the neck, or between the shoulders and the hips. In women, it's often found on the skin on the lower legs or between the shoulders and the hips. Melanoma is rare in people with dark skin. When it does develop in people with dark skin, it's usually found under the fingernails, under the toenails, on the palms of the hands, or on the soles of the feet. Melanoma is more likely than other skin cancers to spread to other parts of the body. RISK FACTORS Sunlamps and tanning booths: Artificial sources of UV radiation, such as sunlamps and tanning booths, can cause skin damage and skin cancer. Health care providers strongly encourage people, especially young people, to avoid using sunlamps and tanning booths. The risk of skin cancer is greatly increased by using sunlamps and tanning booths before age 30. Personal history: People who have had melanoma have an increased risk of developing other melanomas. Also, people who have had basal cell or squamous cell skin cancer have an increased risk of developing another skin cancer of any type. Family history: Melanoma sometimes runs in families. Having two or more close relatives (mother, father, sister, brother, or child) who have had this disease is a risk factor for developing melanoma. Other types of skin cancer also sometimes run in families. Rarely, members of a family will have an inherited disorder, such as xeroderma pigmentosum or nevoid basal cell carcinoma syndrome, that makes the skin more sensitive to the sun and increases the risk of skin cancer. dysplastic nevus if it looks like it might have changed into melanoma. SYMPTOMS Often the first sign of melanoma is a change in the shape, color, size, or feel of an existing mole. Melanoma may also appear as a new mole. Thinking of "ABCDE" can help you remember what to look for: Skin that burns easily: Having fair (pale) skin that burns in the sun easily, blue or gray eyes, red or blond hair, or many freckles increases the risk of skin cancer. Certain medical conditions or medicines: Medical conditions or medicines (such as some antibiotics, hormones, or antidepressants) that make your skin more sensitive to the sun increase the risk of skin cancer. Also, medical conditions or medicines that suppress the immune system increase the risk of skin cancer. Dysplastic nevus: A dysplastic nevus is a type of mole that looks different from a common mole. A dysplastic nevus may be bigger than a common mole, and its color, surface, and border may be different. It's usually wider than a pea and may be longer than a peanut. A dysplastic nevus can have a mixture of several colors, from pink to dark brown. Usually, it's flat with a smooth, slightly scaly or pebbly surface, and it has an irregular edge that may fade into the surrounding skin. A dysplastic nevus is more likely than a common mole to turn into cancer. However, most do not change into melanoma. A doctor will remove a More than 50 common moles: Usually, a common mole is smaller than a pea, has an even color (pink, tan, or brown), and is round or oval with a smooth surface. Having many common moles increases the risk of developing melanoma. Asymmetry: The shape of one half does not match the other half. Border that is irregular: The edges are often ragged, notched, or blurred in outline. The pigment may spread into the surrounding skin. Color that is uneven: Shades of black, brown, and tan may be present. Areas of white, gray, red, pink, or blue may also be seen. Diameter: There is a change in size, usually an increase. Melanomas can be tiny, but most are larger than the size of a pea (larger than 6 millimeters or about 1/4 inch). Evolving: The mole has changed over the past few weeks or months. Melanomas can vary greatly in how they look. Many show all of the ABCDE features. However, some may show changes or abnormal areas in only one or two of the ABCDE features. In more advanced melanoma, the texture of the mole may change. The skin on the surface may break down and look scraped. It may become hard or lumpy. The surface may ooze or bleed. Sometimes the melanoma is itchy, tender, or painful. S ARCOMA A sarcoma is a type of cancer that develops from certain tissues, like bone or muscle. The main types of sarcoma are: osteosarcoma, which develops from bone, and soft tissue sarcomas. Soft tissue sarcomas can develop from soft tissues like fat, muscle, nerves, fibrous tissues, blood vessels, or deep skin tissues. Secondary bone cancer is cancer that spreads to the bone from another part of the body (such as the prostate, breast, or lung). RISK FACTORS When sarcomas start on the arms or legs, most people simply notice a lump that has grown over a period of time (weeks to months). It can be painful, but generally, it doesn't hurt. More than half of sarcomas begin in an arm or leg. Studies have shown that the following are risk factors for sarcoma: Radiation exposure: Patients might develop sarcomas from radiation given to treat other cancers, like breast cancer or lymphoma. The sarcoma often starts in the area of the body that had been treated with radiation. The average time between radiation exposure and diagnosis of a sarcoma is about 10 years. Radiation exposure accounts for less than 5% of sarcomas. Genetic syndromes: Certain inherited conditions increase a person's risk of developing soft tissue sarcomas. Damaged lymph system: Lymph is a clear fluid containing immune system cells that is transported throughout the body by a series of lymph vessels. These vessels connect lymph nodes (small bean-shaped collections of immune system cells). When lymph nodes have been removed by surgery or damaged by radiation therapy, lymph fluid can build up. This is called lymphedema. In other parts of the world, severe lymphedema (a condition called elephantiasis) is sometimes caused by infection with a parasite that blocks lymph vessels. Lymphangiosarcoma (a malignant tumor that develops in lymph vessels) is a very rare complication of chronic lymphedema. Chemicals: Exposure to vinyl chloride (a chemical used in making plastics) is a risk factor for developing sarcomas of the liver, but it has not been proven to cause soft tissue sarcomas. Exposure to dioxin and to herbicides that contain phenoxyacetic acid at high doses (farm workers work closely with these chemicals) may also be risk factors, but this is not known for certain. There is no evidence that herbicides (weed killers) or insecticides, at levels encountered by the general public, cause sarcomas. When sarcomas grow in the retroperitoneum (the back wall inside the abdomen), the symptoms they cause are more often caused by other problems. Sometimes the tumors cause pain. They may also cause blockage or bleeding of the stomach or bowels. They may grow large enough for the tumor to be felt in the abdomen. About 20% of sarcomas begin in the abdomen (stomach) area. Sarcomas can also begin on the outside of the chest or abdomen (about 10%) or in the head or neck area (around 10%). SYMPTOMS If you have any of the following problems, see a doctor right away: A new lump or a lump that is growing anywhere on your body Abdominal pain that is getting worse Blood in your stool or vomiting Black, tarry stools (when bleeding happens in the stomach or bowels, the blood isn't always red, and it may make the stool look very black and tarry) T ESTICULAR don’t know how often CIS becomes true (invasive) cancer, it isn’t clear that treating CIS is a good idea. Some experts think that it may be better to wait and see if the disease gets worse or becomes a true cancer. This could allow many men with CIS to avoid the risks and side effects of treatment. CANCER Testicular Cancer is cancer that forms in tissues of one or both testicles. It is most common in young or middle-aged men. Most testicular cancers begin in germ cells (cells that make sperm) and are called testicular germ cell tumors. Cancer of the other testicle: Men who have been cured of cancer in one testicle have an increased risk (about a 3% to 4% chance) of getting cancer in the other testicle. Age: Nine out of 10 cases of testicular cancers occur in men between the ages of 20 and 54. Race and ethnicity: White American men are about 5 times more likely to get testicular cancer than are AfricanAmerican men. Whites have more than 3 times the risk of Asian-American and American Indian men. The risk for Hispanics falls between that of Asians and non-Hispanic whites. The reason for these differences is not known. Body size: Some studies have that the risk of testicular cancer is somewhat higher in tall men but other studies have not shown a link. RISK FACTORS Studies have shown that the following are risk factors for testicular cancer: Undescended testicle: One of the main risk factors for testicular cancer is a problem called cryptorchidism, or undescended testicle(s). Before birth, the testicles normally develop in the belly of the fetus and then move down (descend) into the scrotum before birth. But in about 3% of boys, the testicles do not move into the scrotum. Sometimes the testicle stays inside the belly. In other cases, the testicle starts to come down, but gets stuck in the groin. Family history: A family history of testicular cancer increases the risk. If a man has the disease, there is a slight risk that his brothers or sons may also get it. But very few cases of testicular cancer are actually found in families. HIV infection: There is some evidence that men infected with HIV (human immunodeficiency virus) have an increased risk of testicular cancer. This may be especially true for men who have AIDS. No other infections have been shown to increase testicular cancer risk. CIS (carcinoma in situ): It isn't clear how often CIS in the testicles becomes cancer. It is sometimes found when a man is tested for infertility. It may also be found when a man has a testicle removed because of cryptorchidism. Radiation or surgery (to remove the testicle) is used to treat CIS. Since we SYMPTOMS In most cases of testicular cancer, the man has a lump on a testicle or notices that the testicle is swollen or larger. Most of the time there is no pain. Men with testicular cancer may also notice a feeling of heaviness or aching in the lower belly or scrotum. In rare cases, men with germ cell cancer notice their breasts are sore or have gotten bigger. This happens because some germ cell tumors give off high levels of a hormone called human chorionic gonadotropin (HCG), which causes the breasts to grow. Blood tests can measure HCG levels. These tests are important in finding, staging, and follow-up of some testicular cancers. T HYROID CANCER Thyroid Cancer is cancer that forms in the thyroid gland (an organ at the base of the throat that makes hormones that help control heart rate, blood pressure, body temperature, and weight). Four main types of thyroid cancer are papillary, follicular, medullary, and anaplastic thyroid cancer. The four types are based on how the cancer cells look under a microscope. Family history of goiters or colon growths: A small number of people with a family history of having goiters (swollen thyroids) with multiple thyroid nodules are at risk for developing papillary thyroid cancer. Also, a small number of people with a family history of having multiple growths on the inside of the colon or rectum (familial polyposis) are at risk for developing papillary thyroid cancer. Personal history: People with a goiter or benign thyroid nodules have an increased risk of thyroid cancer. Being female: In the United States, women are almost three times more likely than men to develop thyroid cancer. Iodine: Iodine is a substance found in shellfish and iodized salt. Scientists are studying iodine as a possible risk factor for thyroid cancer. Too little iodine in the diet may increase the risk of follicular thyroid cancer. However, other studies show that too much iodine in the diet may increase the risk of papillary thyroid cancer. More studies are needed to know whether iodine is a risk factor. RISK FACTORS Studies have found the following risk factors for thyroid cancer: Radiation: People exposed to high levels of radiation are much more likely than others to develop papillary or follicular thyroid cancer. One important source of radiation exposure is treatment with x-rays. Between the 1920s and the 1950s, doctors used high-dose x-rays to treat children who had enlarged tonsils, acne, and other problems affecting the head and neck. Later, scientists found that some people who had received this kind of treatment developed thyroid cancer. Family history of medullary thyroid cancer: Medullary thyroid cancer sometimes runs in families. A change in a gene called RET can be passed from parent to child. Nearly everyone with the changed RET gene develops medullary thyroid cancer. The disease occurs alone as familial medullary thyroid cancer or with other cancers as multiple endocrine neoplasia (MEN) syndrome. A blood test can detect the changed RET gene. If it's found in a person with medullary thyroid cancer, the doctor may suggest that family members be tested. For those who have the changed gene, the doctor may recommend frequent lab tests or surgery to remove the thyroid before cancer develops. SYMPTOMS Early thyroid cancer often does not have symptoms. But as the cancer grows, symptoms may include: A lump in the front of the neck Hoarseness or voice changes Swollen lymph nodes in the neck Trouble swallowing or breathing Pain in the throat or neck that does not go away **This information is not intended to substitute for the advice of, and treatment by, a physician. Contact your doctor for any questions or concerns you may have, including those related to symptoms and diagnosis of a disease. Additionally, the symptoms listed here are not necessarily indicative of cancer; another health problem could be the cause. Therefore, if you have any of these symptoms, you should tell your doctor so problems can be diagnosed and treated. The information contained herein was obtained from the National Cancer Institute and the American Cancer Society.