Regulation of gastric secretion and the role of - PBL-J-2015
advertisement
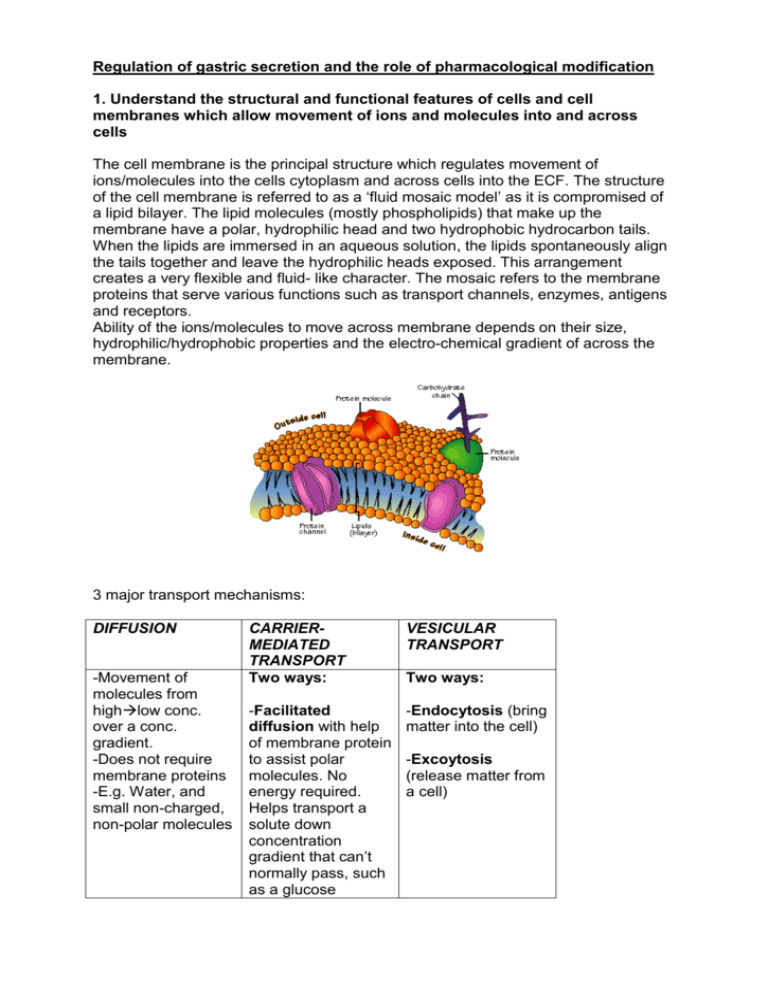
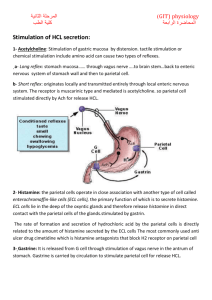
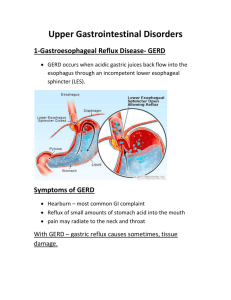
Regulation of gastric secretion and the role of pharmacological modification 1. Understand the structural and functional features of cells and cell membranes which allow movement of ions and molecules into and across cells The cell membrane is the principal structure which regulates movement of ions/molecules into the cells cytoplasm and across cells into the ECF. The structure of the cell membrane is referred to as a ‘fluid mosaic model’ as it is compromised of a lipid bilayer. The lipid molecules (mostly phospholipids) that make up the membrane have a polar, hydrophilic head and two hydrophobic hydrocarbon tails. When the lipids are immersed in an aqueous solution, the lipids spontaneously align the tails together and leave the hydrophilic heads exposed. This arrangement creates a very flexible and fluid- like character. The mosaic refers to the membrane proteins that serve various functions such as transport channels, enzymes, antigens and receptors. Ability of the ions/molecules to move across membrane depends on their size, hydrophilic/hydrophobic properties and the electro-chemical gradient of across the membrane. 3 major transport mechanisms: DIFFUSION -Movement of molecules from highlow conc. over a conc. gradient. -Does not require membrane proteins -E.g. Water, and small non-charged, non-polar molecules CARRIERMEDIATED TRANSPORT Two ways: VESICULAR TRANSPORT -Facilitated diffusion with help of membrane protein to assist polar molecules. No energy required. Helps transport a solute down concentration gradient that can’t normally pass, such as a glucose -Endocytosis (bring matter into the cell) Two ways: -Excoytosis (release matter from a cell) molecule. -Active transport. ATP energy dependent as moving molecule up its concentration gradient. For eg the sodium-potassium pump. 2. Describe in outline the hormonal and nervous control of the stomach Good animation: http://highered.mcgrawhill.com/sites/0072507470/student_view0/chapter24/animation__three_phases_of_gastr ic_secretion.html Stimuli acting at 2 distinct sites (head, stomach and small intestine) provoke or inhibit gastric secretory activity in the three phases of gastric secretion. The effector site is the stomach in all cases and the three stages once initiated can work concurrently: Phase 1: Cephalic -occurs before food enters stomach preparing it for food -few minutes long -triggered by aroma/taste/site of food -Input to olfactory receptorspreganglionic fibres in vagus nerve stomach glands -stimulates mucous for pepsinogen and gastric acid production Phase 2: Gastric -initiated when food enters the stomach in 2 ways: 1. Stretching the stomach 2. Raising pH of contents -stretching activates myenteric and vagovagal reflexes stimulating gastric secretion -also stimulated by Ach, histamine and gastrin -3-4 hours long Phase 3: Intestinal -duodenal response to chyme by moderating gastric activity by hormones and nervous reflexes -duodenum initially enhances gastric secretion but then inhibits it in two ways: 1. acid and semidigested fats in the duodenum trigger an enterogastric reflex which sends inhibitory signals to stomach. 2. secretin, GIP and CCK hormones also inhibit gastric secretion and motility allowing duodenum to process chyme already in it 3. Identify the roles of gastrin, histamine, secretin, gastric inhibitory peptide, and acetylcholine in control of gastric acid secretion and motility Hormone/neurotransmitter Target organ Gastrin Mainly stomach but some effect on small intestine, ileocecal valve and large intestine Activity Stomach: ↑ acid secretion, ↑ gastric motility (stomach emptying). ↑ enzyme secretion Small Intestine: ↑ gastric motility ileocecal valve: relaxes valve Large intestine: ↑ gastric motility Histamine stomach Secretin Stomach, pancreas and liver ↑ acid secretion and ↑ blood flow Stomach: ↓ acid secretion and ↓ gastric emptying Pancreas:: ↑ pancreatic fluid & bicarbonate secretion Gastric inhibitory peptide Stomach Acetylcholine Stomach liver: ↑ bile output ↑ insulin release ↓ acid secretion ↓ gastric motility ↑ acid secretion ↑ blood flow ↑ mucus secretion ↑ bicarbonate secretion 3. Outline the site and mechanism of action of the H2 receptor antagonists -H2 receptor antagonists work on the histamine receptors in the stomach mucosa to effectively reduce HCL acid secretion by parietal cells by up to 90%. These drugs compete with histamine for H2 receptors in a reversible reaction, so when their use is withdrawn acid secretion will reoccur and affect patients with history of duodenal ulcers. -Effective to alter basal acid secretion and secretion induced by food either anticipation (vagal) and food consumption. -Most prominent effect however on basal acid secretion. 5. Indicate other sites for pharmacological intervention in peptic ulcer disease (proton pump inhibitors, antacids) Proton pump inhibitors -Blocks H+/K+ ATPase on parietal cells inhibiting gastric acid secretion at the terminal stage. -Inhibits both basal and stimulated acid secretion. -Faster acting and more effective than H2 antagonists. Antacids -These are weak bases that act by neutralising gastric acid in the lumen of the esophagus, stomach and duodenum. They are used to relieve gastric pain and cell erosion caused by excessive acid secretion. -Most commonly used and effective is magnesium hydroxide Prostaglandins -Prostaglandins produced in the gastric and intestinal mucosa are effective in reducing acid secretion. Prostaglandins also protect deeper mucosal cells from damage. -Prostaglandin analogues (misoprostol) inhibit histamine-mediated stimulation of acid secretion. However, they are clinically mainly used to prevent gastric damage from chronic use of NSAIDS. Muscarinic receptor antagonists -Muscarinic receptor antagonists reduces the activity of the muscarinic acetylcholine receptor (namely M2) by competitively blocking the receptor site from Ach. -M2 receptors found on many locations within the gastrointestinal tract).