SURVEY OF OPHTHALMOLOGY VOLUME 42 • NUMBER 4 • JANUARY–FEBRUARY 1998
MAJOR REVIEW
Keratoconus
YARON S. RABINOWITZ, MD
Cornea-Genetic Eye Medical Clinic, Burns and Allen Research Institute, Cedars-Sinai Medical Center and
the Department of Ophthalmology, UCLA School of Medicine, Los Angeles, California, USA
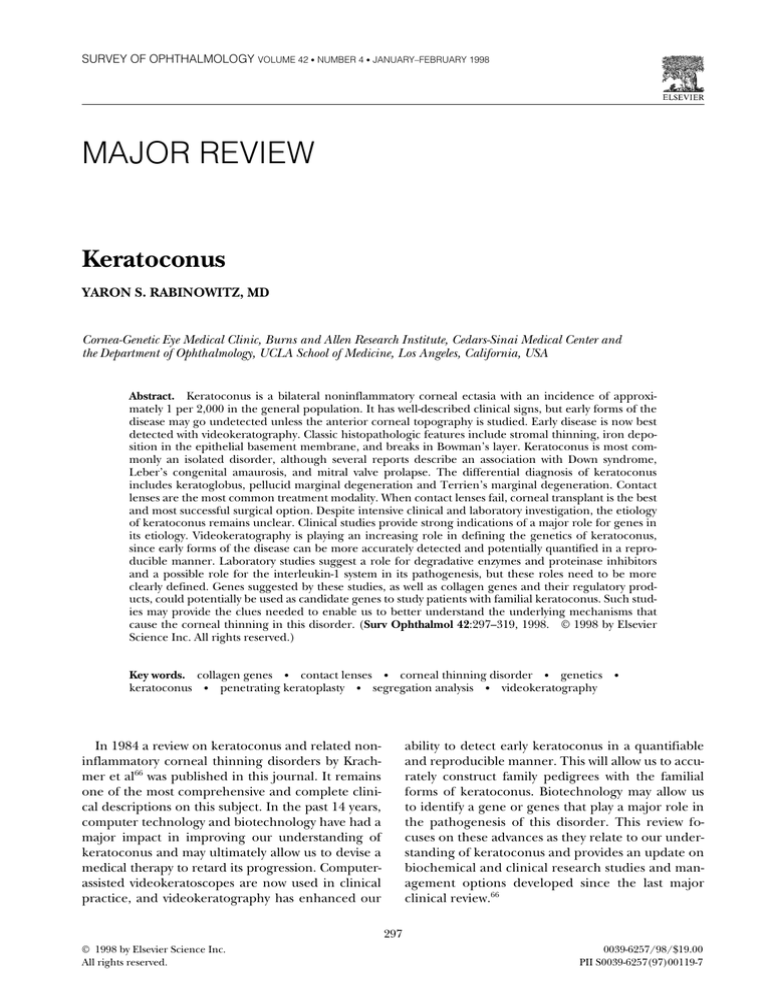
Abstract. Keratoconus is a bilateral noninflammatory corneal ectasia with an incidence of approximately 1 per 2,000 in the general population. It has well-described clinical signs, but early forms of the
disease may go undetected unless the anterior corneal topography is studied. Early disease is now best
detected with videokeratography. Classic histopathologic features include stromal thinning, iron deposition in the epithelial basement membrane, and breaks in Bowman’s layer. Keratoconus is most commonly an isolated disorder, although several reports describe an association with Down syndrome,
Leber’s congenital amaurosis, and mitral valve prolapse. The differential diagnosis of keratoconus
includes keratoglobus, pellucid marginal degeneration and Terrien’s marginal degeneration. Contact
lenses are the most common treatment modality. When contact lenses fail, corneal transplant is the best
and most successful surgical option. Despite intensive clinical and laboratory investigation, the etiology
of keratoconus remains unclear. Clinical studies provide strong indications of a major role for genes in
its etiology. Videokeratography is playing an increasing role in defining the genetics of keratoconus,
since early forms of the disease can be more accurately detected and potentially quantified in a reproducible manner. Laboratory studies suggest a role for degradative enzymes and proteinase inhibitors
and a possible role for the interleukin-1 system in its pathogenesis, but these roles need to be more
clearly defined. Genes suggested by these studies, as well as collagen genes and their regulatory products, could potentially be used as candidate genes to study patients with familial keratoconus. Such studies may provide the clues needed to enable us to better understand the underlying mechanisms that
cause the corneal thinning in this disorder. (Surv Ophthalmol 42:297–319, 1998. © 1998 by Elsevier
Science Inc. All rights reserved.)
Key words. collagen genes • contact lenses • corneal thinning disorder • genetics •
keratoconus • penetrating keratoplasty • segregation analysis • videokeratography
In 1984 a review on keratoconus and related noninflammatory corneal thinning disorders by Krachmer et al66 was published in this journal. It remains
one of the most comprehensive and complete clinical descriptions on this subject. In the past 14 years,
computer technology and biotechnology have had a
major impact in improving our understanding of
keratoconus and may ultimately allow us to devise a
medical therapy to retard its progression. Computerassisted videokeratoscopes are now used in clinical
practice, and videokeratography has enhanced our
ability to detect early keratoconus in a quantifiable
and reproducible manner. This will allow us to accurately construct family pedigrees with the familial
forms of keratoconus. Biotechnology may allow us
to identify a gene or genes that play a major role in
the pathogenesis of this disorder. This review focuses on these advances as they relate to our understanding of keratoconus and provides an update on
biochemical and clinical research studies and management options developed since the last major
clinical review.66
297
© 1998 by Elsevier Science Inc.
All rights reserved.
0039-6257/98/$19.00
PII S0039-6257(97)00119-7
298
Surv Ophthalmol 42 (4) January–February 1998
I. Epidemiology
Keratoconus, classically, has its onset at puberty
and is progressive until the third to fourth decade of
life, when it usually arrests. It may, however, commence later in life and progress or arrest at any age.
Rarely it may be congenital.134 It is most commonly an
isolated condition, despite multiple singular reports
of coexistence with other disorders (Table 1). Commonly recognized associations include Down syndrome, Leber’s congenital amaurosis, and connective
tissue disorders. For example, patients with advanced
keratoconus have been reported to have a high incidence of mitral valve prolapse (58%).66,129 Atopy , eye
rubbing, and hard contact lenses have also been reported to be highly associated with this disorder, and
6–8% of reported cases have a positive family history
or show evidence of familial transmission (Table 2).50,66
RABINOWITZ
The reported incidence of keratoconus varies,
with most estimates being between 50 and 230 per
100,000 in the general population (approximately 1
per 2,000). Prevalence is 54.5 per 100,000.27,35,55,60,66
The variability in the reported incidence reflects the
subjective criteria often used to establish the diagnosis, allowing subtle forms to be often overlooked.
Keratoconus occurs in all ethnic groups with no
male or female preponderance.
II. Clinical Features
Keratoconus is a condition in which the cornea assumes a conical shape as a result of noninflammatory thinning of the corneal stroma. The corneal
thinning induces irregular astigmatism, myopia, and
protrusion, leading to mild to marked impairment
in the quality of vision.66 It is a progressive disorder
TABLE 1
Diseases Reported in Association With Keratoconus
Multisystem Disorders
Alagille’s syndrome116
Albers-Schonberg disease40
Angleman syndrome75
Apert’s syndrome44
Autographism57
Anetoderma13
Bardet-Biedl syndrome37
Crouzon’s syndrome95,160
Down syndrome24
Ehlers-Danlos syndrome69
Goltz-Gorlin syndrome162
Hyperornithemia63
Icthyosis35
Kurz syndrome164
Laurence-Moon-Bardet-Biedl syndrome149
Marfan’s syndrome6
Mulvihil-Smith syndrome114
Nail patella syndrome49
Neurocutaneous angiomatosis38
Neurofibromatosis149
Noonan’s syndrome125
Osteogenesis imperfecta8
Oculodentodigital syndrome49
Pseudoxanthoma elasticum149
Rieger’s syndrome49
Rothmund’s syndrome62
Tourette’s disease32
Turner’s syndrome91
Xeroderma pigmentosa12
Other Systemic Disorders
Congenital hip dysplasia90
False chordae tendinae of left ventricle64
Joint hypermobility117
Mitral valve prolapse129
Measles retinopathy94
Ocular hypertension10
Thalesselis syndrome138
Reference numbers in superscript.
Ocular Disorders (Noncorneal)
Aniridia63
Anetoderma and bilateral subcapsular cataracts13
Ankyloblepharon15
Bilateral macular coloboma39
Blue sclerae49
Congenital cataracts64
Ectodermal and mesodermal anomalies68
Floppy eyelid syndrome87
Gyrate atrophy64
Iridoschisis29
Lebers congenital amaurosis30
Persistent pupillary membrane63
Posterior lenticonus16
Retinitis pigmentosa35
Retinal disinsection syndrome127
Retrolental fibroplasia74
Vernal conjunctivitis48
Corneal Disorders
Atopic keratoconjunctivitis48
Axenfeld’s anomaly135
Avellino’s dystrophy121
Chandler’s syndrome43
Corneal amyloidosis63
Deep filiform corneal dystrophy63
Essential iris atrophy11
Fleck corneal dystrophy63
Fuchs corneal dystrophy73
Iridocorneal dysgenesis5
Lattice dystrophy54
Microcornea63
Pellucid marginal degeneration59
Posterior polymorphous dystrophy26
Terriens marginal degeneration63
299
KERATOCONUS
TABLE 2
Signs of Keratoconus
External signs
Munson’s sign
Rizzuti phenomenon
Slit-lamp findings
Stromal thinning
Posterior stress lines (Vogt’s striae)
Iron ring (Fleischer ring)
Scarring—epithelial or subepithelial
Retroillumination signs
Scissoring on retinoscopy
Oil droplet sign (“Charleaux”)
Photokeratoscopy signs
Compression of mires inferotemporally
(“egg-shaped” mires)
Compression of mires inferiorly or centrally
Videokeratography signs
Localized increased surface power
Inferior superior dioptric asymmetry
Relative skewing of the steepest radial axes above and
below the horizontal meridian (Fig. 6)
ultimately affecting both eyes, although only one eye
may be affected initially.71,105
Symptoms are highly variable and, in part, depend
on the stage of the progression of the disorder. Early
in the disease there may be no symptoms, and keratoconus may be noted by the ophthalmologist simply
because the patient cannot be refracted to a clear
20/20 corrected vision. In advanced disease there is
significant distortion of vision accompanied by profound visual loss. Patients with keratoconus fortunately never become totally blind from their disease.
Clinical signs also differ depending on the severity
of the disease (Table 2). In moderate to advanced
disease any one or combination of the following
signs may be detectable by slit-lamp examination of
the cornea: stromal thinning (centrally or paracentrally, most commonly inferiorly or inferotemporally
[Fig. 1A]); conical protrusion; an iron line partially
or completely surrounding the cone (Fleischer’s
ring); and fine vertical lines in the deep stroma and
Descemet’s membrane that parallel the axis of the
cone and disappear transiently on gentle digital
pressure (Vogt’s striae [Fig. 2]). Other accompanying signs might include epithelial nebulae, anterior
stromal scars, enlarged corneal nerves, and increased intensity of the corneal endothelial reflex
and subepithelial fibrillary lines.66,80
Munson’s sign and Rizzuti’s sign are also useful adjunctive external signs associated with keratoconus.80
Munson’s sign is a V-shaped conformation of the
lower lid produced by the ectatic cornea in downgaze.
Rizzuti’s sign is a sharply focused beam of light near
the nasal limbus, produced by lateral illumination of
the cornea in patients with advanced keratoconus.
Fig. 1. Ectatic dystrophies, the arrows point to the areas
of maximal thinning. Top: Keratoconus-paracentral corneal thinning. Center: Pellucid marginal degenerationinferior thinning from 4 to 8 o’clock. Bottom: Keratoglobus: thinning of the whole cornea from limbus to limbus.
Patients with advanced disease may occasionally
present with a sudden onset of visual loss accompanied by pain. On slit-lamp examination the conjunctiva may be injected and a diffuse stromal opacity is
noted in the cornea. This condition, referred to as
“hydrops,” is caused by breaks in Descemet’s membrane with stromal imbibition of aqueous through
these breaks (Fig. 3A). The edema may persist for
weeks or months, usually diminishing gradually, with
relief of pain and resolution of the redness and cor-
300
Surv Ophthalmol 42 (4) January–February 1998
RABINOWITZ
Fig. 2. Vogt’s striae in a patient with keratoconus located
at the level of Descemet’s membrane noted on slit-lamp
examination of the cornea. (Courtesy of Stephen Orlin, MD.)
neal edema ultimately being replaced by scarring
(Fig. 3B).
Early in the disease process the cornea may appear normal on slit-lamp biomicroscopy; however,
there may be slight distortion or steepening of
keratometry mires centrally or inferiorly. In such instances it is useful to dilate the pupil. Retroillumination techniques and scissoring of the retinoscopic reflex or the “Charleux” oil droplet sign are useful
clinical signs to confirm the diagnosis in suspicious
cases.102 In these early cases, where the cornea appears normal but keratoconus is suspected, measuring the anterior topography of the central and paracentral cornea is also extremely useful to confirm
the diagnosis.66
TABLE 3
Collagens in the Cornea and Their Chromosomal Location
Collagen
Type
I
III
IV
V
VI
VII
VIII
Chain
Gene
alpha 1 (I)
alpha 2 (I)
alpha 1 (III)
alpha 1 (IV)
alpha 2 (IV)
alpha 3 (IV)
alpha 4 (IV)
alpha 5 (IV)
alpha 1 (V)
alpha 2 (V)
alpha 3 (V)
alpha 1 (VI)
alpha 2 (VI)
alpha 3 (VI)
alpha (VII)
alpha 1 (VIII)
alpha 2 (VIII)
COL1A1
COL1A2
COL3A1
COL4A1
COL4A2
COL4A3
COL4A4
COL4A5
COL5A1
COL5A2
COL5A3
COL6A1
COL6A2
COL6A3
COL7A1
COL8A1
COL8A2
Chromosomal
Location
17q21-q22
7q21-q22
2q31-q32
13q33-q34
13q33-q34
2
2
X
2q31-q32
9p
2q31-q32
22q
22q
6
3q
3
1
Fig. 3. Acute hydrops. Top: Stromal opacity as a result
of corneal edema noted on initial presentation. Bottom:
Resolution of the hydrops with resultant corneal scarring
in the same patient 6 months later.
Several devices are currently available for detecting early keratoconus by measuring anterior corneal
topography. These range from simple inexpensive
devices, such as handheld keratoscopes (placido
disks), to expensive sophisticated devices, such as
computer-assisted videokeratoscopes. With the handheld keratoscopes, such as the Klein keratoscope,
early keratoconus is characterized by a downward
deviation of the horizontal axis of the Placido disk
reflection (Fig. 4).3,4 Until recently, nine-ring photokeratoscopes, such as the Corneascope (Kera Corporation, Santa Clara, CA), were commonly used by
cornea specialists. With this device early keratoconus
is depicted by compression of the mires inferiorly or
inferotemporally120 (Fig. 5).
Computer-assisted videokeratoscopes, which generate color-coded maps and topographic indices, are
currently the most sensitive and sophisticated devices for confirming the diagnosis of keratoconus.
(A more detailed discussion is provided in “V. Topographic Studies of Keratoconus.”78) With such devices, keratoconus appears as an area of increased
surface power surrounded by concentric zones of
decreasing surface power. Three features are common to keratoconus videokeratographs that use sag-
KERATOCONUS
301
Fig. 4. Photographic placido disk images used by Amsler. Left: Normal cornea. Right: Deflection of the horizontal meridian labeled as keratoconus “fruste.”
ittal topography, a localized area of increased surface power, inferior-superior power asymmetry, and
skewed steep radial axes above and below the horizontal meridian (depicting irregular astigmatism,
the hallmark of keratoconus [Fig. 6]).103,156
Ultrasonic pachymetry may be useful to confirm
corneal thinning in patients with suspected keratoconus on slit-lamp examination or videokeratography; however, it cannot be solely relied on to make
the diagnosis because of the large range and variation of pachymetry readings both centrally and paracentrally in the normal population.112
III. Histopathology
Thinning of the corneal stroma, breaks in Bowman’s layer, and deposition of iron in the basal lay-
Fig. 5. Egg-shaped mires or inferotemporal steepening
detected with the Corneascope (nine-ring photokeratoscope) in a patient with early keratoconus.
ers of the corneal epithelium comprise a triad of the
classical histopathologic features found in keratoconus (Fig. 7). Depending on the stage of the disease,
every layer and tissue of the cornea can, however, become involved in the pathological process. Fine details of these processes are most clearly appreciated
by electron microscopy.
The epithelium may show degeneration of its
basal cells, breaks accompanied by downgrowth of
epithelium into Bowman’s layer, particles within a
thickened subepithelial basement membranelike
layer and between basal epithelial cells, and accumulation of ferritin particles within and between epithelial cells most prominently in the basal layer of
the epithelium. Histopathologic features detected in
Bowman’s layer may include breaks filled by eruptions of underlying stromal collagen, periodic acid
Schiff–positive nodules, and Z-shaped interruptions, possibly due to separation of collagen bundles
and reticular scarring. Features noted in the stroma
are compaction and loss of arrangement of fibrils in
the anterior stroma, decrease in the number of collagen lamellae, normal and degenerating fibroblasts
in addition to keratocytes, and fine granular and microfibrillar material associated with the keratocytes.66
Descemet’s membrane is rarely affected except
for breaks seen in acute hydrops. The endothelium
is usually normal. However, some abnormalities have
been reported, including intracellular “dark structures,” pleomorphism, and elongation of cells with
their long axis toward the cone. Gross histopathologic analysis of corneal buttons undergoing penetrating keratoplasty for keratoconus has revealed the
presence of two types of cone morphology: “nipple”-
302
Surv Ophthalmol 42 (4) January–February 1998
RABINOWITZ
Fig. 6. Top: Keratoconus videokeratograph (TMS-1 videokeratoscope) demonstrating the three classical phenotypic features of keratoconus (using
sagittal topography): central steepening, inferior-superior dioptric asymmetry, and skewing of the steepest radial
axes above and below the horizontal
meridian. Bottom: Diagram illustrating calculation of the SRAX index that
quantifies the skewing of these radial
axes.
IV. Etiology and Pathogenesis
A. ASSOCIATED DISORDERS
type cones, located centrally, and “oval”-(sagging)
type cones, located inferiorly or inferotemporally.96
These types of cones often can be distinguished on
slit-lamp examination or evaluation of the anterior
corneal topography in keratoconus patients.
Histopathologic examination of corneal buttons
in patients who have had acute hydrops reveals stromal edema. Descemet’s membrane separates from
the posterior surface and retracts into scrolls, ledges,
or ridges. During the repair process, corneal endothelium extends over the anterior and posterior surfaces of the detached Descemet’s membrane and
denuded stroma: endothelial integrity is usually reestablished 3–4 months after the acute event.136
Keratoconus has been reported in various clinical
settings. It may be an isolated sporadic disorder, or it
may be associated with other rare genetic disorders,
with Down syndrome and Leber’s congenital amaurosis, with connective tissue disorders, with hard
contact lens wear and eye rubbing, and with a positive family history of the disorder.53,66,83,84 These associations, however, require critical evaluation.
By far the most common presentation of keratoconus is as an isolated sporadic disorder with no other
associated systemic or ocular disease detectable by
clinical evaluation. Of 300 consecutive keratoconus
patients screened for a genetic research study at the
Cedars-Sinai Medical Center in Los Angeles, 2 (0.6%)
had Down syndrome, 2 (0.6%) had neurofibromatosis, and 296 (99%) were isolated with no associated
genetic disease.
Table 1 summarizes conditions reported to be associated with keratoconus. For the most part, these
associations should be considered to have occurred
by chance. For example, the incidence of keratoconus is 1 per 2,000 and the incidence of neurofibromatosis type 1 is 1 per 4,000 in the general population; thus, there is a 1 in 8,000,000 chance that these
two disorders would occur together (30 potential
cases in the USA). Rare associations with keratoconus are important, particularly if they occur as a result of a chromosomal translocation; if the associated disorder cosegregates with keratoconus it might
provide clues as to the chromosomal location of the
inherited form of keratoconus. Therefore, it is
worthwhile to perform cytogenetic studies in patients who have mental retardation or rare genetic
KERATOCONUS
Fig. 7. Classical histopathologic features seen in keratoconus. Top: Stromal thinning with folding artifact commonly seen in thinned corneas. (Courtsey of Joseph Sassani, MD.) Center: Breaks in Bowman’s layer (arrow).
(Courtesy of Gordon Klintworth, MD.) Bottom: Deposition of iron in the basal epithelium (arrow). (Courtesy of
Joseph Sassani, MD.)
disorders attributed to chromosomal translocations
and associated with keratoconus.
Down syndrome has been reported to have a high
association with keratoconus, with reported incidence ranging from 0.5% to 15% (i.e., 10–300 times
more common than in the general population).24,66,128 Similarly, there is a high incidence of
keratoconus in patients with Leber’s congenital
amaurosis (up to 30% of patients older than 15
years).2 The frequent occurrence of keratoconus has
been attributed to a high incidence of eye rubbing
303
in these two disorders, owing to increased blepharitis in Down syndrome and an oculo-digital sign in
Leber’s congenital amaurosis. However, a recent
study of children in a school for the blind by Elder30
contradicts this theory and suggests that the association with keratoconus might be due to genetic factors rather than eye rubbing.
Several reports suggest an association between
keratoconus and connective tissue disorders.58,62,83,
84,117
This is based on rare reports of associations of
keratoconus with disorders of collagen metabolism,
such as Osteogenesis Imperfecta and subtypes of
Ehlers-Danlos syndrome, and on a study that reported joint hypermobility in 22 of 44 (50%) keratoconus patients. Two recent studies, however, dispute
this high association of joint hypermobility, one by
an Emory University (Atlanta, GA) group137 and one
by our group at the Cedars-Sinai Medical Center. In
our study 34 of 218 (15%) keratoconus patients
compared to 10 of 183 (12%) normal age-matched
controls had joint hypermobility (not statistically significant (P 5 0.304).141 Other compelling evidence
in support of a connective tissue abnormality in keratoconus does, however, exist, based on two reports of
an association between patients with advanced keratoconus and mitral valve prolapse—a 1982 study by
Beardsley and Foulks7 and a more recent study by
Sharif et al,129 which suggests that 58% of keratoconus patients requiring surgery have mitral valve prolapse versus 7% of normal controls.
Mechanical trauma has also been implicated in
the pathogenesis of keratoconus. Although a number of studies report a high association of eye rubbing with keratoconus, a cause-and-effect relationship is difficult to prove.66 A recent preliminary study
at our institution, however, suggests that keratoconus patients do rub their eyes more often than normal controls (174 of 218 [80%] versus 106 of 183
[58%] [P , 0.001]).141 Contact lenses are also suggested as a source of mechanical trauma related to
keratoconus.42,53,66 Because early in the disease process patients have mild myopic astigmatism with clinically normal-looking corneas and their vision is best
corrected with rigid contact lenses, it is extremely
difficult to determine which came first, the keratoconus or contact lens wear. In none of the reports citing these associations were topographic studies performed prior to contact lens fitting to determine
whether the patients had early disease before wearing contact lenses. It is possible that mechanical
trauma induced by eye rubbing and hard contact
lens wear act as environmental factors that enhance
the progression of the disorder in genetically predisposed individuals.
Atopy is often cited as being highly associated with
keratoconus. A review of the literature reveals con-
304
Surv Ophthalmol 42 (4) January–February 1998
flicting data in favor of and against this association.66,87,113,147 In a study conducted at our institution,
96 of 218 (44%) keratoconus patients had a history
or symptoms of allergic disorders versus 66 of 183
(36%) normal age-matched controls (not statistically significant, P 5 0.105)141
B. BIOCHEMICAL STUDIES
Despite intensive biochemical investigation into
the pathogenesis of keratoconus, the underlying biochemical process and its etiologic basis remain
poorly understood. Corneal thinning appears to result from loss of structural components in the cornea, but why this occurs is not clear. Theoretically,
the cornea can thin because it has fewer collagen
lamellae than normal, fewer collagen fibrils per
lamella, closer packing of collagen fibrils, or various
combinations of these factors. These conditions may
result from defective formation of extracellular constituents of corneal tissue, a destruction of previously
formed components, an increased distensibility of
corneal tissue with sliding collagen fibers or collagen
lamellae, or a combination of these mechanisms.63
Early biochemical studies demonstrated that collagen composition in corneas with keratoconus was
unaltered.163 Recent biochemical assays and immunohistological studies of corneas with keratoconus
suggest that the loss of corneal stroma after digestion by proteolytic enzymes could be caused by increased levels of proteases and other catabolic
enzymes123 or decreased levels of proteinase inhibitors.41 Observations of corneal a1 proteinase inhibitor and a2 macroglobulin (also a major proteinase
inhibitor) confer further support to the hypothesis
that the degradation process may be aberrant in
keratoconus.122 Both inhibitors can be demonstrated
immunohistochemically in the epithelium, stroma,
and endothelium of normal and pathologic human
corneas. In contrast to normal corneas and corneas
with other pathologic conditions, the staining intensity in the corneal epithelium of keratoconus corneas was markedly diminished. This decrease in a2
macroglobulin in the cornea and stroma was confirmed by Western blot assays.122 Another proteinase
inhibitor (TIMP-1) that inhibits matrix metalloproteinase was found not to contribute to the increased
levels of gelatinolytic activity noted in prior biochemical studies of the cornea.61,92,133 These proteases and
inhibitors require further study to clarify their precise
role in the pathogenesis of keratoconus.
The preceding biochemical findings may merely
be signs of a more generalized keratocyte abnormality in keratoconus.153 Wilson and coworkers demonstrated that the loss of anterior stromal keratocytes,
which accompanies corneal epithelial abrasion or
subepithelial ablation, is likely due to apoptotic cell
RABINOWITZ
death.153 They point out that both the corneal epithelium and endothelium produce interleukin-1
(IL-1) and that keratocytes can be shown to express
the IL-1 receptor. Interleukin-1 induces keratocyte
death in vitro and negative keratocyte chemotaxis,
and it can upregulate hepatocyte and keratinocyte
growth factors.153 It can also regulate the expression
of keratocyte metalloproteinases collagenase and
complement factors. On the basis of this, IL-1 is postulated to be a modulator of epithelial stromal interactions, with a role in the regulation of corneal cell
proliferation, differentiation, and death.
Wilson et al have proposed a role for an IL-1 system in the cornea in the pathogenesis of keratoconus.153 It has previously been demonstrated that
keratocytes from keratoconus corneas have a fourfold greater number of IL-1 receptors than normal
corneas9; Wilson et al suggest that the increased expression of the IL-1 receptor sensitizes the keratocytes to IL-1 released from the epithelium or endothelium, causing a loss of keratocytes through
apoptosis and a decrease in stromal mass over time.
This hypothesis makes sense of the occurrence of
keratoconus in relation to eye rubbing, contact lens
wear, and atopy, if it is presumed that epithelial microtrauma leads to an increased release of IL-1 from
the epithelium.14 Wilson et al have also suggested
that abnormalities in the processes that regulate apoptosis, besides the IL-1 system, could be the cause
of keratoconus, even in the absence of epithelial cell
injury.153
C. GENETICS
1. Twin Studies
Although formal genetic analyses using current
methodology have not been reported for keratoconus, review of the published literature provides
strong pointers to suggest genetic influences in the
pathogenesis of this disorder. This includes at least
eight reports of its occurrence in both identical
twins,33,66,93 the bilaterality of the disorder,71,105 the
high degree of nonsuperimposable mirror image
symmetry in the location of topographic alterations
between two eyes of an individual patient,156 and
multiple reports of its occurrence in family members
in two and three generations.36
Twins have a special place in the study of human
genetics because of their usefulness in comparing
the effects of genes and environment. The importance of twin studies for comparison of the effects of
nature and nurture was originally pointed out by
Galton in 1875.139 Diseases caused wholly or partly by
genetic factors have a higher concordance rate in
monozygotic twins than in dizygotic twins. In situations where a condition does not show a simple genetic pattern, comparison of its incidence in
305
KERATOCONUS
monozygotic and dizygotic twin pairs can reveal that
heredity is involved; moreover, if monozygotic twins
are not fully concordant for a given condition, nongenetic factors must also play a part in its etiology.
Nine cases of keratoconus in monozygous twins
have been reported in the literature; in all instances
but one, both twins had keratoconus. In the one
who did not have keratoconus, videokeratography
had not been performed. We have observed at least
two sets of twins in which one had clinical keratoconus while the other was affected only as shown by
videokeratography, and two sets of dizygotic twins in
which one was affected and the other normal as
shown both clinically and by videokeratography.
These observations present very strong support for
genetic influences in keratoconus; however, a formal
prospective twin study comparing monozygotic versus dizygotic twins without ascertainment bias is necessary to confirm the conclusions drawn from such
observations.21,139
2. Family Studies
Several large series, including our own study at
Cedars-Sinai Medical Center, have reported a positive family history in 6–10% of patients with keratoconus.51,141 The majority of reported studies suggested an autosomal dominant mode of inheritance
with variable expression and included subtle forms
of the disorder, such as keratoconus fruste or mild
irregular astigmatism, in order to resolve the mode
of inheritance. At least 74 such instances have been
reported in the ophthalmic literature: 21 cases cited
by Falls and Allen,34 including one by Falls; 24 cases
examined by Ihalainen in a Finnish study;56 and 10
families examined by Hammerstien.51 In Hammerstien’s study of 52 families, keratoconus was detected
in 2 or more relatives in 10 of the families (19%).
The degree of penetrance was approximately 20%.
The disease was characterized by complete penetrance and variable expressivity. Seven pedigrees
were reported by Redmond,115 who suggested that
keratoconus fruste and high degrees of astigmatism
represent incomplete expression of the keratoconus
gene and should be taken into account in pedigree
analysis. Five families of patients with keratoconus
were reported by Rabinowitz et al,101 who used
videokeratography to detect abortive forms of the
disorder. In these five families, hereditary patterns
were consistent with autosomal dominant transmission with variable expressivity (Fig. 8). Gonzalez and
McDonnell46 detected videokeratographic abnormalities in at least one parent of seven sets of clinically normal parents of patients with keratoconus.
Although there are several reports in the literature
that suggest recessive inheritance,36 none show clear
evidence that three generations were examined or
Fig. 8. Family pedigrees of subjects studied with videokeratography. Subtle topographic abnormalities in clinically normal family members detectable by videokeratography only suggests a hereditary pattern consistent with
autosomal dominance and variable expression. (Reprinted
from Rabinowitz et al101 with permission of the American
Medical Association.)
that subtle forms of the disorder were sought for inclusion in the pedigree analysis.
3. Formal Genetic Analyses
Although most studies suggest a dominant mode
of inheritance, formal genetic analyses are needed
to accurately define hereditary patterns for various
subtypes of keratoconus and elucidate the role genetic influences may play in its pathogenesis. Formal
genetic analyses of a disease or trait are used to test
whether there is a significant genetic influence in
the etiology of the disease and to identify both the
modes of inheritance of any responsible genes and
their locations in the human genome. In a genetic
analysis, the first question to be investigated is
whether familial aggregation is the result of genetic
factors.
a. Molecular Genetic Studies
Once genetic factors have been established, the
goal of further analysis is to investigate the number
of genes that influence the disease (one, two, or
many), the relative contribution of each of the genes
to the development of the disease, the mode of in-
306
Surv Ophthalmol 42 (4) January–February 1998
heritance of the genes, the presence or absence of
genetic heterogeneity (one or more diseases with a
similar phenotype), and the chromosomal location
of the gene(s). Such information has not yet formally been attained for keratoconus, but with the
rapid development of molecular and statistical
methods, these goals are now achievable and are
currently being pursued at our institution.21,110
Segregation analysis is a statistical method used to
evaluate the mode of inheritance of a trait or disease.21,31,86 A particular mode of inheritance is postulated for the disease, and data on the presence or absence of the disease are collected from families with
affected members. These data are used to test
whether the expression of the disease is consistent
with the proposed mode of inheritance. The variables analyzed in classic segregation analysis are the
presence or absence of disease, which can be based
on a qualitative or discrete (quantitative) trait. Qualitative criteria for diagnosis of keratoconus include
corneal thinning, Vogt’s striae, Fleischer rings, and
scissoring of the retinoscopic reflex with a dilated
pupil. For quantitative traits, for which clear cutoff
points for affectation status are required and complex, segregation analyses using computer programs
are preferred because such methods glean more information from the data.21 For discrete cutoff points
for diagnosis using quantitative traits, videokeratoscopy indices can be used. To develop these cutoff
points, a clear, quantifiable, and reproducible definition of early keratoconus by videokeratoscopy in
the absence of clinical signs is necessary. Because
keratoconus appears to be a complex disorder, not
always following simple mendelian modes of inheritance, videokeratoscopy research to provide minimal
topographic criteria for determining affectation status provides a unique opportunity to determine true
modes of inheritance and ultimately construct pedigrees for molecular genetic analysis in appropriate
families with keratoconus.104 Before expensive molecular studies are undertaken to investigate the heredity and genetics of keratoconus, several areas
must be clarified through formal analysis. A definition of the disorder must be established. The influence of associated systemic conditions and the effect
of mechanical trauma must be determined, and topographical changes in contact lens wearers must be
identified.126 After these factors are understood, the
relationship of expressivity to age and the potential
heterogeneity of keratoconus can be determined.
Once the early phenotype has been characterized
and segregation analysis has been performed, accurate family pedigrees with familial keratoconus can
be constructed. This may open new avenues for investigating the pathobiology of keratoconus through
gene-linkage analysis.23,131 A random marker ap-
RABINOWITZ
proach with polymorphic microsatellite markers or a
candidate-gene approach could be used in appropriate families to identify a gene locus (or multiple
loci) and answer some important questions that
have been suggested by clinical and biochemical observations. Is keratoconus caused by degradative enzymes, as suggested by biochemical studies? Is there
a role for the IL-1 system as previously outlined? Is
keratoconus caused by a structural abnormality of
collagen or products involved in its regulation, as
suggested by clinical observations?
To provide answers to some of the questions
raised by findings in biochemical studies, cDNAs of
the proteinase inhibitors, proteases, or components
of the IL-1 system could be used as candidate genes
in appropriate linkage studies of appropriate keratoconus families. Such studies may provide more definitive support for their role in the thinning process
resulting in keratoconus.
b. Collagen Genes as Candidate Genes
The role of collagen and products involved in its
regulation is receiving intense scrutiny at our institution. The high association of advanced keratoconus
and mitral valve prolapse, prior reports of an association between Osteogenesis Imperfecta, and a recent
report in which keratoconus cosegregates with familial osteogenesis imperfecta in three generations
points to a genetic abnormality of connective tissue
being responsible for at least some forms of keratoconus.8,129 Different subtypes of Osteogenesis Imperfecta have been shown to be caused by mutations in
the COL1A1 and COL1A2 genes.118 To test the hypothesis that some forms of keratoconus may result
from a mutation in one of the fibrillar collagens in
the cornea, we are using the complementary DNAs
of the fibrillar collagens to study one large family
with autosomal dominant keratoconus, using a candidate-gene approach.140
The collagens form a multigene family with more
than 28 members, the genes for which are known to
be dispersed to at least 12 chromosomes. As a family
of proteins, the collagens are the most abundant in
the body. The vast majority of collagen in the body is
type I collagen, which is ubiquitously distributed and
is the major protein in bone, skin, ligament, sclera,
cornea, blood vessels, and hollow organs. Mutations
that affect the structure or processing of the chains
of type I collagen are often expressed as generalized,
connective tissue disorders, although the specific tissue in which the major effect is seen may vary and
determines the clinical phenotype. With the exception of types III, V, and VI collagen, which are also
distributed in virtually all tissues, most other collagens have tissue-specific or structure-specific distribution.20 Types II, IX, X, and XI are found in hya-
307
KERATOCONUS
line cartilage and the vitreous of the eye, type IV
collagens are found in basement membranes, and
type VII collagen is found at some epithelial-mesenchymal junctions in anchoring fibril structures. Because of differences in structure, expression, and tissue distribution, the collagens perform different
functions; in different tissues the same collagen may
perform different functions.20
Collagens throughout the body function in a
number of ways. They provide tensile strength, facilitate transparency, provide form during embryonic
and fetal development, interact with other proteins
to build tissues and organs, separate cell layers during and after development, and provide filtration
barriers between spaces. It is likely that some of the
functions are achieved as a direct result of collagen
structure, while others depend on interactions with
additional matrix macromolecules.20
Collagens type I, III, IV, V, VI, VII, and VIII are
scattered throughout different layers of the cornea
(Fig. 9). The chromosomal location of the genes encoding these collagens have been identified (Table
3).20,163 These genes thus serve as excellent candidate genes for studying keratoconus. Their inclusion
or exclusion could yield valuable information. Preliminary studies at our institution using molecular
genetic approaches have excluded several collagen
genes (Table 4). COL1A1 and COL1A2 remain excellent candidates and are currently being investigated
in more detail, as are new markers distal to COL6A1
and COL6A2 on the telomere of chromosome 21.
Fig. 9.
4. Summary
Clinical observations, topographic studies, and
preliminary segregation analyses of families of patients with keratoconus suggest that genes play a major role in the etiology of keratoconus.101,105,106,110 Environmental factors such as eye rubbing and hard
contact lens wear may cause progression of this disorder in genetically susceptible individuals. The heterogenous nature of the disease suggests that different genetic subtypes might result from different
mutations and that not all families with keratoconus
will follow classical mendelian patterns of inheritance. Despite the fact that to date we have made very
little progress toward understanding what causes
keratoconus, molecular genetic approaches with
DNA markers of families with keratoconus have
great potential for providing pointers to an underlying genetic abnormality that causes the noninflammatory corneal thinning found in keratoconus. This
may ultimately lay the foundation for possible gene
therapy to retard progression of the disorder in
high-risk individuals.23,131
V. Topographic Studies of Keratoconus
A. PLACIDO DISK STUDIES
In 1938 Marc Amsler, using a photographic placido disk, was the first to describe early corneal topographic changes in keratoconus before clinical or
biomicroscopic signs could be detected. His classical
studies on the natural history of keratoconus docu-
Diagram illustrating the distribution of collagens in the cornea.
308
Surv Ophthalmol 42 (4) January–February 1998
RABINOWITZ
TABLE 4
Preliminary Linkage Studies With Collagen Genes as Candidate Genes in Autosomal Dominant Keratoconus104
Two-Point LOD Scores Calculated With LIPED
Keratoconus Z at 0 5
versus _______
COL3A1/COL5A2
COL2A1
GH1/COL1A1*
COL6A1/COL6A2
0.01
27.36
21.81
27.43
0.05
22.39
20.20
22.39
22.35
0.10
21.58
0.01
21.55
0.20
20.84
0.12
20.79
0.30
20.45
0.09
20.42
0.40
20.19
0.03
20.19
*GH1 was used as a marker for COL1A1 because there were no good markers for COL1A1 at the time this study was performed.
mented its progression from minor corneal surface
distortions to clinically detectable keratoconus. He
classified keratoconus into clinically recognizable
stages and an earlier latent stage recognizable only
by placido disk examination of corneal topography.
These early stages were subdivided into two categories: keratoconus fruste, in which there is a 1–4 degree
deviation of the horizontal axis of the placido disk,
and early or mild keratoconus, which has a 4–8 degree
deviation. Only slight degrees of asymmetric oblique
astigmatism could be detected in these early forms.
Similar findings were absent in patients with regular
astigmatism.3,4
In Amsler’s study of 600 patients, 22% had clinically obvious keratoconus in both eyes, 26% had
clinical keratoconus in one eye and latent keratoconus in the other, and 52% had latent keratoconus bilaterally. Progression was highly variable and most
often asymmetric. The cone could remain stationary, progress rapidly over 3–5 years, and arrest or
progress intermittently over an extended period of
time. When Amsler reexamined 286 eyes 3–8 years
after the diagnosis, only 20% of the entire group, including 66% of the latent cases, had progressed. Progression was most likely to occur in patients between
10 and 20 years of age, decreased slightly between
ages 20 and 30, and was less likely to increase after
age 30.3,4
Levene suggests that instrument tilt or poor alignment with respect to the corneal plane in hand held
keratoscopes may result in incorrect interpretation
of the deviation of the horizontal axis.72 Reproducibility thus poses a potential problem with this device.
B. PHOTOKERATOSCOPY
The photokeratoscope produces a topographic
record of 55–80% of the total corneal contour, but it
provides little or no information about the central 3
mm of the cornea. Rowsey et al used this instrument
to study keratoconus and its progression in 827 patients.25,120 The earliest sign detected, in the absence
of biomicroscopic signs, was steepening of the inferotemporal cornea, extending peripherally over time
to involve the inferonasal, superotemporal and, last,
the superonasal quadrant.
C. KERATOMETRY
The ophthalmometer (keratometer), which provides information about only 2–3 points approximately 3 mm apart, can detect keratoconus by showing distortion of its mires or central or inferior
steepening. While steep corneas might suggest keratoconus, there are patients with steep corneas and
high degrees of regular astigmatism who do not
have keratoconus. Conversely, there are patients
who have keratoconus with normal central corneal
curvatures but irregular astigmatism or inferior
steepening only. A documented increase in corneal
curvature over time as seen by keratometry is a sensitive indicator of keratoconus.66
D. COMPUTER-ASSISTED VIDEOKERATOSCOPY
Over the past 7 years computer-assisted videokeratoscopes have gained rapid acceptance in clinical
practice.65 Many such devices are currently available,
most using placido disk principles, although other
technologies are rapidly emerging. (For a detailed
discussion of computer-assisted videokeratoscopes,
refer to “Corneal Topography” in The Clinical Atlas,
by Lucio Burrato.84a)
The instrument we have used primarily in our topography studies is the Topographic Modeling System (TMS-1, Computed Anatomy, New York, NY). It
consists of a placido disk-type nose cone, capturing
the placido disk image into a computer-based system, which can rapidly analyze data accurately and
reproducibly. Both the central and paracentral cornea can be measured in one sitting. This device,
which uses spherically biased algorithms (sagittal topography), has previously been described in detail
and has been shown to be highly accurate and reproducible on spherical surfaces and in the central two
thirds of normal human corneas.47,52,81,159 Topographic data points in polar coordinates using 256
radial lines scanning across 25 rings are examined
and approximately 7,000 data points are generated.
KERATOCONUS
A color-coded map that allows easy appreciation of
changes in the corneal curvature is generated. The
25-ring photokeratoscope mires can be superimposed on the maps for qualitative interpretation,
and a series of quantitative indices, including simulated keratometry readings, are part of the data output.47 Because placido disk–based computer videokeratoscopes, such as the TMS-1, have the combined
features of both a keratometer and photokeratoscope, recording curvature changes in both the central and paracentral cornea, they are ideally suited
for detecting subtle topographic changes present in
early keratoconus and for documenting their progression by serial topographic analysis.
E. VIDEOKERATOGRAPHY STUDIES
OF KERATOCONUS
Several studies have been performed to characterize the topographic phenotype of clinically detectable keratoconus by videokeratography.103,156 The
majority of patients have peripheral cones, with
steepening extending into the periphery. The steepening in this group is usually confined to one or two
quadrants. A smaller group of patients have central
topographic alterations. Many central cones have a
bow tie configuration similar to that found in naturally occurring astigmatism. In the keratoconus patients, however, the bow tie pattern is asymmetric,
with the inferior loop being larger in most instances.
In contrast to eyes having with-the-rule astigmatism,
the steep radial axes above and below the horizontal
meridian in keratoconus appear skewed, giving the
bow tie a lazy-eight configuration. Another pattern
309
found in central cones is more symmetric steepening without a bow tie appearance. The pattern is
usually the same in both eyes, although it may be
more advanced in one eye than in the other. The peripheral and central cones probably correspond
roughly to the oval sagging and nipple-shaped cones
described by Perry et al.96
In summary, keratoconus has three characteristics
seen by videokeratography that are not present in
normals: an increased area of corneal power surrounded by concentric areas of decreasing power,
inferior-superior power asymmetry, and skewing of
the steepest radial axes above and below the horizonal meridian (Fig. 6).
F. VIDEOKERATOGRAPHY PATTERN
RECOGNITION: NORMAL VERSUS KERATOCONUS
Similar patterns have been noted in clinically normal family members of keratoconus patients and in
the clinically normal fellow eyes of patients with clinically unilateral keratoconus.80,101,105 These patterns
are, however, milder (as measured by dioptric
power) than the patterns noted in clinically obvious
keratoconus (Fig. 10).
While it is relatively easy to recognize patterns
with color-coded maps once a practitioner has
gained experience through observing many topographic maps, it is confusing and difficult for clinicians who are inexperienced with this technique to
identify the minimal topographic criteria required
for a diagnosis of keratoconus based on pattern recognition of a videokeratograph alone. Therefore, it
Fig. 10. Videokeratograph of forme
fruste keratoconus in a clinically normal family member of a patient with
familial keratoconus (see Fig. 8, A-II5). This videokeratograph has similar
but milder features than those noted
in keratoconus.
310
Surv Ophthalmol 42 (4) January–February 1998
has been recommended that maps that look suspicious for keratoconus in the presence of a clinically
normal eye be labelled “keratoconus suspect” until
progression to keratoconus can be documented.151
One way to become proficient in recognizing subtle
pathology is to print maps of all patients examined
in the absolute scale (in the TMS-1 this scale divides
the cornea into 1.5 diopter [D] intervals between
35 and 50 D and 5 D intervals outside of this
range).47,155 This singular scale allows the clinician to
get used to patterns descriptive of normal topography, allowing earlier recognition of subtle abnormal
topography. The normalized scale in this device,
which divides the cornea into 11 equal colors, is confusing, and many clinically normal patients with
slight inferior steepening might inadvertently be labelled as suspect using this scale. For the purposes of
our research in trying to define an early keratoconus
phenotype by videokeratography, we have compiled
a database of normal videokeratography patterns of
195 normal individuals using this absolute scale (Fig.
11). This baseline database of videokeratography
patterns (sagittal topography) to be used as a reference for our longitudinal topographic studies of
keratoconus family members can also help the clinician in determining whether subtle deviations in
corneal topography exist in a particular patient observed at any time. While it has not yet been determined which patterns ultimately progress to keratoconus, our database of videokeratography patterns
suggests that only 1 in 195 (0.5%) normal patients
have mild topographic features similar to, but
milder than, those seen in clinically detectable keratoconus asymmetric bow tie with skewed radial axes
([AB/SRAX] pattern, Fig. 11).108
G. VIDEOKERATOGRAPHIC
“PSEUDOKERATOCONUS”
Another source of confusion in assigning minimal
topographic criteria for keratoconus are videokeratography patterns simulating keratoconus (videokeratographic pseudokeratoconus).102,154,157 The most
common culprit is contact lens wear (both hard and
soft), which induces patterns of inferior steepening
that may be very difficult to distinguish from keratoconus.157 These patterns, however, disappear with
time after contact lens wear is discontinued. Videokeratographic pseudokeratoconus may also result
from technical errors during videocapturing, such
as inferior eyeball compression, misalignment of the
eye with inferior or superior rotation of the globe
(Fig. 12), and incomplete digitization of mires, causing formation of dry spots, which simulates inferior
steepening. Early pellucid marginal degeneration,
inflammatory corneal thinning, and previous ocular
surgery can all induce patterns that simulate kerato-
RABINOWITZ
Fig. 11. Classification scheme of normal videokeratographs in the absolute scale devised as a baseline to monitor topographic progression to keratoconus: Top A, round:
B, oval: C, superior steepening; D, inferior steepening; E,
irregular; F, symmetric bow tie; G, symmetric bow tie with
skewed radial axes; H, asymmetric bow tie with inferior
steepening (AB/IS); I, asymmetric bow tie with superior
steepening; J, asymmetric bow tie with skewed radial axes
(AB/SRAX). Lower two figures are a schematic illustration
of how to determine whether a pattern is AB/IS or AB/
SRAX. A line is drawn to bisect the upper and lower lobes
of the asymmetric bow tie (see solid lines), if there is no
significant deviation from the vertical meridian (i.e., no
skewing), the pattern is designated as AB/IS (as in bottom
A); if the lines bisecting the two lobes appear skewed by
more than 308 from the vertical meridian (i.e., 1508 from
one another), it is labeled as AB/SRAX (as in Bottom B).
(Reprinted from Rabinowitz et al108 with permission of the
British Journal of Ophthalmology.)
conus by videokeratography.99 Awareness of the
conditions that may simulate early keratoconus
videokeratographically will enhance the clinician’s
ability to recognize true topographic changes in early
keratoconus.
H. QUANTITATIVE DESCRIPTORS
Developing quantitative descriptors of videokeratography patterns in keratoconus would allow
for easier recognition of patterns and enable us to
develop a quantitative phenotype that could be
universally used to formulate minimal topographic
criteria for diagnosing keratoconus.111 In a small preliminary study, we developed three indices that dis-
311
KERATOCONUS
Fig. 12. Pseudokeratoconus error pattern (with Eysys instrument) induced from misalignment of a normal eye resulting
in a pattern simulating a keratoconus videokeratograph (right); videokeratograph of early keratoconus for comparison
(left). (Courtesy of R. E. Hubbe, MD, and Gary Foulks, MD.)
tinguished eyes with keratoconus from normals: central K (descriptive of central steepening); I-S values
(inferior-superior dioptric asymmetry); and R versus
L (difference between right and left central corneal
power). Videokeratography studies on 28 family
members of five patients with keratoconus revealed
that 50% of the subjects had mild topographic abnormalities and at least one index greater than two
standard deviations from their normal control
group. These abnormalities were similar to, but less
severe than, those found in the patients with keratoconus. It is possible that these indices are descriptive
of the earliest stages of keratoconus in normal eyes
before they progress to keratoconus, and these abnormalities might represent variable expression of a
keratoconus gene in these families.101,104 However,
longitudinal studies and serial topographic analysis
are required to confirm this. Since the original
study, the indices have been modified and embodied into a computer software program where they
are analyzed with our baseline database (constructed from 195 normals). A new index has also
been developed that is more specific to keratoconus
and that quantifies the irregular astigmatism that
typifies the keratoconus videokeratograph, the SRAX
index (Fig. 6). Using a combination of four indices,
Central K, I-S value, Sim K, and the SRAX index,
98% of keratoconus videokeratographs could be distinguished from a group of normal controls. These
indices were, however, useful only in patients with
1.5 D or more of astigmatism as measured by the
simulated keratometry readings.99 Work is currently
in progress to formulate a single numeric value derived from these indices to provide minimal topographic criteria for assigning affectation status to
keratoconus family members for use in formal pedigree analyses such as complex segregation analysis.109
Analyses of videokeratography data described thus
far are based on data generated by sagittal algorithms, which are spherically biased. Recent preliminary studies suggest that tangential algorithms may
have more promise for identifying the early topographic features of keratoconus. Studies are currently in progress to determine whether such algorithms might be the preferred method for studying
keratoconus.98
I. VIDEOKERATOGRAPHY SCREENING FOR
REFRACTIVE SURGERY
With the recent approval in the USA of the excimer laser for the correction of myopia, detecting
early keratoconus in the absence of slit-lamp findings has assumed increasing importance. In some instances, unpredictable results and patient dissatisfaction have been attributed to the existence of
undiagnosed early keratoconus in refractive surgery
patients.28,82 Because these patients do not achieve
high-quality vision with either glasses or contact lenses,
they tend to seek out refractive surgery. Recent reports
suggest that patients with early keratoconus or keratoconus suspects comprise 2–5% of patients presenting
for refractive surgery for myopia.88,154
Videokeratography screening allows the clinician
to rule out these early ectasias and other topographic abnormalities before embarking on refractive surgery. It is difficult to identify which subtle
keratoconuslike topographic patterns truly represent early keratoconus, hence the need to formulate
quantitative indices derived from patients who have
clinical signs of disease.
312
Surv Ophthalmol 42 (4) January–February 1998
Two software systems using quantitative indices
for detecting keratoconus are currently available on
some corneal topographers, the one developed by
Rabinowitz99 and another developed by Maeda and
Klyce at the LSU Eye Center in New Orleans, Louisiana.76,77 Using TMS-1 videokeratographs, the LSU
group computed 11 quantitative criteria for each
map and trained a three-layer neural network using
108 maps from 7 separate diagnostic categories. The
overall accuracy of the trained neural network was
80%. Based on eight of the quantitative criteria,
Maeda and Klyce designed an “expert system” to detect keratoconus. The system, which is based on linear discriminant analysis and a binary decision tree,
identifies the map as representing keratoconus or
nonkeratoconus and, based on a value from the discriminant analysis (the KPI), assigns the map an index expressed as a percentage that suggests the severity of keratoconus (the KCI, Fig. 15). This system
was able to differentiate keratoconus from a wide variety of other pathologies with a false positive rate of
1 out of 43 and a false negative rate of 2 in 130.
The Rabinowitz software differs from the Maeda/
Klyce system in several respects: it attempts only to
differentiate keratoconus from normals, not from
other pathologies in a noncontact lens wearing population; it relies on both eyes, not a single eye in its
evaluation; its indices are derived from videokeratographs only of patients who have clinical signs of
keratoconus, not from videokeratographs judged by
experts to have keratoconus without regard to clinical signs; and it provides clear quantitative cutoff
points based on its indices as to which videokeratographs should be labeled normal or keratoconus.99
Both software programs were designed to aid the
clinician in identifying abnormal topography and
were not intended as a substitute for a history, thorough ocular evaluation, and good clinical judgment
when a patient is being evaluated as a candidate for
refractive surgery.
VI. Differential Diagnosis
It is important to distinguish keratoconus from
other ectatic dystrophies and thinning disorders,
such as pellucid marginal degeneration, Terrien’s
marginal degeneration, and keratoglobus, because
the management and prognosis in these disorders
differ markedly from keratoconus. The distinction
can usually be made by careful slit-lamp evaluation,
but corneal topography evaluation is a useful adjunct to differentiate these disorders in subtle or
early cases.107
A. PELLUCID MARGINAL DEGENERATION
Pellucid marginal degeneration is characterized by
a peripheral band of thinning of the inferior cornea
RABINOWITZ
from the 4 to the 8 o’clock position. There is 1–2-mm
uninvolved area between the thinning and the limbus (Fig. 1B). The corneal protrusion is most marked
above the area of thinning, and the thickness of the
central cornea is usually normal. Like keratoconus,
pellucid marginal degeneration is a progressive disorder affecting both eyes, although eyes may be
asymmetrically affected. In moderate cases it can easily be differentiated from keratoconus by slit-lamp
evaluation because of the classical location of the
thinning. In early cases the cornea may look relatively normal, and in advanced cases it may be difficult to distinguish from keratoconus because the
thinning may involve most if not all of the inferior
cornea. In both instances videokeratography is very
useful to make the distinction. The videokeratograph
has a classical “butterfly” appearance (Fig. 13A), demonstrating large amounts of against-the-rule astigmatism, as measured by simulated keratometry.79
Pellucid marginal degeneration can be differentiated from other peripheral corneal thinning disorders, such as Terrien’s marginal degeneration, because the area of thinning is always epithelialized,
clear, avascular, and without lipid deposition. Terrien’s corneal degeneration affects a similar age
group and also causes high astigmatism; however, it
may affect both the superior and inferior cornea
and is accompanied by lipid deposition and vascular
invasion. Videokeratography can also be used to differentiate these two disorders because they have distinctly different topographic patterns.158
Because of the large amounts of against-the-rule
astigmatism, patients with pellucid marginal degeneration are much more difficult to fit with contact
lenses than patients with keratoconus, although spherical or aspheric contact lenses with large overall
diameter should initially be attempted in early-tomoderate cases. Surgery may be considered for patients whose vision is not adequately corrected by
contact lenses or in patients who are contact lensintolerant. Patients with pellucid marginal degeneration, however, are typically poor candidates for penetrating keratoplasty for two reasons. First, thinning
occurs so near the limbus that the donor cornea
must be placed very close to the corneal limbus, thus
increasing the chances of graft rejection. Second,
because of the extreme thinning and the location of
the thinning, penetrating keratoplasty typically induces large amounts of postoperative astigmatism,
which may be extremely difficult to correct because
of disparity in graft-host thickness.
Crescentic lamellar keratoplasty is a useful initial
surgical procedure in patients with pellucid marginal degeneration. This procedure involves removing a crescentic inferior layer of ectatic tissue by
lamellar dissection and replacing it with a thicker
313
KERATOCONUS
Fig. 13. Pellucid marginal degeneration: A: Videokeratograph with typical butterfly-shaped appearance. B:
Postoperative slit-lamp photo after
combined peripheral crescentic lamellar keratoplasty and central penetrating keratoplasty.
lamellar donor graft.124 This will, in most cases, eliminate large amounts of against-the-rule astigmatism.
In some cases, the patient may become contact lenstolerant, thus obviating a full-thickness procedure.
In contact lens failures, a full-thickness centrally located penetrating keratoplasty can subsequently be
performed, encompassing part of the lamellar graft
and significantly reducing the risk of graft rejection
and postkeratoplasty astigmatism (Fig. 13B).
ning centrally or paracentrally in keratoconus.22,48,66
The cornea may be thinned to as little as 20% of normal thickness, and it assumes a globular shape. In
advanced keratoconus, the entire cornea can also be
thinned and globular-shaped, making it difficult to
distinguish these two entities. However, even in very
advanced keratoconus there may be a small area of
uninvolved cornea superiorly that approaches normal corneal thickness.
Keratoglobus is bilateral, but it is usually present
from birth and tends to be nonprogressive. It can be
distinguished from megalocornea and congenital
glaucoma because the cornea is usually of normal diameter. It is a recessive disorder and is often associated with blue sclerae and other systemic features, in
contrast to keratoconus, which is most commonly an
isolated disorder.22,66,146 In contrast to keratoconus,
the corneas in keratoglobus are prone to corneal
rupture from even minimal trauma. Thus, hard contact lenses are contraindicated and protective spectacles should be strongly encouraged. If the cornea is
extremely thin, a tectonic limbus-to-limbus lamellar
keratoplasty should be considered to strengthen the
cornea. A subsequent central penetrating keratoplasty may be considered if adequate visual rehabilitation cannot be achieved with glasses.
VII. Management of Keratoconus
A. CONTACT LENSES
B. KERATOGLOBUS
Keratoglobus is a rare disorder in which the entire
cornea is thinned most markedly near the corneal
limbus (Fig. 1C), in contrast to the localized thin-
The management of keratoconus varies depending on the state of progression of the disease. In very
early cases, spectacles may provide adequate visual
correction, but because spectacles do not conform
to the unusual shape of the cornea and the resultant
314
Surv Ophthalmol 42 (4) January–February 1998
RABINOWITZ
Fig. 14. Correction of postkeratoplasty astigmatism in a patient with
keratoconus: A: Preoperative videokeratograph illustrating large degree
of astigmatism and stable topography
6 months apart. B: Diagram illustrating location of relaxing incisions and
compression sutures based on the
information gleaned from the videokeratograph. C: Postoperative videokeratograph 2 months after sutures
had been removed. (Reprinted from
Rabinowitz et al107 with permission of
Igaku Shoin Medical Publishers, Inc.)
induced irregular astigmatism, contact lenses provide better correction. Contact lenses are the mainstay of therapy in this disorder and represent the
treatment of choice in 90% of patients.17,18
The type of contact lens used varies depending on
the stage of keratoconus. Early in the disease, soft
lenses of toric design are adequate. As the disease
progresses, more complex rigid gas permeable lenses
are used; these include multicurve spherical-based
lenses, aspheric lenses, and biaspheric lenses. A hybrid lens, which has a rigid central portion for obtaining best optics and a soft hydrophilic peripheral
skirt, is also popular with some practitioners.100,119,161
Fitting contact lenses in keratoconus is a complex
task embraced by few contact lens practitioners. The
challenge is to keep the patient contact lens-tolerant
with good visual acuity in a cornea that may be
changing in shape over time. Common complications from lenses include induced corneal abrasion,
apical scarring, neovascularization from induced hypoxia, lens discomfort, and lenses not staying on the
cornea for adequate periods of time. While some reports suggest that rigid contact lenses induce keratoconus and anecdotal reports contend that keratoconus can be arrested by good contact lens fitting,
good evidence does not exist that supports either of
these contentions. With the new contact lenses currently available and with good fitting techniques,
many patients with 20/40 spectacle correction may
enjoy stable 20/20–20/25 contact lens correction
315
KERATOCONUS
Fig. 15. Keratoconus suspect videokeratograph (absolute scale, sagittal
topography) with Rabinowitz and
Klyce diagnostic indices to aid in interpretation of color-coded map.
for many years. I believe that no keratoconus patient
who can tolerate contact lenses should be denied
the good visual rehabilitation afforded by them because of fear that they may enhance the progression
of the disease.
B. CORNEAL TRANSPLANT
1. Indications
Corneal transplant (penetrating keratoplasty) is
the best and most successful surgical option for keratoconus patients who cannot tolerate contact lenses
or are not adequately visually rehabilitated by them.
Central scarring may preclude good vision from contact lenses, even when they are tolerated. A patient with
keratoconus has an approximately 10–20% chance
over his/her lifetime of needing a corneal transplant.132,145 Corneas in keratoconus almost never perforate; thus, advanced thinning by itself is not necessarily an indication for surgery.
Acute hydrops is not necessarily an indication for
penetrating keratoplasty, because in many instances
the hydrops resolves and the resultant scar is outside
the visual axis. The scarring may flatten the cornea,
allowing the patient to tolerate contact lenses and
achieve good vision. Patients with hydrops can be
treated initially with cycloplegics, steroids or nonsteroidal anti-inflammatory agents, 5% sodium chloride solution (Muro 128), and, in rare instances,
with bandage contact lenses.134
Buzard and Fundingsland have recently suggested
that because of improved corneal transplant techniques and new and improved modalities to correct
refractive error after corneal transplantation, patients whose best corrected spectacle visual acuity is
20/40 or worse should be offered cornea transplants
in lieu of contact lens fitting.19 Considering the good
visual acuity afforded to many patients who are successful contact lens wearers, this approach would be
regarded by many as being too aggressive.
2. Procedures and Success Rate
Because of the avascular nature of the cornea, corneal transplant has a success rate of 93–96%.97,130,144,152
Advances in both eyebanking and surgical techniques now allow this procedure to be done on an
outpatient basis with minimal incapacitation of the
patient. Complete visual recovery may, however, take
as long as 6 months.
Patients who are candidates for penetrating keratoplasty should be counseled that in spite of the high
success rate of surgery there is still a 50% chance that
they may need contact lenses, either because of residual myopia or postkeratoplasty astigmatism. To decrease the amount of myopia, several surgeons are performing keratoplasties with the donor and host
trephines of equal size (usually 7.5 mm; the incidence
of rejection is slightly higher with larger size
grafts).45,143,144 While in many instances this reduces the
amount of myopia, patients who are axial myopes may
still be left with large amounts of residual myopia.143
Large amounts of postkeratoplasty astigmatism may
remain even after all the sutures are removed. This
can be corrected with a combination of relaxing incisions and compression sutures while videokeratography is used as a guide. The residual astigmatism is
then small and and can be corrected well with rigid
gas permeable lenses (Fig. 14).107 It is desirable to
leave a small amount of with-the-rule astigmatism, as
the patients tolerate this better and it allows for easier
contact lens fitting than against-the-rule astigmatism.
316
Surv Ophthalmol 42 (4) January–February 1998
3. Complications
In compliant patients, complications after penetrating keratoplasty are rare. These may include rejection, postoperative astigmatism, a fixed dilated
pupil, and recurrence of keratoconus.1,67,89,142,149 Graft
rejection rates in keratoconus are low and may be reversed with medication if treated early. There have
been isolated reports of keratoconus recurring in
the graft decades after surgery. These reports are extremely rare, and it is not clear whether keratoconus
actually recurred in the graft or whether there was
mild, undetected keratoconus in the donor buttons.1,67,89 Patients will, however, often ask about recurrence, and these isolated reports should be mentioned within this context.
C. EPIKERATOPLASTY
Epikeratoplasty for a while gained acceptance as a
mode of treatment for patients with keratoconus
with a clear visual axis. Although good long-term results have been reported,70,148 the procedure has for
the most part been abandoned in favor of penetrating keratoplasty because of the superior quality of vision afforded by the latter procedure. There still is a
role for epikeratoplasty in select high-risk circumstances. For instance, in keratoconus patients with
Down syndrome, epikeratoplasty might be preferable to a penetrating keratoplasty because of its noninvasive nature and the decreased potential for corneal graft rejection.
D. EXCIMER LASER
PHOTOTHERAPEUTIC KERATECTOMY
Excimer laser phototherapeutic keratectomy has
been demonstrated to be useful in the management
of patients with keratoconus who have nodular subepithelial corneal scars and who are contact lensintolerant.150 This technique provides a smooth corneal surface, allowing patients to regain contact lens
tolerance. The nodules may also be removed at the
slit-lamp with a sharp handheld blade, potentially
with a similar result, albeit with less precision. A recent small study, with short-term data only, suggests
that the excimer laser might be useful for providing
an improved refractive effect and delaying the need
for penetrating keratoplasty in patients with advanced keratoconus.85 This suggested mode of treatment for keratoconus is not currently commonly accepted and should be approached with extreme
caution until long-term data on outcomes become
available. Performing this procedure on an already
thinned and irregular cornea could be hazardous
and has the potential for immediate complications
exceeding the long-term therapeutic effect.
RABINOWITZ
Method of Literature Search
All articles in Medline up to March 1997 were reviewed. Those considered relevant and that contributed scientifically to the topics covered were included
in this article.
References
1. Abelson MB, Collin HB, Gillete TE, Dohlman CH: Recurrent
keratoconus after keratoplasty. Am J Ophthalmol 90:672–676,
1980
2. Alstrom CH, Olson O: Heredo-retinopathia congenitalis.
Monohybride recessiva autosomalis. Hereditas Genttiskt
43:1–177, 1957
3. Amsler M: Le keratocone fruste au javal. Ophthalmologica
96:77–83, 1938
4. Amsler M: Keratocone classique et keratocone fruste, arguments unitaires. Ophthalmologica 111:96–101, 1946
5. Archer DB, Sharma NK: Irido-corneal dysgenesis. Trans
Ophthalmol Soc UK 98:510, 1978
6. Austin MG, Schaefer RF: Marfan’s syndrome with unusual
blood vessel manifestations. Arch Pathol 64:204–209, 1957
7. Beardsley TL, Foulks GN: An association of keratoconus and
mitral valve prolapse. Ophthalmology 89:35–37, 1982
8. Beckh U, Schonherr U, Naumann GO: Augenklinik mit Poliklinik, Universitat Erlangen-Nurnberg. Autosomal dominant keratoconus as the chief ocular symptom in Lobstein
osteogesis imperfecta tarda. Klin Monatsbl Augenheilkd
206:268–272, 1995
9. Bereau J, Fabre EJ, Hecquet C, et al: Modification of prostaglandin E2 and collagen synthesis in keratoconus fibroblasts associated with an increase of interleukin-1 alpha receptor number. CR Acad Sci, Paris 316(III):425–430, 1993
10. Bisaria KK: Bilateral keratoconus with ocular hypertension
and the natural cure of one eye. J All India Ophthalmol Soc
15:197–199, 1967
11. Blair SD, Seabrooks D, Shields JW, et al: Bilateral progressive essential iris atrophy and keratoconus with coincident
features of posterior polymorphous dystrophy: a case report
and proposed pathogenesis. Cornea 11:255–261, 1992
12. Blanksma LJ, Donders PC, Van Voorst Vander PC: Xeroderma Pigmentosum and keratoconus. Doc Ophthalmol
64:97–103, 1986
13. Brenner S, Nemet P, Legum C: Jadasohn-type anetoderma
in association with keratoconus and cataract. Ophthalmologica 174:181–184, 1977
14. Bron A, Rabinowitz YS: Corneal dystrophies and keratoconus. Curr Opin Ophthalmol 7:71–82, 1996
15. Brown IA: Ankyloblepharon associated with keratoconus. Br
J Ophthalmol 51:138–139, 1967
16. Buiuc S, Beschea G, Jaobleceastai L, Dimitriu G: A case of bilateral posterior lenticonus associated with keratoconus. Rev
Chir Oftalmol 22:299–300, 1978
17. Buxton JN: Contact lenses in keratoconus. Contact Intraocular Lens Med J 4:74, 1978
18. Buxton JN, Keates RH, Hoefle FB: The contact lens correction of keratoconus, in Diabezes OH (ed): Contact Lenses.
The CLAO Guide to Basic Science and Clinical Practice. Orlando, Grune and Stratton, 1984
19. Buzard KA, Fundingsland BR: Cornea transplants for keratoconus. Results in early and late disease. J Refract Surg
23:398–496, 1997
20. Byers PH: Disorders of collagen biosynthesis and structure,
in Scriver CR, Beaudet AL, Sly WS, Valle D (eds): Metabolic
Basis of Inherited Disease. New York, McGraw Hill, 1995, ed
7, pp 4029–4077
21. Cantor RM, Rotter JI: Analysis of genetic data: methods and
interpretation, in King RA, Rotter JI, Motulsky AG (eds):
The Genetic Basis of Common Diseases. 1992, pp 49–70
22. Cavara V: Keratoglobus and keratoconus. Br J Ophthalmol
34:621, 1950
317
KERATOCONUS
23. Conneally PM, Rivas ML: Linkage analysis in man. Adv Hum
Genet 10:209–266, 1980
24. Cullen JF, Butler HG: Mongolism (Down’s Syndrome) and
keratoconus. Br J Ophthalmol 47:321–330, 1963
25. Donaldson DD: A new instrument for keratography. Arch
Ophthalmol 88:425–428, 1972
26. Driver PJ, Reed JW, David RM: Familial cases of keratoconus
associated with posterior polymorphous dystrophy (letter).
Am J Ophthalmol 118:256–257, 1994
27. Duke-Elder S, Leigh AG: System of ophthalmology. Diseases
of the outer eye, Vol 8. London, Henry Kimpton, 1965, pp
964–976
28. Durand L, Monot JP, Burillon C, Assi A: Radial keratotomy
in a patient with keratoconus. Refract Corneal Surg 7:374–
376, 1991
29. Eiferman RA, Law MW, Lane L: Iridoschisis and keratoconus. Cornea 13:78–79, 1994
30. Elder MJ: Leber congenital amaurosis and its association
with keratoconus and keratoglobus. J Pediatr Ophthalmol
Strabismus 31:38–40, 1994
31. Elston RC: Segregation analysis. Adv Hum Genet 11:63–120,
1981
32. Enoch E, Itzahki A, Lakshminarayanan V, et al: Visual field
defects detected in patients with Gilles de la Tourette syndrome: preliminary report. Int Ophthalmol 13:331–344,
1989
33. Etzine S: Conical cornea in identical twins. S Afr Med J
28:154–155, 1954
34. Falls HF, Allen W: Dominantly inherited keratoconus. Report of a family. J Genet Hum 17:317, 1969
35. Franceschetti A: Keratoconus, in King JH, McTigue JW
(eds): The Cornea. World Congress. Washington, Butterworths, 1965, pp 152–168
36. Francois J: Afflictions of the cornea, in Francois J (ed): Heredity in Ophthalmology. St Louis, CV Mosby, 297–298,
1961
37. Francois J, Neetens A, Smets RM: Bardet-Biedl syndrome
and keratoconus. Bull Soc Ophthalmol 203:117–121, 1982
38. Frasca G, Belmonte M: Neurocutaneous angiomatosis and
keratoconus. A new syndrome entity? Riv Otoneurooftalmol
41:119–130, 1966
39. Freedman J, Gombos GM: Bilateral macular coloboma,
keratoconus and retinitis pigmentosa. Ann Ophthalmol
3:664–665, 1971
40. Filip O, Golu T, Filip I, et al: Keratoconus in Albers-Schonberg disease. Oftalmologia 38:247–251, 1994
41. Fukuchi T, Yue B, Sugar J, Lam S: Lysosomal enzyme activities in conjunctival tissues of patients with keratoconus.
Arch Ophthalmol 112:1368–1374, 1994
42. Gasset AR, Houde WI, Garcia-Bengochea H: Contact lens
wear as an environmental risk in keratoconus. Am J Ophthalmol 85:339–341, 1978
43. Gasset AR, Worthen DM: Keratoconus and Chandler’s syndrome. Ann Ophthalmol 6:819–820, 1974
44. Geerarts WJ: Ocular Syndromes. Philadelphia, Lea and Febiger, 1969, ed 2
45. Girard LJ, Esnaola N, Rao R, et al: Use of grafts smaller than
the opening for keratoconic myopia and astigmatism. J Cataract Refract Surg 18:380–384, 1992
46. Gonzalez V, McDonnell PJ: Computer-assisted corneal topography of parents in patients with keratoconus. Arch
Ophthalmol 110:1413–1414, 1992
47. Gormley DJ, Gersten M, Koplin RS, Lubkin V: Corneal modeling. Cornea 7:30, 1988
48. Grayson M, Keates RH: Manual of diseases of the cornea.
Boston, Little Brown, 1969, ed 1
49. Greenfield G, Romano A, Stein R, Goodman RM: Blue
sclerae and keratoconus. Key features of a distinct heritable
disorder of connective tissue. Clin Genet 4:8–16, 1973
50. Hallerman W, Wilson EJ: Genetische betrachtungen uber den
keratoconus. Klin Monatsbl Augenheilkd 170:906–908, 1977
51. Hammerstien W: Zur genetik des keratoconus. Graefes Arch
Klin Exp Ophthalmol 190:293–308, 1974
52. Hannush SB, Crawford SL, Waring GO III, et al: Accuracy
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
63.
64.
65.
66.
67.
68.
69.
70.
71.
72.
73.
74.
75.
76.
77.
and precision of keratometry, photokeratoscopy, and corneal modeling on calibrated steel balls. Arch Ophthalmol
107:1235–1239, 1989
Hartstien J: Keratoconus that developed in patients wearing
corneal contact lenses. Arch Ophthalmol 80:345–346, 1968
Hoang-Xuan T, Elmaleh C, Dhermy P, et al: Association of a
lattice dystrophy and keratoconus: anatomo-clinical study
apropos of a case. Bull Soc Ophthalmol Fr 89:35–38, 1989
Hofstetter H: A keratoscopic survey of 13,395 eyes. Am J Optom Acad Optom 36:3–11, 1959
Ihalainen A: Clinical and epidemiological features of keratoconus: genetic and external factors in the pathogenesis of
the disease. Acta Ophthalmol 178(Suppl):5–64, 1986
Iwaszkiewicz E: Keratoconus. II. Coexisting diseases and theories on its etiology and pathogenesis. Klin Oczna 91:210–
211, 1989
Judisch GF, Waziri M, Krachmer J: Ocular Ehlers-Danlos
syndrome with normal lysyl hydroxylase activity. Arch Ophthalmol 94:1489, 1976
Kayazawa F, Nishimura K, Kodama Y, et al: Keratoconus with
pellucid marginal corneal degeneration. Arch Ophthalmol
102:895–896, 1984
Kennedy RH, Bourne WM, Dyer JA: A 48-year clinical and
epidemiologic study of keratoconus. Am J Ophthalmol
101:267–273, 1986
Kenney MC, Chwa M, Opbroek AJ, et al: Increased gelatinolytic activity in keratoconus keratocyte cultures. A correlation to an altered matrix metalloproteinase-2/tissue inhibitor of metaloproteinase ratio. Cornea 13:108–113, 1994
Kirkham TH, Werner EB: The ophthalmic manifestations of
Rothmund’s syndrome. Can J Ophthalmol 10:1–14, 1975
Klintworth GK: Degenerations, depositions and miscellaneous reactions of the ocular anterior segment, in Garner A,
Klintworth GK (eds): Pathobiology of Ocular Disease: A Dynamic Approach. New York, Marcel Dekker, 1994, ed 2, pp
743–794
Klintworth GK, Damms T: Corneal dystrophies and keratoconus. Curr Opin Ophthalmol 6:44–56, 1995
Klyce SD: Computer-assisted corneal topography. High resolution graphic presentation and analysis of keratoscopy. Invest Ophthalmol Vis Sci 25:1426–1435, 1984
Krachmer JH, Feder RS, Belin MW: Keratoconus and related noninflammatory corneal thinning disorders. Surv
Ophthalmol 28:293–322, 1984
Kremer I, Eagle RC, Rapuano CJ, Laibson PR: Histologic evidence of recurrent keratoconus seven years after keratoplasty. Am J Ophthalmol 119:511–512, 1995
Kremer I, Martini AM, Cohen EJ: Keratoconus associated
with ectodermal and mesodermal anomalies (letter). CLAO
J 18:141, 1992
Kumig BS, Joffe L: Ehlers-Danlos syndrome associated with
keratoconus. S Afr Med J 52:403–405, 1977
Lass JH, Stocker EG, Fritz ME, Collie DM: Epikeratoplasty.
The surgical correction of aphakia, myopia, and keratoconus. Ophthalmology 94:912–925, 1987
Lee LR, Hirst LW, Readshaw G: Clinical detection of unilateral keratoconus. Aust N Z J Ophthalmol 23:129–133, 1995
Levene JR: An evaluation of the handheld keratoscope as a
diagnostic instrument for corneal astigmatism. Br J Physiol
Opt 19:237–251, 1962
Lipman RM, Rubenstein JB, Torczynski E: Keratoconus and
Fuchs’ corneal endothelial dystrophy in a patient and her
family. Arch Ophthalmol 108:993–994, 1990
Lorfel RS, Sugar HS: Keratoconus associated with retrolental fibroplasia. Ann Ophthalmol 8:449–450, 1976
Lund AM: The Angelman syndrome. Does the phenotype
depend on maternal inheritance? Ugeskr Laeger 153:1993–
1998, 1991
Maeda N, Klyce SD, Smolek MK, Thompson HW: Automated keratoconus screening with corneal topography analysis. Invest Ophthalmol Vis Sci 35:2749–2757, 1994
Maeda N, Klyce SD, Smolek MK: Comparison of methods
for detecting keratoconus using videokeratography. Arch
Ophthalmol 113:870–874, 1995.
318
Surv Ophthalmol 42 (4) January–February 1998
78. Maguire LJ, Bourne W: Corneal topography of early keratoconus. Am J Opthalmol 108:107–112, 1989
79. Maguire LJ, Klyce SD, McDonald ME, Kaufmann HE: Corneal topography of pellucid marginal degeneration. Ophthalmology 94:519–524, 1987
80. Maguire LJ, Meyer RF: Ectatic corneal degenerations, in
Kaufman H (ed): The Cornea. 1988, pp 485–510
81. Maguire LJ, Wilson SE, Camp JJ, Verity S: Evaluating the reproducibility of topography systems on spherical surfaces.
Arch Ophthalmol 111:259–262, 1993
82. Mammilis N, Montgomery S, Anderson C, et al: Radial keratotomy in a patient with keratoconus. Refract Corneal Surg
7:374–376, 1991
83. McKusick VA: Heritable Diseases of Connective Tissue. St
Louis, CV Mosby, 1966, ed 3
84. McKusick VA: Inherited disorders of connective tissue, in
Harrison TR (ed): Principles of Internal Medicine. New
York, McGraw Hill, 1974, ed 7, pp 2015–2020
84a. Merlin U, Cantera E: Corneal topography, in Burrato L
(ed): The Clinical Atlas thoroughfare, New Jersey, Slack,
1996, pp 9–93
85. Mortensen J, Ohrstrom A: Excimer laser photorefractive
keratectomy for treatment of keratoconus. J Refract Corneal
Surg 10:368–372, 1994
86. Morton NE: Segregation analysis, in Computer Applications
in Genetics, Honolulu, University of Hawaii Press, 1969, pp
129–139
87. Negris R: Floppy eyelid syndrome associated with keratoconus. J Am Optom Assoc 63:316–319, 1992
88. Nesburn AB, Bahri S, Salz J, et al: Keratoconus detected by
videokeratography in candidates for photorefractive keratectomy. J Refract Surg 11:194–201, 1995
89. Nirankari VS, Karesh J, Bastion F, et al: Recurrence of keratoconus in a donor cornea 22 years after successful keratoplasty. Br J Ophthalmol 67:32, 1983
90. Nucci P, Brancato R: Keratoconus and congenital hip dysplasia (letter). Am J Ophthalmol 111:775–776, 1991
91. Nucci P, Trabucchi G, Brancato R: Keratoconus and
Turner’s syndrome: a case report. Optom Vis Sci 68:407–
408, 1991
92. Opbroek A, Kenney MC, Brown D: Characterization of a human corneal metalloproteinase inhibitor (TIMP-1). Curr
Eye Res 12:877–883, 1993
93. Parker J, Ko W, Pavlopoulos G, et al: Videokeratography of
keratoconus in monozygotic twins. J Refract Surg 12:180–
183, 1996
94. Peduzzi MD, Torlai F, Delvecchio G: Bilateral pigmented retinopathy following measles: long term follow up and possible association with keratoconus. Eur J Ophthalmol 1:148–
150, 1991
95. Perlman JM, Zaidman GW: Bilateral keratoconus in Crouzon’s syndrome. Cornea 13:80–81, 1994
96. Perry HD, Buxton JN, Fine BS: Round and oval cones in
keratoconus. Ophthalmology 87:905–909, 1980
97. Price FW, Whitson WE, Marks RG: Graft survival in four
common groups of patients undergoing penetrating keratoplasty. Ophthalmology 98:322–328, 1991
98. Rabinowitz YS: Tangential vs sagittal videokeratographs in
the “early” detection of keratoconus. Am J Ophthalmol
122:888–889, 1996
99. Rabinowitz YS: Videokeratographic indices to aid in screening for keratoconus. J Refract Surg 11:371–379, 1995
100. Rabinowitz YS, Garbus JJ, Garbus C, McDonnell PJ: Contact
lens selection for keratoconus using a computer-assisted
videophotokeratoscope. CLAO J 17:88–93, 1991
101. Rabinowitz YS, Garbus J, McDonnell PJ: Computer-assisted
corneal topography in family members of keratoconus. Arch
Ophthalmol 108:365–371, 1990
102. Rabinowitz YS, Klyce SD, Krachmer JH, et al: Videokeratography, keratoconus, and refractive surgery. Opinions. Refract Corneal Surg 5:403–407, 1992
103. Rabinowitz YS, McDonnell PJ: Computer-assisted corneal topography in keratoconus. Refract Corneal Surg 5:400–406,
1989
RABINOWITZ
104. Rabinowitz YS, Maumenee IH, Lundergan MK, et al: Molecular genetic analysis in autosomal dominant keratoconus.
Cornea 11:302–308, 1992
105. Rabinowitz YS, Nesburn AB, McDonnell PJ: Videokeratography of the fellow eye in unilateral keratoconus. Ophthalmology 100:181–186, 1993
106. Rabinowitz YS, Riley C, Yang H, et al: Videokeratography
studies of keratoconus parents (abstract). Invest Ophthalmol Vis Sci 36 (Suppl):S308, 1995
107. Rabinowitz YS, Wilson SE, Klyce SD (eds): Corneal Topography: Interpreting Videokeratography. New York, Tokyo, Igaku Shoin, 1993
108. Rabinowitz YS, Yang H, Akkina J, et al: Videokeratography
of normal human corneas. Br J Ophthalmol 80:610–616,
1996
109. Rabinowitz YS, Yang H, Elashoff J, Rotter J: The KI-SA% index: a quantitative new videokeratography algorithm embodying minimal topographic criteria for diagnosing keratoconus and “suspects” (abstract). Invest Ophthalmol Vis Sci
37 (Suppl):S910, 1996
110. Rabinowitz YS, Yang H, Elashoff J, Rotter J: Familiality in
keratoconus and related topographic measures. Proceedings of the World Congress of the Cornea IV (Abstract). Abstract Book. VIII Keratoconus, 1996, p 2
111. Rabinowitz YS, Yang H, Elashoff J, Rotter J: Videokeratography indicators of “early” keratoconus (abstract). Invest Ophthalmol Vis Sci 34 (Suppl):S1218, 1993
112. Rabinowitz YS, Yang H, Elashoff J, Rotter J: Videokeratography and pachymetry studies in keratoconus (abstract). Ophthalmology (Suppl):67, 1993
113. Rahi A, Davies P, Ruben M, et al: Keratoconus and coexisting atopic disease. Br J Ophthalmol 61:761, 1977
114. Rau S, Duncker GI: Keratoconus in Mulvihill-Smith syndrome. Klin Monatsbl Augenheilkd 205:44–46, 1994
115. Redmond KB: The role of heredity in keratoconus. Trans
Ophthalmol Soc 27:52–54, 1968
116. Ricci B, Lepore D, Iossa M, et al: Ocular anomalies in
Alagille’s syndrome (Anomalies oculaires dans le syndrome
d’Alagille). J Fr Ophthalmol 14:481–485, 1991
117. Robertson I: Keratoconus and Ehlers Danlos syndrome. A
new aspect of keratoconus. Med J Aust 1:571–573, 1975
118. Rose NJ, Mackay K, Byers PH, Dalgleish R: A Gly238Ser substitution in the alpha 2 chain of type I collagen results in osteogenesis imperfecta type III. Hum Genet 95:215–218, 1995
119. Rosenthal P, Cotter JM, Clinical performance of a splinebased apical vaulting keratoconus corneal contact lens design. CLAO J 21:42–46, 1995
120. Rowsey JJ, Reynolds AE, Brown R: Corneal topography. Corneascope. Arch Ophthalmol 99:1093–1100, 1981
121. Sassani JW, Smith SG, Rabinowitz YS: Keratoconus and bilateral lattice-granular corneal dystrophies. Cornea 11:343–
350, 1992
122. Sawagamuchi S, Twinning SS, Yue BY, et al: Alpha 2 macroglobulin levels in normal human and keratoconus corneas.
Invest Ophthalmol Vis Sci 35:4008–4014, 1994
123. Sawagamuchi S, Yue BYT, Sugar J, Giljoy JE: Lysosomal abnormalities in keratoconus. Arch Ophthalmol 107:1507–
1510, 1989
124. Schanzlin DJ, Samo EM, Robin JB: Crescentic lamellar
keratoplasty in pellucid marginal degeneration. Am J Ophthalmol 96:253, 1983
125. Schwartz DE: Noonan’s syndrome associated with ocular abnormalities. Am J Ophthalmol 73:955–960, 1972
126. Sczhotka L, Rabinowitz YS, Yang H: The influence of contact lens wear on the topography of keratoconus. CLAO J
22:270–273, 1996
127. Shammas HJ, McGaughey AS: Retinal disinsertion syndrome: report of a case. J Pediatr Ophthalmol Strabismus
16:284–286, 1979
128. Shapiro MB, France T: The ocular features of Down’s syndrome. Am J Ophthalmol 99:659, 1985
129. Sharif KW, Casey TA, Colart J: Prevalence of mitral valve
prolapse in keratoconus patients. J R Soc Med 85:446–448,
1992
319
KERATOCONUS
130. Sharif KW, Casey TA: Penetrating keratoplasty for keratoconus: complications and long term success. Br J Ophthalmol
75:142–146, 1991
131. Shows TB, Sakaguchi AY, Naylor SL: Mapping the human
genome, cloned genes, DNA polymorphisms, and inherited
disease. Adv Hum Genet 12:341–468, 1982
132. Smiddy WE, Hamburg TR, Kracher GP, Stark WJ: Keratoconus. Contact lens or keratoplasty? Ophthalmology 95:487–
492, 1988
133. Smith VA, Hoh VB, Littleton L, Easty DL: Overexpression of
gelatinase A activity in keratoconus. Eye 9:429–433, 1995
134. Smolin G: Dystrophies and degenerations, in Smolin G,
Thoft RA (eds): The Cornea: Scientific Foundations and
Clinical Practice, Boston, Little, Brown, 1987, ed 2, pp 448–449
135. Stokes DW, Parrish CM: Axenfeld’s anomaly associated with
Down’s syndrome. Cornea 11:163–164, 1992
136. Stone DL, Kenyon KR, Stark WJ: Ultrastructure of keratoconus with healed hydrops. Am J Ophthalmol 82:450–458, 1976
137. Street DA, Vinokur ET, Waring GO III, et al: Lack of association between keratoconus, mitral valve prolapse and joint
hypermobility. Ophthalmology 98:170–176, 1991
138. Thalasselis A, Selim AA: Keratoconus-tetany-menopause: the
new association. Optom Vis Sci 68:357–363, 1991
139. Thompson JS, Thompson MW: Twins in medical genetics in
genetics in medicine. Philadelphia, WB Saunders, 1986
140. Tiller G, Cohn D, Rabinowitz YS: Linkage analysis in familial
keratoconus (abstract). Invest Ophthalmol Vis Sci 33
(Suppl):S793, 1992
141. Tretter T, Rabinowitz YS, Yang H, et al: Aetiological factors
in keratoconus. Ophthalmology 102 (Suppl):156, 1995
142. Tuft SJ, Buckley RJ: Iris ischaemia following penetrating
keratoplasty for keratoconus (Urets-Zavalia syndrome). Cornea 14:618–622, 1995
143. Tuft SJ, Fitzke FW, Buckley RJ: Myopia following penetrating keratoplasty for keratoconus. Br J Ophthalmol 76:642–
645, 1992
144. Tuft SJ, Gregory WM, Davidson CR: Bilateral penetrating
keratoplasty for keratoconus. Ophthalmology 102:462–468,
1995
145. Tuft SJ, Moodaley LC, Gregory WM, et al: Prognostic factors
of progression to keratoconus. Ophthalmology 101:439–
447, 1994
146. Verrey F: Keratoglobe aigu. Ophthalmologica 114:284, 1947
147. Wachmeister L, Ingemannsson SO, Moller E: Atopy and
HLA antigens in patients with keratoconus. Acta Ophthalmol (Copenh) 60:113, 1982
148. Waller SG, Steinert RF, Wagoner MD: Long-term results of
epikeratoplasty for keratoconus. Cornea 14:84–88, 1995
149. Walsh FB, Hoyt WF: Clinical neuro-ophthalmology. Baltimore, Williams and Wilkins, 1969, ed 3
150. Ward MA, Artunduaga G, Thompson KP, et al: Phototherapeutic keratectomy for the treatment of nodular subepithelial corneal scars in patients with keratoconus who are contact lens intolerant. CLAO J 21:130–132, 1995
151. Waring GO, Rabinowitz YS, Sugar J, et al: Nomenclature for
keratoconus suspects. Refract Corneal Surg 9:219–221, 1993
152. Williams KA, Muehlberg SM, Lewis RF, Coster DJ: How successful is corneal transplantation? A report from the Australian Corneal Graft Register. Eye 9:219–227, 1995
153. Wilson SE, He YG, Weng J, et al: Epithelial injury induces
keratocyte apoptosis: Hypothesized role for the interleukin
1 system in the modulation of corneal tissue organization
and wound healing. Exp Eye Res 62:325–337, 1996
154. Wilson SE, Klyce SD: Screening for corneal topographic abnormalities before refractive surgery. Ophthalmology
101:147–152, 1994
155. Wilson SE, Klyce SD, Husseini MD: Standardized color
coded maps for corneal topography. Ophthalmology
100:1723–1727, 1993
156. Wilson SE, Lin DTC, Klyce SD: The topography of keratoconus. Cornea 10:2–8, 1991
157. Wilson SE, Lin DTC, Klyce SD, et al: Topographic changes
in contact lens-induced corneal warpage. Ophthalmology
97:734–744, 1990
158. Wilson SE, Lin DTC, Klyce SD, Insler MS: The corneal topography of Terrien’s marginal degeneration. Refract Corneal Surg 6:15–20, 1990
159. Wilson SE, Verity SM, Conger DL: Accuracy and reproducibility of the corneal analysis system and topographic modeling system. Cornea 11:28–35, 1992
160. Wolter JR: Bilateral keratoconus in Crouzon’s syndrome
with unilateral acute hydrops. J Pediatr Ophthalmol 14:141–
143, 1977
161. Yeung K, Egbahli F, Weissman BA: Clinical experience with
piggyback contact lens systems on keratoconic eyes. J Am
Optom Assoc 66:539–543, 1995
162. Zala L, Ettlin C, Krebs A: Fokale dermal Hypoplasie mit
Keratokonus. Osophaguspappillomen und Hidrokystomen.
Dermatologica 150:176–185, 1975
163. Zimmerman DL, Fischer RW, Winterhalter KH, et al: Comparitive studies of collagens in normal and keratoconus corneas. Exp Eye Res 46:431–442, 1988
164. Zolog N: On congenital blindness (Kurz syndroms) (Observations sur la cecite congenitale [Syndrome de Kurz]). Bull
Mem Soc Fr Ophthalmol 82:113–116, 1969
Outline
Epidemiology
Clinical features
Histopathology
Etiology and pathogenesis
A. Associated disorders
B. Biochemical studies
C. Genetics
1. Twin studies
2. Family studies
3. Formal genetic analyses
a. Molecular genetic studies
b. Collagen genes as candidate genes
4. Summary
V. Topographic studies of keratoconus
A. Placido disk studies
B. Photokeratoscopy
C. Keratometry
D. Computer-assisted videokeratoscopy
E. Videokeratography studies of keratoconus
F. Videokeratography pattern recognition: normals
versus keratoconus
G. Videokeratographic “pseudokeratoconus”
H. Quantitative descriptors
I. Videokeratography screening for refractive surgery
VI. Differential diagnosis
A. Pellucid marginal degeneration
B. Keratoglobus
VII. Management of keratoconus
A. Contact lenses
B. Corneal transplant
1. Indications
2. Procedures and success rate
3. Complications
C. Epikeratoplasty
D. Excimer laser phototherapeutic keratectomy
I.
II.
III.
IV.
Supported in part by a grant from the National Institutes of Health
NEI R01-09052 and the Eye Birth Defects Research Foundation, Inc.
Reprint address: Yaron S. Rabinowitz, MD, 444 South San Vicente
Boulevard, #1102, Los Angeles, CA 90048. E-Mail: rabinowitzy@
csmc.edu. Internet address: www.laser-prk.com