OSTEOARTHRITIS
advertisement

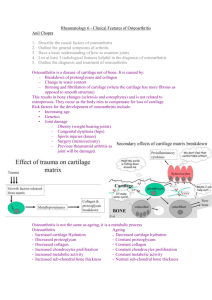
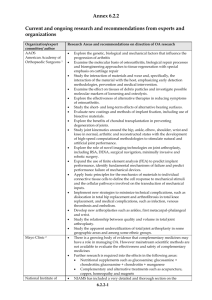
What is Osteoarthritis? Osteoarthritis (OA) is a slowly progressive joint disease that is characterized by a break down in cartilage. Cartilage is a flexible, connective tissue that protects the ends of bones from rubbing against each other. As cartilage breaks down, the bone starts to change shape. Progressive cartilage degeneration can cause the bone to curve inward (also known as “knock knees”) or outward (also known as “bow-legged”). Bone spurs can also form when cartilage breaks down. Bone spurs are bony growths that form on normal bone in response to pressure, rubbing, and chronic stress. Bone spurs occur along the edge of the joint and cause pain and swelling if it presses on other bones or soft tissues. Unlike other forms of arthritis including rheumatoid arthritis and systemic lupus, osteoarthritis only affects the joints and does not affect other organs in the body. The joints that are most affected by osteoarthritis are the hands, spine, hips, and knees. Symptoms of osteoarthritis: Joint pain or stiffness Warmth around joint or swelling Grinding sounds in the joints Decreased range of motion in the joints Popping or locking in the joint Weakness or feeling that the joint will “buckle” Worsening joint pain with repetitive use or after long periods of inactivity (sitting in a movie theater). Worsening joint pain with weather changes (colder temperatures and rainy conditions) Symptoms vary greatly between people. Some may have little to no symptoms despite having a severely degenerated joint on X-ray, while others may be completely debilitated. Pain may be intermittent or constant. Risk factors for osteoarthritis include older age (most commonly affects middle aged and elderly people), obesity, genetics (having family members with osteoarthritis), overuse, or trauma to certain joints (including injury or repeated joint surgeries). Diagnosis for osteoarthritis involve gathering a complete medical history, physical examination, X-rays, and possibly laboratory tests to rule out diseases or other types of arthritis that cause similar symptoms. X-rays will show narrowing of the joint space, changes in the shape of the bone, bone spurs, fluid in the joint, or other abnormalities. Treatments for osteoarthritis include slowing the progression of the degeneration, managing pain and swelling, improving range of motion and joint function, and improving strength. There is no cure for osteoarthritis so treatment focuses on improving symptoms and slowing down further deterioration. Nonsurgical treatments include: Lifestyle modifications: weight loss, avoiding activities that aggravate pain, staying active - switch to low-impact exercises such as aerobics, bicycling and swimming, take breaks from prolonged sitting or standing, and use good posture to take stress off of your joints. Medications: o Analgesics are used for mild-moderate pain like acetaminophen (Tylenol). o Topical analgesics are creams and rubs that can be applied to the painful area. Examples are Voltaren gel or capsaicin cream. o Non-steroidal anti-inflammatory (NSAID) drugs are used to reduce inflammation. Examples of NSAIDs include aspirin, ibuprofen, ketoprofen, naproxen, naproxen sodium and meloxicam. o Cox-2 drugs are targeted NSAIDs that don’t cause the stomach irritation associated with traditional NSAIDs. Examples of cox-2 drugs are celecoxib (Celebrex) and valdecoxib (Bextra). o Corticosteroids are used to reduce pain and swelling. o Dietary supplements like glucosamine and chondroitin sulfate are used to reduce arthritis pain. Physical therapy: to improve range of motion, improve joint flexibility, improve strength, and improve ambulation (ability to walk). Supportive or assistive devices: to improve stability in joint and improve ambulation. These include braces, splints, elastic bandages, canes, crutches, and walkers. Injections: viscosupplement injections (replacing lubrication into joint to reduce friction between bones), corticosteroid injections to improve pain and swelling, and platelet rich plasma (PRP) injections to accelerate tissue and wound healing within the joint. If conservative treatment fails, surgery may be an option. The decision to treat surgically depends on the age of the person, the condition of the joint, and the extent of the osteoarthritis. Surgical treatments include: Arthroscopy: A surgeon uses a flexible, fiberoptic instrument (arthroscope) to make several small incisions around the joint to remove bone spurs, cysts, damaged lining, or loose fragments. Osteotomy: The long bones of the arm or leg are realigned to take pressure off of the joint. Joint fusion: A surgeon eliminates the joint by fastening together the ends of the bone (fusion). Pins, plates, screws, or rods may hold bones in place while they heal. This procedure eliminates the joint's flexibility. Joint replacement: A surgeon removes parts of the bones and creates an artificial joint with metal or plastic components (total joint replacement or arthroplasty). References: Osteoarthritis. American Academy of Orthopaedic Surgeons. http://orthoinfo.aaos.org/topic.cfm?topic=a00227. Accessed January 24, 2012 Osteoarthritis. Arthritis Foundation. http://www.arthritis.org/disease-center.php?disease_id=32&df=treatments. Accessed January 24, 2012. REVISED 1/31/2012