MVA Sample Protocols
advertisement

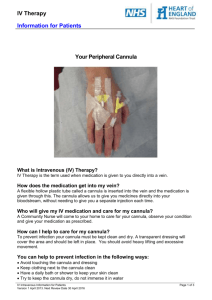
MM-TI Miscarriage Management Training Initiative Sample Protocol MVA for Early Pregnancy Miscarriage Management POLICY: Purpose: To outline staff and provider responsibility in the performance of manual vacuum aspiration for early pregnancy miscarriage management or endometrial biopsy. LEVEL: Intradependent SUPPORTIVE DATA: Manual vacuum aspiration (MVA) is a safe, relatively painless, and cost-effective diagnostic and therapeutic means of evacuating the uterus during early pregnancy miscarriage or for evaluating the endometrium for abnormal uterine bleeding, infertility, and malignancy. INDICATIONS: A) Treatment/completion of incomplete spontaneous abortion in first trimester (<13 weeks) 1) Ensures POC are fully evacuated 2) Controls hemorrhage 3) Evacuates post-abortal hematometra B) See policy #4529.00 for outline of indications for endometrial biopsy CAUTION/CONTRAINDICATION: A) Coagulation disorders, anticoagulant drug therapy B) Uterine anomalies C) Pelvic inflammatory disease/cervicitis D) Extreme anxiety E) Any condition causing patient to be medically unstable F) Cervical stenosis G) Endometrial biopsy also contraindicated in pregnancy EQUIPMENT: Sterile gloves, mask with face shield, fluid resistant gown Vaginal speculum (sterile), light source Lubricant Antiseptic solution (povidone-iodine) or Benzalkonium Chloride for iodine allergy, small Sterile bowl for iodine, sterile gauze Manual vacuum aspirator Cannula for aspirator (4-12 mm) Cervical dilator (4-12 mm) Tenaculum, ring forceps Sterile syringe and needle, 1% Lidocaine, Hurricaine spray Long hemostat Sterile basin for emptying aspirator Miscarriage Management-Training Initiative Strainer Glass bowl and backlight for examining uterine contents Container and formalin for pathology Monsel’s solution/Gelfoam available Cytotec (Misoprostol), Methergine, Ibuprofen Rhogam if indicated STEPS PREPARATION OF THE PATIENT: A) Verify patient name and date of birth. B) Take vital signs and weight, complete nursing intake note in medical record. C) Have patient empty bladder and obtain urine pregnancy test, if indicated. D) Explain procedure to patient. Patient should have opportunity to read “Miscarriage” handout if not already read. E) Assure that patient has ride home. F) Administer NSAID as ordered (optimally one hour prior to procedure). G) Review chart for results of Rh factor and prepare Rhogam if indicated (50 mcg). Perform in-house hematocrit if ordered. H) Once consent is obtained, prepare patient for vaginal exam; assist patient into dorsal lithotomy position and drape with draw sheet. PROVIDER RESPONSIBILITIES: A) Obtain informed consent and perform procedural verification. B) Perform bimanual exam noting size and position of uterus. May perform ultrasound. C) Place speculum and perform antiseptic prep and paracervical block. D) Inform patient that she may experience cramping because of dilation of the cervix during the procedure. E) Dilate cervix to admit suction cannula of the appropriate size, usually equal to estimated gestational age of Miscarriage Management-Training Initiative KEY POINTS Fever may be a reason to delay procedure. Pregnancy test only necessary for endometrial biopsy. Ideally, patient will have appt. prior to procedure to meet with social worker and/or behavioral health services, so as to deal with issues of loss. If patient is not pre-sedated, and is stable following endometrial biopsy, she should be able to drive self. May also pre-medicate with Ativan 1 hr. pre-procedure (RX to pharmacy, no Ativan kept on site) Informed consent should be obtained prior to any pre-procedure sedation. Ascertain patient’s drug sensitivity and/or history of allergy to skin prep, materials, and anesthetics prior to administration of local anesthetic. Use size 4 dilator and suction cannula for endometrial biopsy. i.e. 7 or 8mm dilator and cannula for 7 weeks gestation. pregnancy or one size larger. F) Perform MVA by generating suction before insertion of suction cannula. G) Place suction cannula into the cervical os and move the cannula slowly into the uterine cavity until it touches the fundus; then withdraw it slightly. H) Release the buttons on the aspirator to transfer the vacuum through the cannula into the uterus. I) For uterine evacuation, evacuate the contents of the uterus by rotating the cannula 180 degrees in each direction while using a gentle in-andout motion. J) For endometrial biopsy, movement of the cannula gently back and forth along the anterior uterine wall, then rotating and taking a sample from the posterior uterine wall in same fashion should provide sufficient tissue for diagnosis. K) Empty syringe if needed and repeat until all uterine contents removed, usually 2-3 times. L) For endometrial biopsy, collect aspirated material in formalin and send specimen to pathology. M) For uterine evacuation, inspect aspirated tissue. If visual inspection is not conclusive, strain the tissue and put in water or vinegar in clear glass container and examine through backlight. Send to pathology if indicated. N) Order methergine/cytotec (misoprostol) if needed. O) Order Rhogam if indicated. POST PROCEDURE CARE: A) Ask the patient to remain supine for a few moments following the procedure. Place peri-pad. B) May elevate head of table after a few minutes; assess for vasovagal reaction. Offer fluids if not nauseated. C) Monitor BP every 15 minutes for minimum of 30 minutes, longer if unstable. Check amount of bleeding Miscarriage Management-Training Initiative If cannula becomes clogged, ease it back toward, but not through, the external cervical os. This movement will often unclog the cannula. If it does not, cannula can be removed and tissue removed with sterile forceps or gauze. Depress valve buttons and disconnect cannula from the aspirator while leaving cannula inserted through the cervical os. Signs that uterus is empty include red or pink foam without tissue passing through cannula, gritty sensation felt as cannula passes over the surface of the evacuated uterus, uterus contracts around or “grips” the cannula, and/or patient notes pain as uterus contracts Would you give one or the other, or both? at same intervals. D) Assess for painful uterine cramping. Communicate pain level to provider and document along with vital signs in medical record. E) If heavy bleeding is not observed and the vasovagal reaction (if it has occurred) has resolved, discharge the patient after 30 minutes. F) Review discharge instructions with patient/significant other. G) Patient to be contacted by provider or provider’s representative in 24 hrs. for phone follow-up. Patient to schedule follow-up appt. in 2 weeks. H) Dispose of aspirated contents per “Blood and Body Fluids Disposal” procedure, VMC Infection Control Manual I) Dispose of cannula per VMC guidelines. Aspirator should be disassembled, cleaned and sterilized, per VMC disinfection procedures. DOCUMENTATION A) Document procedure and patient’s tolerance. B) For uterine evacuation, document visual inspection of aspirated uterine contents C) Document vital signs and patient’s pain level, before, during and after procedure. D) Document that patient received discharge instructions and verbalized understanding, and plan for follow-up care. PATIENT EDUCATION A) The patient may resume sexual relations in one week, or after bleeding has stopped. If birth control is desired, sexual relations should wait until method of birth control is chosen. B) Daily activities may be resumed as soon as patient feels up to it, but strenuous activities should be delayed for several days following uterine evacuation. C) Pads should be used while bleeding Miscarriage Management-Training Initiative For endometrial biopsy, inform patient that she will be contacted by phone or mail within three weeks, of biopsy results. Follow-up in clinic not necessary unless patient is having problems. Patients may be allowed to take home products of conception if desired. High level disinfection using Cidex OPA is acceptable if sterilization is not feasible. For endometrial biopsy, sexual relations may be resumed earlier, in 3 days unless bleeding is heavier. is heavier, but tampons may be used after heavier bleeding lets up. D) Patient should report the following: 1) Fever with a temperature higher than 100.4 degrees F for more than 24 hours post procedure 2) Severe cramping not relieved by medication, especially more than 24 hrs. post-procedure 3) Bleeding and soaking through more than two maxi pads per hour, for two or more hours in a row. 4) Dizziness or syncope 5) Nausea, vomiting or diarrhea for more than 24 hours post procedure. 6) Overwhelming sadness or depression E) Give written aftercare instructions, including how to get help after hours. F) Provider to send in RX for antibiotic, Doxycycline 100 mg X 2 doses, take 1st dose with next meal, take 2nd dose following day with meal. Check allergies Is antibiotic given after endometrial biopsy as well? REFERENCES A) Valley Medical Center Clinic Network, Endometrial Biopsy Procedure, #4529.00, and related references B) Sarah Prager, MD, Department of Obstetrics and Gynecology, University of Washington C) IPAS Gynecological Aspiration System instruction manual, 4/07 Miscarriage Management-Training Initiative Miscarriage Management-Training Initiative