Case 1 (SIDS) 2 month old boy coming in by EMS found
advertisement
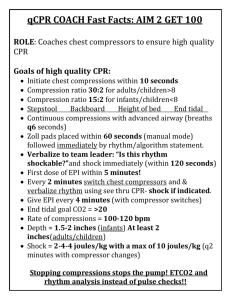
Case 1 (SIDS) 2 month old boy coming in by EMS found unresponsive in his crib. Asystolic on EMS arrival and they are doing full CPR. ETA 2 minutes. What are you going to get ready? People, equipment, drugs Tube size? Blade size? 3.0 -3.5 cuffed; 3.5-4.0 uncuffed 0-1 Miller blade Patient arrives in resusc bay. The nurses take over CPR. What do you instruct them to do? (Be specific) 15:2 compression ratio; compress chest 1/3-1/2 of diameter of chest EMS has tried IO in both tibias and unsuccessful. Where are you going to go next? Review landmarks for IO Best next spot is distal femur but can also use prox humerus if needed While you are trying to get access the charge nurse asks if you want epi down the ETT. What do you say? Review evidence for this – no evidence in adults but perhaps some in peds/neonates so for now is still a reasonable option but should not waste time on this instead of getting IV/IO access If use then use 10x dose and flush with 5mL NS and PPV x 5 The patient has had 1 x dose down the ETT and you now have IO access. Your staff tells you to use high dose epi through the IO – you vaguely remember that this is not part of PALS but aren’t sure why not…what do you say? The family runs in shortly after EMS arrives. What do you do with them? Review benefit of family presence during CPR When do you call it? Name 3 instances when you would continue longer. Hypothermia Toxin-induced cardiac arrest Recurrent/refractory VF/VT Known cardiac disease, witnessed arrest and ECMO available Case 2 – Bradycardia 2 year old rushed in by parents this morning. Unwell for 3-4 days with fever and cough and some wheezing/resp distress but parents hadn’t been too concerned until about an hour ago and things have gotten much worse in the car on the way to ACH. On arrival he is blue and unresponsive and they call you STAT overhead. Initial vital signs: T 38.2, hr 30, rr 10. They cannot detect a blood pressure. O2 is 76% on non-rebreather mask. Glucose check shows 10.1. What do you do? Start bag-mask ventilation – at what rate? (12-20; closer to 20 as younger) BVM being done at rate of 20bpm. No improvement in hr – remains at 40. Rhythm appears as sinus bradycardia. Still unable to get a BP. Pulses are weak, extremities cool, skin mottled in appearance. Crackles throughout. What is your immediate intervention? Trial of atropine or epinephrine Begin compressions (15:2) – difference from adult world where we do compressions for hr <60 and unstable Secure an airway (do this early as respiratory causes are most common) Size tube? Meds? Doses? Successfully intubated this patient – now what rate do you bag at? Saturations are now 94% on 100% FiO2 but hr remains 40 and perfusion has not improved. What next? Continue compressions at 100/min; breaths at 8-10/min Epinephrine - dose? After one round at your next pulse check hr is 80 and perfusion slightly better. BP now 55/30. Can give some fluid – probably no more than 40mL/kg – if still poor perfusion would start epi infusion and talk to PICU Now draw labs; do CXR; order abix; etc. (post-resusc care) The ICU resident comes in – it is her first day on call and she wants to know if you think she should cool this patient? Review evidence for cooling post-resuscitation. Case 3 (myocarditis): 7 year old girl presents to PLC with 1 week of fever and flu-like symptoms. She looks unwell so the triage nurse takes her straight to the resuscitation bay and pages you overhead. When you arrive you see this on the monitor: (strip of VTach) She is sitting up on the stretcher and able to speak to you but is very pale. Vital signs are: T-38.2C, hr 160, rr 28, BP unable to obtain, Sats 91% on RA. Pulses are weak and thready, CRT 6 seconds, rumbling systolic murmur at the apex, fine crackles to both lung bases, liver is 4cm BCM. What are you going to do? O2 IV Labs (CBCD, BC, extended lytes, creat, troponin, gas) Put defibrillator pads on her ASAP! Call cardiology/PICU What size of defibrillator pads are you going to use? What position? <10kg (1yo) use pediatric pads >10kg use adult pads The nurses can’t get an IV or bloodwork. What do you do? Can check out saphenous vein or insert an IO Art gas/cap gas IO can use local to help with pain; can infuse lidocaine o.5mL/kg into IO prior to meds to help with injection pain List 5 complications from IO placement Your gas comes back – Ph 7.13/CO2 30/HCO3 15/lactate 13/gluc 11; lytes N What do you want the nurse to draw up? Have epi drawn up - ? doses? Have your own epi pocket infusion drawn up – dilute 1mL in 9mL NS to make 10mcg/mL You now have IO access and nurse asks you if you want fluids running. If use then use small amounts – 5-10mL/kg and stop if worsening What next? Cardiovert (chemically or electrically) If choose electrical – what energy dose? Are you going to sedate first? If choose chemical – what dose and what rate? Would not do this in an unstable patient as could significantly worsen the hemodynamic profile with amiodarone After you cardiovert she suddenly becomes apneic and limp. The monitor shows Vfib now. What do you do? BLS – start compressions and bagging (15:2) Intubate – what size tube? Size blade? Defibrillate – energy dose? Epi doses? Amiodarone? After 3rd shock she is in wide complex PEA rhythm. What now? Epi – doses? The PICU transport team shows up and asks: Have you given any Calcium yet? name 3 instances when you would use What about bicarbonate? Name 2 instances when you would use Case 4 – Neonatal resuscitation You have a 32 year old female arriving at Foothills via EMS from a well known drug house with severe abdominal pain. She is high but states she has been worried she is pregnant but hasn’t seen a doctor yet and isn’t sure how far along she might be. You take a look and see that she is crowning. Meconium present. You deliver the baby immediately – she is limp, blue and not making any respiratory effort. What do you do? If any question about viability then attempt resuscitation. Viability - >23-24wk GA; >400g Warmer if possible – otherwise increase the heat in the room. (heat loss is very rapid in newborns; especially in prems – ideally would have a polyurethane bag to wrap in to decrease insensible losses in <29wks but in ED wouldn’t have this) Follow NRP guidelines Dry and stimulate – ideally you would suction meconium but in the event that you don’t have equipment readily available don’t waste time on this Check hr (feel pulse at umbilical artery or listen over apex) - 50 Still no resp effort begin BVM Do you want to use naloxone? (no! in this baby could withdraw; also caution in any baby as you can miss important causes of resp depression if blame things on narcotics) Tips for BVM – suction; reposition head; open mouth slightly; bag with 15-20cm H2O pressure; most important indicator of good BVM is improvement in hr Begin at RA and increase to 100% if no improvement in 90 seconds or beginning chest compressions BVM is single most important intervention as <0.1% go on to require chest compressions Recheck hr – if <60 then begin compressions (3:1 ratio) Recheck hr – if remains <60 then give epi – how are you going to obtain access? Will you use the ETT? Secure airway – tube size? Tube depth? Blade size? Meds? Continue 3:1 ratio even after airway is secured Give fluids – 10mL/kg aliquots as neonatal heart and brain really sensitive to volume changes; if suspicious of bleed then use O neg rbc’s Look for other causes (i.e. pneumothorax) How long do you persist?