Maternity Strategy Annual Report
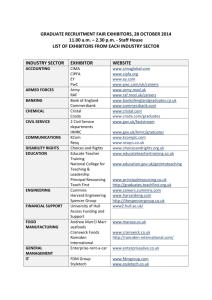
advertisement

Report to: Planning & Commissioning Committee Date of Meeting: 6th May 2015 Subject: Presented by: Maternity Services Commissioning Strategy Annual Report 2014/15 Natalie Robinson – Interim Commissioning Manager Author: Natalie Robinson – Interim Commissioning Manager STATUS OF THE REPORT: To approve x To endorse To ratify To discuss To consider For information To note PURPOSE OF REPORT: The purpose of the annual report is to provide the Planning & Commissioning Committee with a review of progress for Year 1 of the Hull Maternity Services Commissioning Strategy (2013 – 2018) and its associated work plan and thereby assurance on delivery of the NHS Hull CCG strategic objectives associated with the strategy. RECOMMENDATIONS: It is recommended that the Planning & Commissioning Committee : a) Note the content of this report b) Seeks assurance on the progress of the delivery of the work streams and initiatives within the Maternity Services Commissioning Strategy Year 1 (2014/15) work programme. c) Support and agree the contents of the Year 2 (2015/16) work plan and its associated actions and objectives REPORT EXEMPT FROM PUBLIC DISCLOSURE If yes, grounds for exemption (FOIA or DPA section reference) No x Yes CCG STRATEGIC OBJECTIVE (See guidance notes below) ASSURANCE FRAMEWORK SPECIFIC OBJECTIVE Short summary as to how the report links to the CCG’s strategic objectives (See guidance notes below) Short summary as to how the report adds assurance to the Assurance Framework The Maternity Services Commissioning Strategy is an identified initiative within The Children, Young People and Maternity Programme ‘Next Generation’ which is one of four transformational change programmes within the NHS Hull CCG This report provides assurance to the Planning & Commissioning Committee on the delivery of the Maternity Services Commissioning Strategy work-streams and initiatives. IMPLICATIONS: (summary of key implications, including risks, associated with the paper ), Resources are identified within the CCG Financial Plan for the initiatives within the Finance Children, Young People and Maternity Programme. HR None Quality Quality issues are addressed at initiative level. Safety Safety issues are addressed at initiative level. ENGAGEMENT: This paper presents work undertaken through the Maternity Services Forum which is responsible for taking forward the initiatives and projects related to this programme area. Members of the Maternity Services Forum have been consulted with and asked for input and feedback in relation to the content of this annual report and the development of the Year 2 (2015/16) work plan. There is an identified objective within the work plan that focuses on service user experience and engagement. LEGAL ISSUES: (Summarise key legal issues / legislation relevant to the report) None EQUALITY AND DIVERSITY ISSUES: (summary of impact, if any, of CCG’s duty to promote equality and diversity based on Equality Impact Analysis (EIA). All reports relating to new services, changes to existing services or CCG strategies / policies must have a valid EIA and will not be received by the Committee if this is not appended to the report) An Equality Impact Analysis/Assessment is not required for this report. Tick relevant box x An Equality Impact Analysis/Assessment has been completed and approved by the lead Director for Equality and Diversity. As a result of performing the analysis/assessment there are no actions arising from the analysis/assessment. An Equality Impact Analysis/Assessment has been completed and there are actions arising from the analysis/assessment and these are included in section xx in the enclosed report. THE NHS CONSTITUTION: (How the report supports the NHS Constitution) Objective No 1 Strategic Objective Specific Objective 2014/15 In 2020 we will work together better to enable the people of Hull to improve their own health, resilience, wellbeing and to achieve their aspirations for the future 2 Achievement of CCG balanced scorecard domains and strategic performance objectives Patients receive clinically commissioned, high quality services Patients and the public are actively engaged and involved The CCG has robust governance arrangements CCG plans are delivering better outcomes for patients The CCG has strong and robust leadership 21st Century Primary Care Workforce Next Generation 3 Other Strategic Objectives Integration Implementation of Better Care Fund and readiness for April 2015 Care closer to home Transform and redesign pathways in high volume (outpatient) specialties. Provide choice of services for patients Closer integration of services with hospital and primary care services working more closely together Community Hubs Development of a population based approach to commissioning to support community priorities based on x7 areas Single Care Navigator A principle of delivery Thriving communities, build communities ownership and resilience HULL MATERNITY COMMISSIONING STRATEGY (2013 – 2018) ANNUAL REPORT 2014/15 1. INTRODUCTION The purpose of this report is to provide the Planning & Commissioning Committee with an update on progress of the work being delivered through the Hull Maternity Commissioning Strategy (2013 - 2018) and progress against the year 1 workplan objectives, thereby providing assurance on delivery of the NHS Hull CCG strategic objectives associated with the children, young people and maternity programme. 2 BACKGROUND NHS Hull CCG has a strong focus on children and young people as the ‘next generation’. ‘Children and young people and maternity’ is one of the five service development work streams of the Hull 2020 Strategy and includes services from preconceptual care and maternity through to early years, education, learning and employment. The Maternity Services Commissioning Strategy sets out the strategic plans for NHS Hull Clinical Commissioning Group for the period April 2013 to March 2018. It is identified as an initiative within the children, young people and maternity programme. The overarching aim of the strategy is that maternity services commissioned by NHS Hull CCG will provide “high quality, evidence based and safe care, delivered at the right time, in the right place, by a properly planned, educated and trained workforce. Services will be integrated and care will be coordinated around the woman and her family, with service users reporting positive experience of the maternity care they have received”. The strategy has five key measurable outcomes that continue to be delivered through the Maternity Services Work Programme. 1. An improvement in maternal health – this includes improvements in the rates of early access to midwifery care, reduction in maternal obesity and rates of smoking. 2. A reduction in maternal mortality 3. A reduction in infant mortality 4. A reduction in infant morbidity 5. An improvement in women and their families’ experience of maternity services The Maternity Services Forum is a multi-disciplinary, multi-agency forum that brings together key stakeholders (commissioning, provider organisations and services and service users) in order to: contribute to the development and provision of high quality maternity services secure service user engagement and involvement, ensuring that the views of women and their families who use local maternity services are taken into account in the commissioning, delivery and review of such related services lead the delivery and monitoring of the NHS Hull CCG Maternity Services Commissioning Strategy Work Programme alongside other associated groups such as for example, the Smoking in Pregnancy Group and the Children’s Centre Strategic Group. To drive the delivery of NHS Hull CCG Maternity Services Commissioning Strategy Work Programme the Hull Maternity Services Forum meets quarterly. The forum is chaired by NHS Hull CCG. 3 INFORMATION During the period 2013/14 to March 2015 considerable progress has been made against the delivery of the NHS Hull CCG Maternity Services Commissioning Strategy Work Programme (2014-2015). Appendix A sets out the progress made against each of the key actions and objectives. 3.1 Achievements include: Agreement and sign off of the Hull and East Yorkshire Hospitals NHS Trust (HEYHT) maternity service specification for delivery of services up to 2017 Re-procurement of the “Doula Project” for a further four years (until 2019) which will support the training of 40 volunteers and support 160 pregnant women per year. Re-procurement of the “Peer support breastfeeding project” for a further four years (2019) which will support the recruitment of 50 volunteers and engage with approximately 2000 women each year (antenatal and postnatal) Implementation of CO2 monitoring at booking for all pregnant women, with direct referral into the Smoking in Pregnancy Service. Strengthened Perinatal Mental Health pathway through procurement of the “Let’s Talk” service, and the training and development of the health visitor and GP/Primary Care workforce. Investment in the HEYHT midwifery workforce resulting in recruitment of 12 midwives, reducing the birth to midwife ratio to from 1:35 (Nov 14) to1:32 (Jan 15) Hull City Council (CC) Public Health allocation of £100k over three years (20142017) to implement an integrated maternal healthy lifestyles plan. The plan includes the development of an “Us Mums to Be” and “Us Mums” brand supporting healthy eating and physical activity across the city. NHS Hull CCG commissioned a research study delivered by The University of Hull to determine if training assists primary care practitioners to effectively identify and manage Peri-mental Illness (PMI), This outcomes of the study will inform workforce development requirements and will support the development of a “Map of Medicine” A Protected Learning Time event which was held in March 2015 on “Bridging Primary Care and Maternity Care” The event was attended by over 120 health professionals and included presentations on stillbirth, managing medical elements of maternity care, perinatal mental health and healthy lifestyles. 3.2 Progress made against 5 key measurable outcomes 1. An improvement in maternal health – this includes improvements in the rates of early access to midwifery care, reduction in maternal obesity and rates of smoking. Table 1 evidences improvements in the number of women seen by a midwife or maternity healthcare professional by 12 weeks and 6 days of pregnancy. England 13/14 (Q1) 12/13 (Q3) 91.5% 91.8% Hull PCT/ NHS Hull CCG 95.9% 95.9% Table 1: Number of women seen by a midwife or maternity healthcare professional by 12 weeks and 6 days of pregnancy. Data Source: NHS England The city of Hull continues to be an outlier in performance in the reduction of women smoking at time of delivery (SATOD). Data as of Q3 of 2014/15 shows 20.3% of women smoking at time of delivery, compared to the England average of 11.5% (Q2 2014/15). The implementation of Breathe2025, the Still Care Bundle pilot and Hull CC’s reprocurement of Smoking Cessation services will support the drive for on-going improvement. The Yorkshire and Humber Strategic Clinical Network as part of its work on the development of a maternity dashboard have suggested a SATOD target of 11% or less for achievement by the end of 2015. Maternal Obesity continues to be of concern, in Q3 of 2014/15 24.9% of women seen at booking clinic had a BMI>30. It is difficult to put this data into national or regional context as reporting for this measure has not been routinely collected. The publication of the Maternity Services Data Set (MSDS) Information Standards notice requires Maternity Service to centrally submit this dataset which includes BMI from the 1 st May 2015. 2. A reduction in maternal mortality Due to the very small numbers of maternal deaths it is not possible to present the details in this report, that being said one maternal death is too many and there continues to be a drive to prevent any avoidable maternal deaths. Further to the recent publication of the HEYHT LSA Audit report from October 2014 and Dr Kirkup’s “Morecambe Bay Investigation Report” assurance is required regarding the local position and any required actions. 3. A reduction in infant mortality Table 2 shows the latest available data for infant mortality. As can be seen, whilst progress has been made and a reduction shown since 2008/10, Hull continues to have a higher rate in comparison to England. To date there has been a variable trend in the mortality rate, it is expected that the 2012/14 data set will be published in May 2015, until then no assumptions can be made of a sustained reduction. 2009/11 2008/10 2007/09 England Kingston Upon Hull 4.4 5.0 4.6 5.5 4.7 4.9 Table 2: Infant mortality rate per 1,000 live births Data source: HSCIC Indicator Portal There has been improvement in the reduction in the 3 year average crude rate of stillbirths in Hull, however the single year rate for 2013 (rate per 1,000 live births 6.4) is considerably higher than that of the England average (rate per 1,000 births 4.6) 2011/13 2010/12 2009/11 England Kingston Upon Hull 4.9 4.7 5.0 4.3 5.2 5.3 Table 3: Still births: crude rate, 3 year average Data source: HSCIC Indicator Portal 4. A reduction in infant morbidity This outcome measure should be seen in the overall wider strategic context of the maternity commissioning strategy. It is difficult to present a reduction in real data terms for infant morbidity. Morbidity statistics are available from a range of sources and refer to ill health within a specific population, in this case infants. A robust maternity JSNA will allow us to explore this data in more detail highlight any areas for concern. A number of the objectives in the work plan support an improvement in infant health and wellbeing including: improvement in pre conceptual care, breast feeding rates, reduction in smoking rates, increase the number of normal births etc. For both initiation of breastfeeding at time of delivery and women breastfeeding at 6-8 weeks NHS Hull CCG continues to be an outlier in performance in comparison to the England average. 14/15 Q2 14/15 Q1 13/14 Q4 13/14 Q3 13/14 Q2 Breastfeeding initiation % England NHS Hull Rank CCG 74.4% 62.6% 161/185 74.0% 63.1% 155/185 73.8% 63.1% 117/185 73.7% 63.0% 134/185 74.2% 62.3% 150/185 Breastfeeding at 6-8 weeks % England NHS Hull Rank CCG Data quality criteria not met Data quality criteria not met 46.2% 30.7% 65/116 45.7% 35.4% 79/116 45.7% 32.9% 88/116 Table 4: Breastfeeding rates at initiation and 6-8 weeks Data source: NHS England Action is required to address data quality reporting for breastfeeding at 6-8 weeks to provide assurance on performance. In 2013/14 (Year 1) Birth Preparation and Parent Education Services (BUMPS) delivered sessions to 926 clients (pregnant women and their partners) averaging 77 clients per month. NHS Hull CCG are working with BUMPS to agree a service development plan with stretch targets against all key performance indicators with the primary goal to improve access and uptake of the service in 2015/16 . 5. An improvement in women and their families’ experience of maternity services There is insufficient information and data available to provide assurance in any improvement in women and families experience of maternity care. This is highlighted as a key area for action in Year 2 of the work plan. There has been a continued poor response to the Friends and Family Test. Whilst the scores achieved are high, the response rates are so poor that no assurance can be gained. The latest results published (December 2014) show the following number of responses: How likely are you to recommend our antenatal service to friends and family – 78 responses How likely are you to recommend our labour ward/birthing unit to friends and family if they needed similar care or treatment – 12 responses How likely are you to recommend our postnatal ward to friends and family if they needed similar care or treatment – 12 responses How likely are you to recommend our postnatal community service to friends and family if they needed similar care or treatment – 16 responses 3.3 Summary and focus for year 2 (2015/16) Further improvement is still needed against the five measurable outcomes and in order to address the issues highlighted above. Appendix B sets out the Draft Year 2 Work Programme (2015 -2016). This will be continued to be led, delivered and monitored by the Hull Maternity Services Forum. There are a number of actions and objectives which have been carried forward and a strengthened focus on the following areas: The development a Maternity JSNA for Hull Reduce the number and rate of still births Improve access and outcomes from birth preparation and parent education services Improve service user experience and engagement Perinatal Mental Health Healthy lifestyles including a reduction in maternal obesity and smoking at time of delivery. 4. RECOMMENDATIONS It is recommended that the Planning & Commissioning Committee:a) Note the content of this report b) Seeks assurance on the progress of the delivery of the objectives within the Maternity Services Commissioning Strategy Year 1 work programme. c) Support and agree the objectives set out in the draft Year 2 Work Plan (20152016). Appendix A MATERNITY SERVICES COMMISSIONING STRATEGY WORK PROGRAMME: YEAR 1 (DEC 2013 – MARCH 2015): Final Version March 2015 Outcome reference key * 1. Improving maternal health; 2. Reducing maternal morbidity; 3. Reducing infant mortality; 4. Reducing infant morbidity; 5. Improving women and families’ experience of care Key Actions 1 2 Development and implementation of service specification for maternity services Implementation and monitoring of maternity tariff Outcome ref Lead Status/Outcome Timescale for completion Evidence of progress/update 1,2,3,4,5 Hull CCG Service specification approved by CCG Ratification by Hull and East Yorkshire NHS Hospitals (HEYHT) Contract monitoring February 2014 Complete March 2014 Agreed and in contract Meeting with HEYHT January 2014 to discuss actions required to provide monitoring information for 2014/15. April 2014 1,2,3,4,5 HEYHT and Hull CCG Tariff requirements incorporated into service specification for maternity services. April 2014 Complete Agreed and in contract 3 4 5 Development of maternity performance framework, incorporating CCG Indicators and NHS Outcomes Framework Indicators 1,2,3,4,5 Development of assurance and reporting framework for work programme 1,2,3,4,5 Maternity Protected Time for Learning (PTL) event for Primary Care 1,2,3,4,5 Hull CCG Developed and incorporated into service specification for maternity services March 2014 Complete Agreed and in contract Contract monitoring Hull CCG Hull CCG Working Group to meet bi-monthly Reporting (quarterly/six-monthly) to: Hull Children and Families Board Hull CCG Children, Young People and Maternity Programme Board Health and Wellbeing Board Health Overview and Scrutiny Commission January 2014 Agreement for Maternity PTL 18.3.2015 Completed Working group established and continues to meet Completed A PTL has been agreed and is planned for the 18th March 2015. An agenda has been agreed. Objectives 1 2 Improve pre-conceptual care particularly women with: Existing health conditions Previous history of obstetric/genetic problems Second and subsequent pregnancies Increase the number of normal births 2013/14 to 2014/15 Outcome ref 1,2,3,4 1,2,3,4,5 Lead Action(s) required Public Health (Rachel Iveson) i HEYHT (Janet Cairns) i Needs assessment and scoping exercise Timescale for completion July 2014 Recommendations discussed and agreed with partners September 2014 Establish current status/baseline information and set targets April 2014 Evidence of progress/update Ongoing An outline for a Maternity JSNA has been agreed, Due to capacity and prioritisation completion of a Maternity JSNA is to be carried over into the Year 2 work plan. Ongoing Further work is needed to agree and confirm baseline and targets. For the period 2013/14 the normal birth rate was reported by HEYHT to be 66.9% which is above the national average of 62.9% national average. ii Ongoing agree target (numbers and %) for year-on-year improvement Further work is needed to agree and confirm baseline and targets. This action is to be carried over into Year 2 of the work plan. iii iv Include Quality Requirement within service specification for maternity services Establish Alongside MidwifeLed Unit at Hull Royal Infirmary site March 2014 Completed TBC Agreed and in contract Ongoing HEYHT are still committed to establishing a MLU at the Hull Royal Infirmary site and a number of meetings have taken place to progress this work. Objectives 3 Improve breastfeeding rates at initiation and at 6 to 8 weeks, 2013/14 to 2014/15 Outcome reference 1,2,3,4 Lead Action(s) required Public Health (Rachel Iveson) i Establish current status/baseline Timescale for completion April 2014 Evidence of progress/update Completed ii Include Quality Requirement within service specification for maternity services March 2014 As of May 2014 a baseline established at: 60.1% initiation 31.7% at 6-8 weeks Completed iii Focus on improving breastfeeding rates through Life Course Approach to be incorporated into Health and Wellbeing Strategy June 2014 Completed iv UNICEF BFI Level 3 accreditation for community services March 2014 Completed in November 2013. v UNICEF BFI accreditation Level 3 for hospital services March 2015 vi Review progress against targets Ongoing through 2014/15 vii Service now monitoring and maintaining accreditation Continue with ibreastfeed campaign On going Re-tender of breastfeeding peer support services to ensure maximum value for money May 2014 Increase availability of breast pumps for loan within the community May 2014 Ongoing HEYHY continue to work towards L3 accreditation Ongoing Doula service awarded further 4 years funding to support breastfeeding peer support programme Ongoing Completes - Tender exercise complete. Goodwin appointed as provider, delivering to target. Additional breastfeeding peer support clinics commissioned within year to increase access throughout the city. Completed – delivered to CHCP Objectives 4 Improving women and their families’ experience of care Outcome reference 1,2,3,4,5 Lead Action(s) required HEYHT (Janet Cairns) i Establish current status/baseline and agree areas for focused improvement Timescale for completion March 2014 Evidence of progress/update Ongoing Friends and family test monitored monthly Questionnaire to replicate the CQC maternity survey had a poor response and was reissued again to 100 women in December 2014 received only 38 responses. Further work is needed in this area in Year 2. ii HEYHT to implement Action Plan to address findings of CQC maternity survey 2013 January 2014 Completed An action plan is in place and is monitored on a monthly basis A survey/questionnaire was repeated in June 2014 however received a poor response and was sent out again to 100 women in December iii Friends and Family Test to be implemented Implemented Oct 2013 and ongoing monthly Completed Reported monthly: reviewed by the Hull MSF with suggestions and actions aimed at improved uptake iv Maternity Services Forum to develop service user engagement programme for 2014/15 Working group established January 2014 Ongoing Further work is needed in this area and Year 2 of the work plan includes a number of key actions to support this. Objectives Improve uptake of 5 newborn screening Outcome reference Lead Action(s) required Timescale for completion Evidence of progress/update 3,4 PHE/NHS E and HEYHT (Tara Cox and Wendy Francis. Jan Cairnes) i March 2014 Ongoing Identify and agree scope of screening programmes requiring action HEYHT continue to monitor progress against all new born screening programmes and report to Public Health England as required Identified areas for action include: ID 2 Antenatal infectious disease programme – timely referral of Hep B positive women for specialist advice ST 2 Antenatal Sickle cell and Thalassaemia screening – timeliness (although the trust has made in year improvements from 18% in Q4 to 49.1% in Q2 NB 2 Newborn Blood Spot test – avoidable repeats ii Establish current status/baseline and agree improvement target for each programme March 2014 iii Antenatal and Newborn Screening Steering Group to be established January 2014 iv Localisation of national service specifications TBC Completed Thresholds set by Public Health England and continue to be monitored and discussed at the Antenatal and Newborn Screening Programme Board Complete Further information required on this Objectives 6 7 Improve uptake of vaccination / immunisations (maternal and newborn) Reducing maternal obesity Outcome reference Lead Action(s) required Timescale for completion Evidence of progress/update 3,4 PHE/NHS E and HEYHT (Tara Cox and Wendy Francis) i Identify and agree scope of Vacc/imm programmes requiring action March 2014 Ongoing Action carried over into Year 2 work plan ii Public Health (Rachel Iveson & Claire Farrow) i Establish current status/baseline and agree improvement target for each programme Establish current status and baseline 1,2,3,4 Ongoing Action carried over into Year 2 work plan March 2014 Ongoing Further work is needed to establish a baseline Action carried over into Year 2 work plan ii Review pathway and service delivery May 2014 Ongoing Bitesize service launched, review still required to evaluate. Action carried over into Year 2 work plan iii Identify actions from preconceptual care needs assessment August 2014 Ongoing Dependent upon outcomes and recommendations of the Maternity JSNA iv Work with leisure services to develop maternity specific interventions September 2014 Ongoing Progress continues to be made Maternal healthy lifestyles action plan to be developed A bid has recently been submitted to Sport England, 'Get Healthy, Get Active' fund with the aim to increase the take up and maintenance of pregnant women/post pregnant women taking part in sport and physical activity. Us Mums to Be and Us Mums brand developed (in line with successful ‘Us Girls’ brand in the city). Ongoing Draft lifestyle plan has been prepared and requires further consultation. This action to be carried over into Year 2 of the work plan Objectives 8 Improve Perinatal Mental Health (PNMH) Outcome reference 1,2,3,4,5 Lead Action(s) required NHS Hull CCG i Primary Care workforce development Timescale for completion TBC PNMH Team ii Ongoing Training has been delivered to all Health Visitors to support early identification. This work is supported by the Institute of Health Visiting. Public Health workforce development CHCP TBC iii PNMH Care Pathway December TBC iv Map of Medicine March 2015 University of Hull v Re-establish Maternal Mental Health Advisory Group Deliver a Perinatal MH conference in Hull TBC TBC Ongoing NHS Hull CCG approved a perinatal mental health research project and training to primary care re: PNMH from September 2014. The study continues The Maternity PTL on the 18th March has a dedicated session to Perinatal Mental Health and the research study. This action is to be carried over into Year 2 of the work plan. University of Hull Hull CC PH Evidence of progress/update TBC This action is to be carried over into Year 2 of the work plan. Ongoing The ‘Let’s Talk’, Depression and Anxiety Service Hull went live on October the 1st 2014; they are now the lead providers for Primary Care Mental Health in Hull. Further work is needed in this area and will be taken forward in Year 2 of the work plan Ongoing This action is to be carried over into Year 2 of the work plan. Completed Next meeting agreed to take place in April 2015 Ongoing Agreement by University of Hull to develop and deliver a city wide Perinatal Mental Health conference/workshop in 2015 This action will be carried over into the year 2 work plan Objectives 9 Reduce smoking in pregnancy Outcome reference 1,2,3,4 Lead Action(s) required Public Health (Rachel Iveson) i Establish baseline Timescale for completion April 2014 Evidence of progress/update Completed Baseline set as of 2013 data: Number of mothers smoking at time of delivery = 23.1%. Aim to reduce year-on-year. Q1 2014-15 data shows that the rate has reduced to 20% for the first time. Attributed to the success of the new pathway implemented by CHCP and midwifery. Further work is being undertaken to ensure that this reduction is not impacted by the withdrawal of free Nicotine Replacement Therapy ii Review of evidence April 2014 Completed iii Implement CO monitoring July 2014 Completed Midwifery training commenced in May 2014 and was completed by October 2014. Monitoring is now in place Appendix B MATERNITY SERVICES COMMISSIONING STRATEGY WORK PROGRAMME: YEAR 2 (APRIL 2015 – MARCH 2016): Version 1.1 May 2015 Key Actions – Governance and Accountability 1 2 Lead To monitor the overarching contract performance of commissioned maternity services, including implementation of NICE guidelines, LSA Audit and response to Dr Kirkup’s report on Morecambe Bay NHS Hull CCG To maintain and further develop the Hull Maternity Services Forum NHS Hull CCG Status/Outcome Timescale for completion Evidence of progress/update May 2015 Ongoing Receipt of quarterly performance reports. Performance managed where required by contract board meetings. Awaiting final report from LSA before can share and release as public HEYHT reported at May meeting the Trust response to Dr Kirkup’s report Ongoing Regular meetings with quorum attendance Increased scope of membership including a service user Service user attended May MSF meeting 3 To develop and implement a Maternity Joint Strategic Needs Assessment for Hull Hull CC (Rachel Iveson) TBC Meeting planned with NR and Vicky Harris to in June 2015 discuss Maternity JNA 1. Research and development Objectives Lead Action(s) required Timescale for completion Evidence of progress/update December 2015 Meeting with Jan Cairns and development of proposal by end of April 2015, Proposal to CCG for approval by end of May 2015 HEY audit approval by June 2015: 6 month audit, presentation of audit report by Dec 2015 Hull University HEYHT To ensure that any new maternity service development is evidence based and evaluated to measure outcomes and added value. Jan Cairns 1.1 To develop and deliver a proposal for a still birth audit in partnership with Hull University Julie Jomeen Meetings taken place, proposal in preparation Jan Cairns 1.2 Julie Jomeen Natalie Robinson Jan Cairns 1.3 To develop a pilot pregnancy telehealth project for a period of 12 months with agreed evaluation and outcome measures May 2016 Proposal to CCG by April 2015, ethics approval May 2015, commencement of project June 2015, monthly review meetings against project milestones To develop a pilot GP led 24 week antenatal assessment in primary care September 2015 Initial discussions taken place with HEYHT to understand scope of assessment. Building on feedback from PTL Maternity event. NR to prepare a proposal to go to CCG SLT for approval, - June 2015 2. Service Development Objectives Lead Action(s) required HEYHT Timescale for completion Evidence of progress/update May 2015 & ABL Healthcare To reduce the number and rate of still births. (links to work streams 1, 5) Baseline 3 year period 2010-2012 Number of Stillbirths = 49 Rate per 1,000 total births = 4.7 2.1 Jan Cairns Jan Cairns 2.2 Jan Cairns 2.3 HEY to carry out SANDS audit tool and develop an action plan to address findings Sept 2015 Linked to Still Birth Care Bundle work Establish and agree baseline and agree improvement stretch target June 2015 2014 27 Still births Participate in NHS England Still Birth Care Bundle programme April 2015 Work on-going, including baseline audit of C0 monitoring in practice, improvements identified Cardiotocography (CTG) interpretation – signed up to K2 online programme to assess CTG interpretation. Customised Growth Chart – capacity identified as issue, involved in SABINE project, looking at GAP programme Looking at competencies, what happens in Antenatal Day Unit Jan Cairns 2.4 Workforce development in primary care re: education and understanding of foetal movement monitoring TBC Aligned to still birth care bundle, information leaflet being prepared, will be shared with primary care and relevant colleagues. Leaflet primarily for patient use To increase the number of normal births ( see link to telehealth in work stream 1) Jan Cairns 2.5 Establish baseline based on three year period 2011 2014 June 2015 April 2015 61.6% Normal Birth 27.2% Caesarean Section 10.3% Instrumental Birth 2.6 2.7 2.8 Natalie Robinson Agree target and plan for improvement June 2015 Targets Normal Birth ≥60% Caesarean Section ≤26.3% Instrumental Birth ≤12.8% Establish reporting framework for assurance to MSF Develop policy for elective Caesarian, aligned to IFR panel. Sept 2015 On-going Jan Cairns agreed to share trust report after each MSF meeting. Initial discussions taking place locally with CSU and HEYHT, scoping current situation, capacity and considerations for any local policy. April 2015 Draft policy prepared for consultation with HEYHT,LMC, GP Board Members, Public Health, Patient Ambassadors, Commissioners and MSF Ratification of IFR policy to go to Planning and Commissioning Committee and LMC in July 2015 2.9 To increase the number of home births Jan Cairns 2.10 2.11 Establish alongside midwife led unit at Hull Royal Infirmary site TBC Establish baseline based on three year period 2011 2014 June 2015 Agree target and plan for improvement June 2015 A costed proposal has been prepared, for consideration by HEYHT. Jan Cairns to provide feedback and update at next MSF Improve access and outcomes from birth preparation and parent education services Jan Cairns 2.12 Victoria Sharpley Victoria Sharpley 2.13 Develop a revised virtual tour DVD of Maternity Unit that is used by all required services Sept 2015 To agree stretch target to increase the number of primps attending the BUMPs service and action plan as a result. June 2015 CCG commissioners and contracting have worked with ABL to agree staged a plan to improve activity aligned to a wider service development plan. Agreed and in contract from May 2015 Currently providing places to all women who request a place and have an average of 11 participants per group. Plans are in place to raise the BUMPS profile. ABL have in place a PR and Coms and Marketing strategy and plan. Includes; o promotional stands in clinics/HEY/ childrens centres o shopping centres o health centres o health promotion events (i.e. PTL events) o Monthly press releases, radio interviews (where possible) o Social media (paid advertising) Targeting wards with the lowest uptake- Orchard Park, Newington, Myton MSF Members 2.14 To review BUMPS booklet and agree content for revised version prior to print May 2015 Booklet raised at MSF meeting: Feb Laura Allenby sent out with MFS minutes: 16th Feb and 6th March by Natalie comments requested back by Monday 27th April. No comments received. Going to print June 5th. 3. Service User Experience and Engagement Objectives Lead Action(s) required HEYHT Timescale for completion Evidence of progress/update May 2015 ABL Healthcare To demonstrate continual improvement in the experience of care along the maternity pathway for women and their families Jan Cairns 3.1 Victoria Sharpley To establish current status/baseline and agree areas for focussed improvement. To include client questionnaires, external audit, LSA report, Peer review, CCQ, PALS and complaints Sept 2015 HEYHT to provide details of PALS, complaints and service user feedback at future MSF meetings. At May meeting it was agreed that lessons learnt and themes will be shared with the MSF Carolyn Rabaud (CHCP, HV) agreed to review and consider a reporting framework for service user feedback to include parents of children up to the age of 1 year. ABL currently; Collect anonymous feedback after each course Do a 6 monthly survey with additional follow up questions i.e. “following your birth and the first few post-natal weeks, was there anything you would have found useful to have been included in the classes” Provide a ‘you said, we did’ every quarter Collate feedback each month and implement into the classes, i.e. more interactive work. Work under CQC/ ISO registered Jan Cairns Victoria Sharpley 3.2 To develop a mechanism for sharing service improvements and changes that occur as a result of service user feedback Sept 2015 MSF members MSF members 3.3 3.4 Improve uptake and completion of the Friends and Family Test, giving consideration to a city wide media and communication plan. Ongoing Maternity Services Forum to develop a service user engagement programme for 2014/15 Sept 2015 NR to establish a task and finish group to look at service user engagement and experience. Meeting to take place in June 2015 4. Health Protection Objectives Lead Action(s) required Timescale for completion Evidence of progress/update May 2015 PHE/NHS E and HEYHT To improve on coverage and timeliness of results and required assessments associated with the antenatal newborn screening programme: ID1 Antenatal infectious disease programme – HIV coverage ID 2 Antenatal infectious disease programme – timely referral of Hep B positive women for specialist advice FA1 – Down’s syndrome screening completion of laboratory forms ST1 Antenatal Sickle cell and Thalassemia screening coverage ST 2 Antenatal Sickle cell and Thalassemia screening – timeliness ST 3 Antenatal Sickle cell and Thalassemia screening – completion of FAQ NB 2 Newborn Blood Spot test – avoidable repeats NP 1 Newborn and Infant Physical examination – results entered onto database within 72 hours NP 2 – Babies with hip referral have ultrasound appointment within 2 weeks Tara Cox 4.1 Wendy Francis Continue to monitor, identify and agree scope of newborn screening programmes requiring action Ongoing CCG representation on ANNB Programme Board. Data provided by HEYHT to MSF Q4 2014/15 ID1 – 90.7% ID2 – 50% FA1 – 98.5% ST1 – DNA ST2 – DNA ST3 – DNA NB2 – 4.9% NP1 – 96.6 NP2 – DNA Jane McFarlane DNA – Data not available nationally 4.2 HEYHT to ensure that there is a fully established and ongoing internal HEY ANNB group to oversee delivery and KPIs Ongoing Meeting planned for 2nd June. Miss J Hingorani to chair meetings. Terms of reference to be developed, meetings will be held quarterly. Membership includes: Screening Coordinator Clinical leads for screening programmes eg. Consultant Microbiologist, Cons. Neonatologist, Radiologist, Lead Sonographer, Fetal Medicine Lead,. Head of Midwifery PHE representation NHSP Coordinator CHRD representation Midwifery representation (ie Community MW sister) 4.3 4.4 4.5 4.6 Provider to ensure that they can identify the cohort for each programme TBC ID2: Improve on the timely referral of hepatitis B positive women for specialist assessment to ensure that the 70% acceptable threshold is met. Ongoing Performance for Q4 2014/15 50% Remains an issue, have only managed to achieve once due to hard work of infectious disease consultant. Kevin Phillips is working with the clinical support division to address this. ST2: Improve on the timeliness of antenatal sickle cell and thalassaemia screening to ensure that women are tested by 10 weeks gestation within the acceptable threshold of 50% Ongoing Q4 2014/15 Data not available (nationally) NB2: Improve on the number of avoidable repeat tests for new born blood spot screening to ensure that the acceptable threshold of 2% is not exceeded. Ongoing Performance for Q4 2015/15 4.9% Considerable work going on to address. E-Learning has been mandated, midwives who have never had a repeat are carrying out peer assessments and sharing good practice. From April 1st 2015 laboratory have changed requirements in terms of amount of blood for sample. There is an expectation that this KPI will go down as a result until new practice embedded. To improve uptake of vaccination / immunisations (maternal and newborn) Maternity Flu Pertussis Hep B Tara Cox 4.7 Wendy Francis 4.8 Establish current status/baseline and agree improvement target for each programme Review delivery mechanism of maternity flu as part of the Yorkshire and Humber Sub-region Flu Strategy 31st May 2015 NR requested data from PHE – May 2015 TBC NR requested updated from PHE – May 2015 5. Healthy Lifestyles Objectives Lead Action(s) required Timescale for completion Evidence of progress/update May 2015 Hull CC Public Health To reduce smoking in pregnancy (links to work stream3) Alex Norman Baseline Smoking status at time of delivery for 2013/14 was 21.6% (PHE 2015). (PHE 2014 Local Tobacco Control Profile). 5.1 2015-18 New Smoking Cessation Service specifies: Reduce smoking in pregnancy; local target - to reduce rates of smoking throughout pregnancy by 1.0 percentage point per year to 17.6% by 2018 Current position to be reported when data available 5.2 5.3 5.4 To improve breastfeeding rates at initiation and at 6 to 8 weeks, 2014/15 to 2015/16 Establish current status and agree improvement stretch target Rachel Iveson 5.5 All midwives already have “Smokefree Training” To explore the implementation of risk perception training Not Applicable Implement a localised Baby Clear project aligned to Stillbirth Care Bundle Ongoing HEY are not proceeding with the Baby Clear Project because of the cost. HEY is a pilot site in Yorkshire and Humber for a project to reduce still births and near natal deaths; there are four elements to this of which one is CO Monitoring. All midwives have CO Monitors. Ensure NRT support is available to all pregnant women who wish to stop smoking Ongoing NRT support to pregnant women is included in the new Smoking Cessation Service Specification in which pregnant women feature as a “priority group”. NRT can also be supplied via the GPs, midwives and consultants are aware of the value of NRT and can prescribe as required. Establish current status and agree improvement stretch target COMPLETED Ongoing Breast Feeding Initiation April 2015 69% 6-8 week breast feeding rate currently at 32%, have been national issues on the data set and acceptance of data quality, being addressed locally. Baseline established at: 60.1% initiation 31.7% at 6-8 weeks 5.6 5.7 5.8 5.9 To reduce maternal obesity Rachel Iveson & Claire Farrow 5.10 Focus on improving breastfeeding rates through Life Course Approach to be incorporated into Health and Wellbeing Strategy TBC UNICEF BFI accreditation Level 3 for hospital services November 2015 HEYHT have confirmed that the BFI assessment is due to take place in October 2015 Maintain UNICEF BFI Level 3 accreditation for community services November 2015 Local work on going to support successful accreditation, including liaison with BUMPS re: course content. Continue with ibreastfeed campaign TBC Establish current status/baseline and agree improvement stretch target July 2015 Regular meetings established with HEY Maternity Services SLA in progress re continuation of Healthy Lifestyle Midwife post which will agree clear targets based on previous performance and anticipated throughput; monitoring arrangements and qualitative and quantative information to be collected to inform performance. Q3 2014/15 24.9% of women at booking had BMI ≥30 5.11 5.12 5.13 Establish stretch targets for agreement with all partners TBC Review pilot service In progress and will be completed to inform new SLA by July 2015 Carry out a mapping exercise of current service provision of physical activity interventions, Completed Additional funding has been secured through Sport England to deliver a 3 year physical activity in pregnancy programme in partnership with HEY. A comprehensive programme of PA opportunities will be classes and sessions available to pregnant women developed as part of this programme linked to identified needs/demands, supported by key workers linked to HL Midwife and Community Midwifery Service. COMPLETED 5.14 5.15 To improve preconceptual care particularly women with: Existing health conditions Previous history of obstetric/genetic problems Second and subsequent pregnancies Rachel Iveson 5.16 5.17 Maternal healthy lifestyles action plan to be developed TBC In progress and linked to the above programme development Deliver a coordinated and suitable physical activity and healthy cooking programme for pregnant women “Us mums to Be” Year one programme to be drafted by end of July 2015 this will be part of the new programme and is currently in development CF and FR attending introductory workshop with Sport England in May 2015, programme likely to commence in Summer 2015. Needs assessment and scoping exercise 1st Draft September 2015 Needs assessment on pre-conceptual in progress, but waiting for further data from the acute trust. Needs confirmation on what data will be provided by June2015. Recommendations discussed and agreed with partners October 2015 6. Mental Health Improvement Objectives Lead Action(s) required Timescale for completion Evidence of progress/update May 2015 University of Hull To improve Perinatal Mental Health (PNMH) (links to work stream 1) University of Hull 6.1 To reinstate the Hull and East Riding Maternal Mental Health Advisory Group (MMHAG) March 2015 First meeting held 20th April 2015. Minutes of meeting completed – arrangements in place for next meeting COMPLETED MMHAG MMHAG MMHAG University of Hull 6.2 6.3 6.4 6.5 To review and refresh the clinical pathway for PNMH March 2016 All relevant parties (Let’s talk, HV, PMH team, IAPT) engaged in process of reviewing and refreshing pathway – arrangements pathways meeting underway, deadline for completion of pathway exercise 1st June 2015 To evidence base impact and outcomes of service interventions; including establishing a performance framework, data collation and analysis. March 2016 Ongoing To develop a Map of Medicine for PNMH to provide primary care practitioners with access to advice and prescribing information for women with PMI Sept 2015 This is ongoing and largely dependent on the progress of the GP/Primary Care Practitioners research study below To report on findings of the PNMH training in Primary Care study and make recommendations for any further action required. June 2015 The findings to date have been presented @ PTL event Continuation of project reliant on agreeing on a suitable method for delivering training – discussions still on going with Hull CCG. Possibility of another training event – if a clear strategy for advertising is agreed on between research team and Hull CCG University of Hull University of Hull 6.6 6.7 To develop and deliver a workforce development plan that includes scoping of an e-learning package. Ongoing Develop and deliver an accredited Perinatal MH workshop in Hull January 2016 Linked to the work of the PNMH training project and a package may emerge out of this project as an alternative form of delivery. At minimum will produce a report of workforce training need and recommendations for training by March 2016 with proposal for training provision and outline package. Work will link to content of PMH workshop Workshop planning team minutes Confirmation of programme August 2015 and advertising of workshop Conference/workshop planning underway – initial discussions taken place in March 2015 regarding suitable date, venue, and possible speakers.