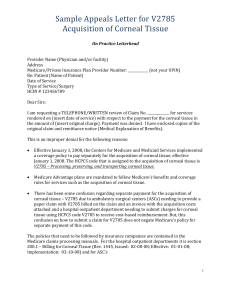
IC-88_El Danasoury_Handout
advertisement

IC-88 Modern trends in the diagnosis and treatment of Keratoconus Keratoconus Diagnosis & Management: Modern Technologies & Techniques Faculty: Alaa El Danasoury, MD Jorge Alio, MD Yaron Rabinowitz, MD Damien Gatinel, MD Farhad Hafezi, MD Joseph Colin, MD Course objective: The objective of this course is to provide delegates with basic information necessary for early detection of keratoconus, understanding the mechanism of action, indications& expected outcome of different available treatment modalities and selection of the most appropriate procedure for a given keratoconus case. Introduction: Keratoconus is the most frequent corneal dystrophy and a frequent contraindication of corneal refractive surgery. Reported estimates of its frequency vary widely between 50 and 230 per 100,000; recently incidence of keratoconus has increased due to availability of modern sensitive diagnostic tools able to provide early diagnosis. Keratoconus is a frequent cause of permanent visual loss and is the leading indication of corneal grafting in many parts of the world. Keratoconus has a multifactorial origin and appears to be under genetic control is some instances. Early diagnosis and measurement of keratoconus with modern technology: Detection of early keratoconus is sometimes difficult and has to be based on different sources of information. Anterior topography & biomicroscopy remains very important tools for the diagnosis of keratoconus. In the last decade, several technologies have been developed and used for the detection of early keratoconus, such as corneal aberrometry, measurement of posterior corneal elevation, and corneal biomechanics characterized by means of the corneal hysteresis. Corneal aberration measurement is, in our hands, the best method to grade and detect keratoconus. Anterior corneal aberrometry is the mathematical transformation of elevation data from corneal topography and offers a quantitative measurement of the optical performance of anterior ocular surface. Higher order corneal aberrations are significantly altered in keratoconus, with significant amounts of primary vertical coma. Any evidence of abnormal levels of primary coma over 0.5 and especially 0.75 microns in corneal aberrometry should be considered as suspicious. Validity of posterior elevation above the best fit sphere, as a diagnostic tool has been demonstrated; values of maximum posterior elevation in the 5 mm central zone over 30 microns are suspicious of keratoconus. Corneal Hysteresis and Corneal Resistance Factor in keratoconus and keratoconus suspect eyes This part focuses on the biomechanical properties of the normal eyes with eyes affected by various degrees of keratoconus. Proper recognition of form fruste keratoconus is a major concern for refractive surgeons and its diagnosis is not yet codified. Increased collagen distensibility has been reported to be an important factor in the pathogenesis of keratoconus and preliminary clinical studies have demonstrated reduced hysteresis in the presence of corneal pathology such as keratoconus and following laser in situ keratomileusis. We have explored the biomechanical properties of keratoconus and keratoconus suspect corneas, and to compare corneal hysteresis and corneal resistance factor in normal, keratoconus suspect, and keratoconic eyes. AVAILABLE TREATMENT MODALITIES: Corneal modelling using intracorneal ring segments In eyes with keratoconus, the placement of intracorneal ring segments generates both an immediate response that interrupts the biomechanical disease progression in keratoconus, and a time-dependent biomechanical response that allows subsequent improvement of vision over 6 months. The immediate response governed by the elastic properties and the long term response is by viscoelastic properties. Intracorneal ring placement results in a reduction of astigmatism and improved visual acuity. Different designs of ICRS including Intacs Segment, Ferrara Ring Segment & Keraring will be discussed Outcomes after Implantation of Intracorneal Ring Segments: Complications include epithelial defects at the keratotomy site, anterior and posterior perforations while creating the channel, extension of the incision toward the central visual axis or toward the limbus, shallow placement and/or uneven placement of the Intacs segments, infectious keratitis with the introduction of the epithelial cells into the channel during the channel dissection, asymmetric placement, persisting incisional gap, decentration, and stromal thinning, corneal stromal edema around the incision and channel from surgical manipulation. Corneal modelling by ultraviolet crosslinking In recent years, increased attention was paid to the biomechanical properties of the cornea. Corneal biomechanics are altered in a variety of corneal conditions such as keratoconus and pellucid marginal degeneration. Therefore, a therapeutic approach to increase the biomechanical resistance of the cornea would address important issues. Corneal collagen crosslinking with riboflavin and UVA (CXL) is a new clinical technique that fulfills these criteria. Interestingly, CXL leads to an arrest of keratoconus progression in some, and even to a regression of maximal K values in other patients. Clinical results of CXL for progressive keratoconus will be reviewed and potential explanations for the long-term topographical changes associated to it will be discussed in details. Deep Anterior Keratoplasty with Exposure of the Descemet’s Membrane Corneal grafting remains the only solution to restore visual acuity in many cases when rigid contact lenses, corneal ring segments and crosslinking are ineffective or contraindicated. Compared to penetrating keratoplasty, deep lamellar keratoplasty has many advantages: 1- preserving the patient’s endothelium, 2nullifying the risk of endothelial rejection 3- less rigid selection criteria for donor tissue. Surgical technique is more demanding as compared to penetrating keratoplasty. The combination of the big bubble technique with the Femtolaser lead to less postoperative astigmatism & earlier patient rehabilitation. Details of surgical techniques & long term clinical results will be discussed in details. Phakic IOL implantation in selected cases Phakic IOLs can also be used to correct myopia and compound myopic astigmatism in eyes with stable keratoconus, in eyes where the pathology has been successfully stabilized with crosslinking, intraconeal ring segments or both and also in eyes that received deep lamellar keratoplasty provided the selection criteria are met.