Chapter 16: THE CARDIOVASCULAR SYSTEM
advertisement

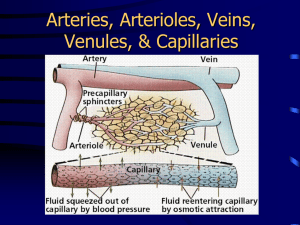
Name: __KEY__________________________________________ Period: ____ Chapter 16: THE CARDIOVASCULAR SYSTEM-BLOOD vessels and circulation I. BLOOD VESSEL STRUCTURE AND FUNCTION- page 391 OBJ: Compare the structure and function of the different types of blood vessels Describe how substances enter and leave the blood in capillaries. Explain how venous blood returns to the heart. Five types of blood vessels: (1) _Arteries_Carry blood away from the heart to body tissues Two large arteries are: _aorta_ and _pulmonary trunk_ branch out from the heart go to small arteries (2) _Arterioles_Small arteries found in organs, branch out into capillaries (3) _Capillaries_Microscopic vessels that branch off of arterioles in organs (4) _Veins_ Small veins formed by groups of capillaries within a tissue that reunite (5) _Venules_Larger vessels formed by merging venules; convey blood from tissues back to the heart The average adult has over _60,000_ miles of blood vessels in their body. Systematic volume of blood in blood vessels at any given time during circulation: a. Systematic arteries and arterioles _15_% b. Systematic veins and venules _60_% c. Systematic capillaries _5_% d. Pulmonary blood vessels _12_% e. Heart chambers _8_% What is the function of blood reservoirs? _Veins and venules contain so much blood, thus certain veins serve as blood reservoirs from which stored blood can be diverted to other parts of the body_ B. Arteries and Arterioles- page 391 1. Walls of arteries have three layers of tissue surrounding a hollow space through which the blood flows called the _lumen_. 2. Three layers surrounding the lumen: a. _Tunica interna_: inner layer; endothelium composed of simple squamous epithelium, a basement membrane, and an elastic tissue (internal elastic lamina) b. _Tunica media_: middle layer; smooth muscle and elastic tissue c. _Tunica externa_: outer layer; mainly elastic and collagen fibers 3. _Vasoconstriction_: decrease in the size of the lumen of a blood vessel. Cause: increase in sympathetic stimulation that causes smooth muscle to contract, squeezing vessel walls and narrowing lumen. Increases blood pressure…. 4. _Vasodilation_: increase in the size of the lumen of a blood vessel. Cause: decrease in sympathetic stimulation that causes smooth muscle to relax, expanding vessel walls and widening lumen. Decreases blood pressure… 5. _Elastic arteries_: largest-diameter arteries; a lot of elastic fiber in middle layer, walls pretty thin; propel blood onward when ventricles relaxed. Elasticity needed to accommodate surge of blood coming from heart as it pumps. 6. _Muscular arteries_: medium-sized arteries; contain more smooth muscle; capable of greater vasoconstriction and vasodilation to adjust rate of blood flow. 7. _Arteriole_: very small artery; delivers blood to capillaries; regulate blood flow from arteries to capillaries (vasoconstriction = blood flow artery to capillary restricted; vasodilation = flow is increased) C. Capillaries- pages 391-394 Connection between _arterioles_ and _venules_. Known as _exchange vessels_ because permit exchange of nutrients and waste between body cells and blood. Extensive capillary networks present in: _muscles, liver, kidneys, nervous system_ Have high metabolic requirements… NOT present in: _cornea and lens of the eye, nails, hair follicles, cuticles, cartilage_ Have low metabolic requirements… 1. Structure of Capillaries A. Walls consist of: _single layer of endothelial cells_Thus substances pass across them easily… B. _Precapillary sphincters_: rings of smooth muscle at meeting point of capillary to arteriole; along with smooth muscle fibers in arterioles regulate flow of blood (when sphincters relaxed = more blood flows; when sphincters contracted= less blood flow) 2. Capillary Exchange A. Two main methods of exchange: (1) _Diffusion_ a. _Oxygen_ and _nutrients_: down the gradient into interstitial fluid and then into body cells b. _Carbon dioxide_ and _waste_: down the gradient from interstitial fluids into the blood for removal c. _glucose_ d. _amino acids_ e. _hormones_ _Sinusoids_: smallest blood vessels in the liver have very large gaps in between their endothelial cells to allow proteins (fibrinogen, main clotting protein, and albumin) to enter bloodstream _Blood-brain barrier_: tightness of endothelial layer found in brain; allows only a few substances to enter and leave (2) _Bulk Flow_ (Filtration and Reabsorption) Passive process from area of higher pressure to lower pressure, for as long as a pressure differs occurs a. _Ions_, _molecules_ or _particles_ in a fluid; move together, same direction b. Two opposing pressures = _capillary blood pressure_ and _blood colloid osmotic pressure_ _Capillary blood pressure_: pressure of blood against capillary walls, “pushes” fluid out of capillaries into interstitial fluid _Filtration_: movement of water and solutes from capillaries to interstitial fluid _Blood colloid osmotic pressure_: opposing pressure “pulls” fluid into capillaries _Reabsorption_: movement of water and solutes from interstitial fluid into blood capillaries _Autoregulation_: ability of a tissue to automatically adjust its blood flow to match its metabolic demands 2 D. Venules and Veins- pages 394-395 1. Structure of Venules and Veins A. _Venules_: little veins; walls thinner at capillary end, thicker as they progress toward heart B. _Veins_: structural similar to arteries; middle and inner layers thinner than arteries, outer layers are the thickest Lumen of veins wider than that of corresponding artery Inner layer forms valves to prevent backflow of blood Blood flows out of a vein slowly and more rapidly out of an artery C. What causes varicose veins? _Weak venous valves, gravity forces blood backwards through the valve thus increasing venous blood pressure that pushes the vein’s wall outward. Veins receive repeated overloads, walls lose elasticity, stretch become flabby_ 2. Venous Return A. Volume of blood flowing back to heart through veins, occurs through pressure generated in three ways: (1) _Contractions of the heart_BP generated by contraction of heart’s ventricles and measured in millimeters of mercury (Hg) (2) _Skeletal muscle pump_Locomotory activity promotes venous return, i.e. walking, running. Veins in legs and arms have one-way valves that direct flow away from limb to the heart. Muscles compress (contraction phase) the veins propels blood forward through distal (upper) valves. Muscles decompress (relaxation phase) proximal valves open, blood flows into and fills venous segment. Both of these work together to create enough pressure to propel blood to heart. (3) _Respiratory pump_Also based on alternating compression and decompression of veins. You inhale, diaphragm moves downward = decrease in pressure in thoracic cavity, abdominal veins are compressed, thus blood moves from compressed abdominal veins to decompressed thoracic veins and then into right atrium of heart. You exhale; valves in veins prevent backflow of blood from thoracic to abdominal veins. II. BLOOD FLOW THROUGH BLOOD VESSELS- page 396 OBJ: Define blood pressure and describe how it varies throughout the systematic circulation. Identify the factors that affect blood pressure and vascular resistance. Describe how blood pressure and blood flow are regulated. A. Blood Pressure- page 396 1. Blood flows from areas of _higher_ pressure to areas of _lower_ pressure, the greater the pressure difference the greater the _blood flow_. 2. What generates blood pressure (BP)? _contraction of the ventricles_ 3. What is blood pressure? _pressure exerted by blood on the walls of a blood vessel; highest in the aorta and large systemic arteries; rises to 120mmHg systolic (contraction) and falls to 80mmHg diastolic (relaxation)_ 4. Systolic measures _ maximum arterial pressure occurring during contraction of the left ventricle of the heart_ Average = _120_mm Hg High end begins = _140_ mmHg 5. Diastolic measures _arterial pressure during the interval between heartbeats_ Average = _80_mm Hg High end begins = _90_ mmHg B. Resistance- pages 396-397 1. _Vascular resistance_: opposition to blood flow due to friction between blood and the walls of blood vessels Increase in vascular resistance = increase in BP 3 Decrease in vascular resistance = decease in BP 2. Vascular resistance is dependent upon: a. _Size of the blood vessel (lumen)_ Smaller means greater resistance to blood flow; alternates between vasoconstriction and vasodilation b. _Blood viscosity_ Ratio of RBCs to plasma volume Higher viscosity = higher resistance c. _Total blood vessel length_ Resistance increase with total length Longer the length = greater contact between vessel wall and blood C. Regulation of Blood Pressure and Blood Flow- pages 397-399 Negative feedback systems control BP and blood flow 1. Role of the Cardiovascular Center a. _Cardiovascular Center (CV) in medulla oblongata_: regulates heart rate and stroke volume b. The diagram below shows how input to the CV affects the output of effectors 2. Hormonal Regulation of Blood Pressure and Blood Flow a. _Renin-angiotensin-aldosterone _(RAA system): if blood volume falls or blood flow to kidneys decreases, RAA system works to raise BP through vasoconstriction and increase reabsorption of sodium and water to increase blood volume b. _Epinephrine and norepinephrine_: respond to sympathetic stimulation, adrenal medulla releases these to increase cardiac output by increasing the rate and force of heart contractions; causes vasoconstriction c. _Antidiuretic hormone (ADH)_: produced by hypothalamus, released by posterior pituitary in response to dehydration or decreased blood volume; causes vasoconstriction to increase BP; thus ADH is known as vasopressin d. _Atrial natriuretic peptide (ANP)_: released by cells in atria of heart; lowers BP, cause vasodilation, promotes loss of salt and water in urine, thus reducing blood volume III. CIRCULATORY ROUTES- pages 400, 416-417 OBJ: Understand the overall systemic circulation route and pulmonary circulation route. Describe the function of hepatic portal circulation. Blood vessels are organized in circulatory routes that carry blood throughout the body. Two main circulatory routes: systemic and pulmonary… A. Systemic Circulation- page 400, Pulmonary Circulation- page 416, and Hepatic Portal Circulation- pages 416-417 1. Includes: _arteries_ and _arterioles_ 2. Carries blood containing _oxygen_ and _nutrients_ from left ventricle to systemic capillaries throughout body 3. Also the _veins_ and _venules_ that carry blood containing _carbon dioxide_ and _waste_ to the right atrium. 4. What color is blood that leaves the aorta and travels through systemic arteries? _bright red 5. Blood then moves through the capillaries, loses _oxygen_ and takes on _carbon dioxide_ becoming _dark red_ in color. 6. Examine the diagram below to find the beginning and the ending of systemic circulation and the route of pulmonary circulation. 4 Systemic Circulation: (1) All systemic arteries branch off of aorta, which arises from left ventricle of the heart carrying oxygenated blood to all parts of the body. (2) Deoxygenated blood returns to the heart through systemic veins; superior vena cava to inferior vena cava (coronary sinus) to right atrium. Pulmonary Circulation: (3) When deoxygenated blood returns to the heart from the systemic route, it is pumped out the right ventricle through the pulmonary artery into the right lung where it loses CO2. (4) Blood moves into the left lung, picks up O2, and then returns to left atrium of heart, to once again go through systemic circulation. Hepatic Portal Circulation: (5) Hepatic portal vein carries blood from one capillary network to another, namely from the GI to the liver. In the liver substances from the GI tract are processed before pushed out the hepatic vein into the inferior vena cava for circulation throughout the body. Fetal circulation also introduced here!! IV. CHECKING CIRCULATION- page 400 OBJ: Explain how pulse and blood pressure are measured. A. Pulse- page 400 1. How does a pulse occur? _Through alternate expansion and elastic recoil of an artery after each contraction and relaxation of the left ventricle_ 2. What is the normal range for pulse rate/heart rate? _70 to 80 beats per minute at rest_ 3. _Tachycardia_: rapid resting heart or pulse rate over 100 beats/minute. 4. _Bradycardia_: slow resting heart or pulse rate under 60 beats/minute. B. Measurement of Blood Pressure- page 400 1. What does blood pressure refer to in clinical terms? _pressure in the arteries generated by the left ventricle during systole and the pressure remaining in the arteries when the ventricle is in diastole_ 2. Where blood pressure is usually measured? _brachial artery in the left arm_ 3. What type of device is used to measure blood pressure? _sphygmomanometer_ 4. What is meant by systole? _contraction of the heart_ 5. The first sound heard corresponds to _systolic blood pressure (SBP)_, force with which blood is pushing against arterial walls during ventricular contraction. 6. The last faint sound hear corresponds to _diastolic blood pressure (DBP)_, force exerted by the remaining blood in arteries during ventricular relaxation. 7. Normal blood pressure of a young adult male is _120_ mmHg systolic and _80_ mmHg diastolic. 8. In females the blood pressure is _8_ to _10_mmHg lower. 5