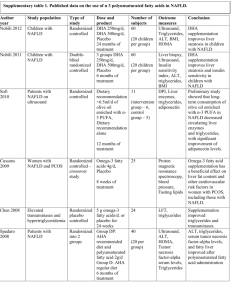
Supplementary Data
advertisement

Supplementary Box 1: NAFLD Fibrosis Score (NFS) calculation and accuracy NFS can be calculated on a free, easy to use on-line calculator (http://NAFLDscore.com). NFS = -1.675 + 0.037 X age (years) + 0.094 X BMI (kg/m2) + 1.13 X Impaired fasting glucose/diabetes (yes = 1, no = 0) + 0.99 X AST/ALT ratio + 0.013 X platelet count (x109/L) - 0.66 X albumin (g/dl). The low cut-off score (<-1.455) has a negative predictive value (NPV) of 88–93% and the high cut-off score (>+0.676) has a positive predictive value (PPV) of 79– 90% for the presence of advanced fibrosis in NAFLD in secondary care populations (13, 22). Those with an indeterminate score (-1.455 to +0.676) cannot confidently have advanced fibrosis excluded and require further investigations (i.e. transient elastography). Supplementary Box 2: General information on the MDT NAFLD clinic The MDT NAFLD clinic was started in 2009 at the University Hospitals Birmingham, UK. The MDT clinic consists of: o 2 consultant hepatologists (P.N.N; G.H) o 1 consultant endocrinologist (J.W.T, with specialist interest in obesity/NAFLD) o 2 Diabetes specialist nurses (A.P, L.C) o 1 specialist dietician with an interest in liver disease (J.J) o Rotating clinic research fellows (M.J.A, R.P) Between 1st January 2010 and 30th December 2010, there were 95 new referrals to the clinic and 400 patients were reviewed. In 2012, the clinic had 150 new referrals and 670 patients were reviewed. The specialist liver tools available include; transient elastography (Fibroscan®) and Fibrotest (Biopredictive, France). In 2012, the transient elastography service became nurse-led (M.R). 1 Supplementary Box 3: Dietary assessment and guidance Assessment: Weight history, current weight/BMI, and influencing factors Lifestyle and exercise via direct questioning (open and closed questions) Food intake and eating habits via a 7-day food diary (completed prior to appointment) Rationale: Discuss rationale for diet and lifestyle advice in relation to the patients underlying liver disease and severity. Guidance: Tailored to patients lifestyle (i.e. variable working patterns, family members, ability to exercise etc) Aim to reduce energy intake by 250-500 calories per day to promote 1-2kg weight loss per month Rationale for breakfast and suitable choices Regular meals advised with rationale (introduced across appointments if very poor meal patterns i.e. only eat a high calorific evening meal etc) Target high sugar/fat intake (especially high sugar drinks i.e. energy drinks) Additional advice regarding fibre/vitamins/minerals across appointments Specialist advice for patients with type 2 diabetes: As above Additional rationale for complex (vegetables, cereal) vs. simple (e.g. milk, yoghurt etc) carbohydrates, glycaemic index and fibre. Discuss the effects of glucose vs. complex carbohydrates on blood glucose Discuss the fact that poor glycaemic control is a driver of fat accumulation in the liver and rationale for maintaining good control Establish clear aims and targets with the patient 2 Supplementary Table 1 – Demographics and characteristics of patients with type 2 diabetes screened with the NAFLD Fibrosis Score at the diabetes clinic in HHB, UK HHB diabetes clinic (n=64) Age (years) Male Sex, % (n) Ethnicity - White - Asian - Black - Other/unknown Metabolic conditions Obesity (BMI > 30), % (n) Hypertension, % (n) Hyperlipidaemia, % (n) Ischaemic heart disease, % (n) History of Liver disease, % (n) Metabolic parameters Duration of type 2 diabetes (years) HbA1c % [mmol/mol] Therapy for type 2 diabetes, % (n) - Non-insulin dependent - Insulin dependent Weight (Kg) Body Mass Index (Kg/m2) Systolic Blood Pressure (mmHg) Diastolic Blood Pressure (mmHg) Total cholesterol (mmol/L) Creatinine (µmol/L) Liver Function Tests ALT (IU/L) % (n) patients with abnormal ALT (>43) AST (IU/L) % (n) patients with abnormal AST (>41) GGT (IU/L) % (n) patients with abnormal GGT (>50) ALP (IU/L) % (n) patients with abnormal ALP (>130) Bilirubin (µmol/L) % (n) patients with abnormal Bilirubin (>17) Albumin (g/L) % (n) patients with abnormal Albumin (<35) 56.5 (48.3-67.0) 65.6 (42/64) 34.4 (22/64) 39.1 (25/64) 3.1 (2/64) 23.4 (15/64) 50.0 (32/64) 64.0 (41/64) 79.7 (51/64) 9.4 (6/64) 0.0 (0/64) 8.5 (5-10) 7.8 (6.8-9.6) [62; 52-81] 62.5 (40/64) 37.5 (24/64) 86.5 (73.5-98.5) 31.5 (27.8-35.1) 134 (121-139) 77.0 (69.8-82.5) 3.9 (3.6-4.8) 82.5 (72.0-95.5) 29.0 (22.0-46.8) 29.7 (19/64) 25.0 (21.0-33.8) 12.5 (8/64) 39.0 (27.0-58.0) 29.7 (19/64) 81.0 (69.0-92.8) 1.6 (1/64) 7.0 (5.0-9.0) 0.0 (0/64) 45 (43-46) 0.0 (0/64) All values are median values (IQR), unless stated. HHB, Heartlands Hospital Birmingham. Abnormal ranges for liver function tests are routine laboratory cut-offs (in brackets). 3