International Comparison of Preoperative Testing and Assessment
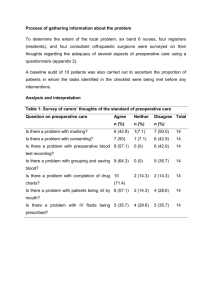
advertisement

International Comparison of Preoperative Testing and Assessment Protocols and Best Practices to Reduce Surgical Care Costs: A Systematic Literature Review Presenters: Kayla Cline, Texas A&M University Recorded on: February 11, 2015 Alright perfect, and now we're ready for today's presenter. Kayla. >> Hi everyone, I am Kayla Klein and I will be the primary presenter today >> Vita may join us later, she has a conflicting appointment, so you're stuck with me for now. So what I will be presenting to you today is the results of a paper that we have forthcoming in the journal of advanced student health care management. >> And so you can see the title of the paper here. You should be looking for it in the next couple of weeks or months. You can see we've worked on it with a few other people. We've worked on it with Stephen Timmons, who is one of our compatriots in the UK working in the business school in a healthrelated capacity there. We also worked with a fourth-year med student, Rahil Ripani. And then Tom Miller, who worked for the American Society of Anesthesiologists who is our CHOT industry partner for this project. All right. So Having some technical difficulties. Hold on. Okay. So overall what we're going to be talking about today is the usefulness of preoperative testing. And kind of what it looks like in the US and in other countries around the world. So we took a twopronged approach for this project. The first part of the project was a systematic literature review. What preoperative testing does for the surgical process and for surgical care quality. And then the second part was an investigation into national, nationally sanctioned preoperative testing guidelines in several Western countries. Our literature review findings in total sort of lead us to a few key conclusions, and you can see those on the screen here in blue. The first, we looked at clinical outcomes and we found that minimizing preoperative testing, and we'll kind of expand on what that means later. Minimizing preoperative testing did not have an adverse effect on clinical outcomes. We also looked at operating room efficiency and we found mixed results on routine and selective preoperative testing on operating room efficiency. And then we looked at cost savings and we found that if preoperative testing is done selectively, it can be a source of cost savings. But if it's done indiscriminately it can be a significant driver, potentially, of the cost of surgical care. So we'll expand on each of these points over the course of this next couple of minutes. So here's some background on what preoperative testing is, if it's not something you're familiar with. First of all, surgical costs in the United States are high and they're growing. So you see here on the slide in 2000, surgeries cost about $13,000 per hospitalization. In 2010, they have cost $18,000 per hospitalization. That is inflation-adjusted. So we've seen a pretty dramatic increase in the last couple of years in surgical costs. The reasons for this increase in the cost of surgery are many and multifaceted. So we're not necessarily saying that preoperative testing is necessarily the driver, but it has been pointed to as one driver of high surgical costs. And so, because of that, it's kind of come under scrutiny in recent years. Now when we say preoperative testing, we're talking about various diagnostic tests that are run on patients before they go into surgery. So this could include something as simple as a history and physical examination. It could also include EKG's, chest radiography, hemoglobin measurements, so on and so forth. Maybe some of you have experienced these tests or known people that have. It's pretty common. So, when we say preoperative testing we're just talking about tests that are prescribed for patients before they go into surgery. To prepare them for surgery or to identify issues that may become problematic during the surgery. And so the tests that are performed vary widely by procedure, and they also vary by doctor and by patient. They're very highly variable, which is another reason that they're studied so frequently. Health care organizations in many Western and developing nations have developed preoperative testing protocols as one approach to managing these costs. So these tests kind of add up and they get expensive and so some organizations have started targeting this as one place to standardize care. And there's a couple of different ways that organizations approach this. Some organizations have just developed really detailed standardized protocols. If this patient presents with this and has this comorbidity, we do this test. So, it's just a very detailed set of protocols, rather than allowing physicians to rely 100 percent on their discretion. Which may lead to over over-testing and may also lead to under-testing. So that's one approach. Another approach is the development of a preoperative clinic. And the preoperative clinics go by various names, but in general one of their main purposes is to coordinate preoperative testing to make sure. That maybe testing isn't done by multiple parties, that the right testing is done, and that the wrong testing isn't done. So, those are two approaches we're going to see commonly in the literature. And, all these approaches have come up because, as we mentioned earlier, critics have begun to question the usefulness of routine preoperative testing. And we'll see some studies that sort of back that up in just a A few minutes. So the section that we're about to go into is the actual lit review. We're going to look at the literature on the usefulness of preoperative testing across multiple lines of surgery. And that's kind of one the unique parts of this study, is that we're not looking at just one line of surgery. So, pancreatic surgery or ophthalmologic surgery or colo-rectal surgery. We're looking at all lines of surgery and we also, as an application piece, are going to look at testing guidelines in three western countries. As our sort of wrap-up. So to do the literature review, we employed three means of document retrieval. We searched several databases. You see there PubMed, JSTOR, and Google Scholar, using various terms related to preoperative testing, cost and efficiency to maximize our sensitivity. And then we also performed reference crawling of the selected articles that we found in the database search. And if you're not familiar with reference prowling, what we mean by that is we take an article that we found that was pertinent. And then we read the reference list and go pick out any of those references that are relevant and go get those papers and so on. And then we also, for the second part, the application piece, we searched national healthcare websites for relevant preoperative guidelines. So, for the literature review, we, this process yielded 154 potentially relevant studies, and we excluded 126 of them. Which seems like a lot. Some of it was based on publication dates, the studies were published before 1975 and so we didn't think they were particularly relevant at this point. Also, methodology. I would say this is where a lot of our culling came from. There were a lot of literature reviews and a lot of editorials. And since we were doing a literature review, we chose to exclude both of those types of studies. And then content. So if the paper mentioned preoperative testing but focused on another element of preoperative Care, we kind of culled that out. And so this left us with 29 studies, two surveys, two randomized control trials and 25 retrospective reviews of patient records. And so this map here shows where we found these papers. So most of them were published in the United States or Canada. But there were also others posted in, published, excuse me, in Thailand, Brazil, and Europe, as you can see there. Those are sort of the concentrations. But we got a pretty good worldwide canvas to work with. So when we summarized our results, we put the papers into one of three categories. Findings focused on clinical outcomes, findings focused on operating room efficiency, and then findings focused on cost savings. And often a paper fell into multiple of these categories. So in terms of clinical outcomes, we saw 12 studies that looked at the effect of preoperative testing on clinical outcomes. And so the findings were as follows. Four of these studies found patients who received routine preoperative testing, so that means indiscriminate, that's what I'll call it, indiscriminate preoperative testing. If you compare those to the people that received no preoperative testing, the clinical outcomes were very similar. Which may indicate that this indiscriminate testing was not particularly useful or not cost effective. Three studies found that if you implement selective testing, so rather the indiscriminate testing we were talking about before, but rather selective testing, either using the judgment of a high level provider like an anesthesiologist or very detailed protocols or something along those lines. So if you implement selective testing or use of guidelines, you don't have an incidence of adverse events. So in other words, this is saying if you trim down your testing and make you're only focusing on the important tests, and cut out the extra tests, you're not going to see an increase in adverse events. So that's a good thing. Going on, three studies show that implementing a preoperative clinic did not increased adverse events, and actually reduced length of stay. So again, you're kind of culling down the testing, making your testing more selective by using a preoperative clinic. You're not increasing adverse events, so that's good. And these studies actually showed that the preoperative clinic could reduce length of stay, which was also, generally speaking, considered to be a good thing. And then, finally, two studies found that abnormal preoperative test results were inferior predictors of adverse events, compared to patient and procedure-specific factors. So, basically, this is saying, if you look at, if you factor in patient co-morbidities and things like that, and then procedure-specific factors so the risk of a specific procedure, the explanatory power of test results kind of goes away. So compared to just the information about the procedure and the patient test results really aren't that important in predicting adverse events. And that's kind of the goal with preoperative testing. So this indicates that this indiscriminative preoperative testing is not particularly useful. So the key takeaway going forward here is that selective or minimized preoperative testing did not impair clinical outcomes. And there's some evidence that it could actually improve clinical outcomes, compared to indiscriminate testing. So those were kind of the key findings for clinical outcomes. Moving on to operating efficiency. This is our second category of results. We also saw that 12 studies looked at the effect of preoperative testing on operating room cancellations and delays. Now, the findings in this section were a lot more mixed. So as you see here, four studies found that if you have a preoperative testing clinic, or some kind of standardized process, aka selective preoperative testing, you can reduce cancellations. And different studies reported different numbers, different percentages, but something along those lines. Three studies, though, found that if it's just routine, standardized preoperative testing did not modify surgical approach or reduce cancellations. And then, the remaining five studies had just kind of disparate findings that were somewhere in between those two, and so the key takeaway here is that maybe we don't have a key takeaway quite yet. The literature was a little bit mixed on whether routine testing or selective testing could improve operating room efficiency, reduce cancellations, reduce delays. And also other literature in this arena has pointed to the fact that reducing delays and cancellations may or may not actually translate into cost savings, and that's a subject for a different paper. But it does kind of call into question whether preoperative testing and operating room efficiency really go hand in hand. Certainly the jury is still out. And that is kind of a natural segue into the costs section. So fewer studies focused on costs. I think the data is maybe just a little bit harder to find. Six studies looked at the effect of preoperative testing on costs. And there were kind of two approaches here. Some of the studies looked at how much indiscriminate testing costs. So if you do testing quote unquote poorly, or indiscriminately, how much does it cost your organization? And then other studies had implemented some sort of standardized testing protocol, or preoperative clinic, and so they were looking at the cost savings yielded by what we're calling selective testing. Then two studies looked at the cost of the indiscriminate testing and these studies found that such testing could cost up to 600 per patient, or $200,000 over one year in one relatively small organization in overseas, so that's not an insignificant chunk of change. And then four studies looked at the cost savings yielded by appropriate testing, so if you do testing but you do it well, how much can you save? And the findings there were that the savings were between 38.50 and 112 per patient, depending on the study. And one institution implemented a pre-operative clinic and saw that they saved 1 million over the course of the year in unnecessary testing. So that's definitely a significant amount. So a key takeaway here from the cost side of things is that if preoperative testing is done appropriately, if it's done well, it can yield cost savings, but if it isn't done well, it can increase institution costs dramatically. So definitely something that institutions want to be looking at because it is a source of potential overspending and as a potential source of savings. And no one really likes undergoing preoperative testing, and so not something that we necessarily saw in the literature, but from a patient perspective I would assume that less testing would probably be preferable. So that's an interesting arena for future research possibly, how it affects the patient's experience of care. So practically speaking, what does it mean? What do these findings mean for preoperative testing going forward? First of all, I would say that they highlight the importance of what I've been calling selective preoperative testing using specific guidelines or preoperative clinic, and not just having those in place, but actually Losing them of course. That's one of the hardest parts about this, is that you've gotta develop a set of guidelines, and you've gotta develop a site, a set of guidelines that physicians can use and find useful, or it's not gonna make a difference. And so, as this was sort of our key practical implication, we started looking at what's been done in this arena. So, we tried to identify country-specific guidelines that have been endorsed by various health care authorities in Western nations. And also, we were interested in looking at whether adherence to these guidelines was linked to payment for services. So, if you don't adhere to these guidelines, does it hurt you, essentially. So Table 2, this is Table 2 from our manuscript that's to be published in the next couple of weeks. This shows kind of the testing guidelines that we found in a few Western countries. So, the first two come from the United States. The first is put forward by the American Society of Anesthesiologists, and it's a set of guidelines for preanesthesia testing. But as you can see, adherence is not tied to payment. In the United States there's also the AHA/ACC Cardiac Preoperative Testing Guidelines by the American College of Cardiology and American Heart Association. And these are widely used and have been cited in the literature several times. But, again adherence is not tied for payment. So, this is a great resource for hospitals or practices that want to develop guidelines. But at this point, they're not instituted. No, for example, payers are holding providers accountable for these types of guidelines, financially. In the UK, you can see that there are three different guidelines. So the Association of Anesthetists of Great Britain and Ireland have developed pre-hospital anesthesia guidelines that include preoperative testing guidelines. The Royal College of Anesthetists also have developed a kind of guideline for preoperative assessment. And then the National Institute for Health and Clinical Excellence over there, across the pond, developed kind of a document specifying how to test, essentially. And this document, Preoperative Testing, Test: The Use of Routine Preoperative Tests for Elective Surgery, is in fact tied to payment. And this is the only guideline that we found that was. Canada, we found two. The Canadian Anesthesiologist Society has developed a set of guidelines. And also, in Ontario, a group of, I believe it's a group of physicians, have gotten together in this Ontario Pre-Operative Task Force to develop a testing grid. That's been analyzed in the literature for physicans to be able to kind of assess pretty quickly what tests need to be run for what type of patient for what type of procedure. And then in Europe in general, the European Society of Cardiology have developed some guidelines for non-cardiac surgery. They're very broad, but one subset of these guidelines focused on preoperative testing. So this is not to say that there are no other preoperative testing guidelines out there, these are the ones that we discovered. And it's also evident in the literature that many hospitals and healthcare organizations have their own individual preoperative guidelines that they do follow, that may be based on, in part, on some of these recommendations. This is one example of one of the United States guidelines that we saw. This is called Choosing Wisely, and so it's an endeavor of the American Board of Internal Medicine, where they kind of interact with various specialties to help inform providers and patients about what to look for in their healthcare. So this particular Choosing Wisely section was done in partnership with the American Society for Anesthesiologists, and the next two slides kind of highlight five things that the ASA, or this part of the ASA, would like patients and providers to think more carefully about. So you can see here, the first one, don't obtain baseline lab studies in patients who are ASA level I or II, relatively healthy, undergoing lowrisk surgery. So, and they specify some specific tests that are some specific expectations there. And they expand on that, and then don't obtain basic, baseline diagnostic cardiac testing or stress testing in stable patients with known cardiac disease, undergoing low-risk surgery. So again, sort of a general guideline. Here are 3 and 4. And I am not a clinician, so I don't pretend to fully understand all of these, and I imagine other clinicians would understand these better. But you can see here things related to blood utilization and hemoglobin measurement, catheters and cardiac surgery. And then here's the fifth Choosing Wisely element. Again, something that's a little out of my pay grade, but basically this is developed by the ASA for providers and patients to be able to make good decisions related to preoperative testing and preoperative evaluation. So, in sort of summary, the key takeaways are that selective or minimized preoperative testing did not impair clinical outcomes, may or may not have influenced OR efficiency in terms of delays and cancellations. That's something that we probably need a little bit more research on. But we did find that preoperative testing, if it's done selectively, can yield some cost savings, but if it's not done selectively it can increase institution costs dramatically. And then finally of, sort of the practical section of this studying, we found that national guidelines have been developed in several Western countries, but adherence to these guidelines is only linked to payment in the UK. Here are two publications related to this study. The first is the actual paper this study is based on. So again, it's forthcoming in Advances in Health Care Management, we expect it to be published in the next few months. So if you're interested in this, you wanna see more of the studies and more of the detail of this study, please go check that out, again, later this spring. And then the second is a related paper. This paper was developed as kind of part of a larger project on the perioperative surgical home and perioperative care. And so, the second paper, Kash et al, was published in the Milbank Quarterly last, I believe, December, and is more of a general overview of perioperative surgical care, and may be of interest to you, as this topic is interesting. So, with that, we will open it up for questions. Feel free to ask anything and I'll answer to the best of my ability. Hey Kayla. How are you? This is Dave from Penn State. Hi! I have a couple of questions. First of all, thank you for the presentation. Sure. And, did you find any kind of information about QALYs, which. QALYs, we know- In terms of the cost effectiveness. Yeah, so. Yeah, we actually didn't, we don't have anything on QALYs in this paper. This is, that's something we were really interested in, but unfortunately, it's not something we found a lot of studies on. So, no- Okay. We don't have anything about QALYs here. Yes, good. Yeah, I think for future research, it would be pretty interesting to see how we can use these cost effectiveness analysis from an economic health policy perspective. Right. To know how we can incorporate these QALYs, or how much the quality of life that we can gain by using these preoperative-like interventions, and to see from an economic perspective, if those type of interventions, preoperative screening, are cost effective. I think- Yeah. They are, but it would be good to have that. Kind of mortality versus mobility versus cause. Right, yeah. For future research, I think would be pretty interesting. I do too, yeah that's a great point. Thanks. Yes. Are there any more questions? Kayla's ready for them. I'm ready. Okay well, since we've, doesn't sound like anyone has any questions right now. Thank you everyone very much for attending today's webinar. Please feel free to send us an email. Send myself or Bita or Kayla any more questions you have, and please make sure to attend our next webinar which will be on March the fourth. Thank you all. Thank you.