Baylor Pressure Ulcer Prevention Guideline
advertisement

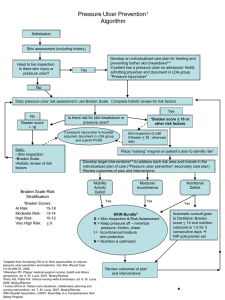
Attachment A3 - BHCS Pressure Ulcer Prevention and Intervention Guideline Standard of Care: Bony Prominences Do not massage bony prominences Avoid positioning directly on the trochanter by using a 30 degree side-lying position Do not use donut shaped foam/pillow to offload pressure points, this increases pressure Heels Float heals off the end of a longitudinally placed pillow(s) or heel offloading device Heel pads are not an adequate way to off load heels Avoid use of rolled towels for offloading heel Incontinence Use incontinence pads ONLY if patient is incontinent Remove adult brief when patient is in bed Recommendations can be reconsidered if contraindicated by patient condition and/or goals of care (Cutaneous and cognitive perception of sensory stimuli) Degree to which patient is able to respond meaningfully to pressure related discomfort or pain Sensory Perception Braden & Braden Q Subscale Rating Score for Braden & Braden Q Subscale with Interventions o 4. No Impairment - no deficits in the ability to feel and voice pain o 3. Slightly Limited – responds to verbal commands, but may not have the ability to communicate: sensation in one or two extremities, discomfort, pain, or turning o o Provide routine skin care ___________________________________________________________________________________________________________________________________ needs Teach patient/family the importance of changing positions for prevention of pressure ulcers Encourage and assist small frequent position changes. (minimum every 2 hours) Off load pressure areas, heels and contracted joints Keep HOB at or below 30 degrees Protect skin from tubes such as NG, nasal cannula, orthopedic and positioning devices, and reposition if needed. Specialty support surface Develop pressure-relief schedule ___________________________________________________________________________________________________________________________________ 2. Very limited – responds only to painful stimuli or sensory impairment to approximately half the body (unable to verbally communicate pain or feel pain/discomfort). Provide interventions listed above as appropriate ___________________________________________________________________________________________________________________________________ 1. Completely Limited – unresponsive (decreased LOC or sedated) to painful stimuli or limited ability to feel pain or discomfort over most of the body (does not moan, flinch, or grasp) Provide select interventions listed above as appropriate ___________________________________________________________________________________________________________________________________ Page 1 of 6 Degree to which skin is exposed to moisture Moisture Attachment A3 - BHCS Pressure Ulcer Prevention and Intervention Guideline o 4. Rarely Moist – skin is usually dry, linen only requires changing at routine intervals o 3. Occasionally Moist – skin is occasionally moist, requiring an extra linen change approximately once a day o o Degree of physical activity Provide interventions listed above Cause of moisture addressed Incontinence pad Adult brief (use when up in chair or walking) remove when patient in bed Use of skin care products twice daily and after each incontinent episode Care to skin folds ___________________________________________________________________________________________________________________________________ 2. Very Moist – skin is often but not always moist. Linen must be changed at least once a shift Provide interventions listed above as appropriate ___________________________________________________________________________________________________________________________________ 1. Constantly Moist – skin is kept moist almost constantly by perspiration, urine, etc. Dampness is detected every time patient is moved or turned Activity Instruct patient and family to request care as needed Assess and provide appropriate skin care as needed to keep skin clean, avoid the use of incontinent pads under patient Moisturize as appropriate to maintain skin integrity ___________________________________________________________________________________________________________________________________ Provide interventions listed above as appropriate Fecal/urinary incontinence containment device ___________________________________________________________________________________________________________________________________ o 4. Walks Frequently - walks outside the room at least twice a day and inside the room at least once every two hours during waking hours. o 3. Walks Occasionally - walks occasionally during day but very short distances, with or without assistance. Spends majority of each shift in bed or chair. o o Encourage activity as tolerated ___________________________________________________________________________________________________________________________________ Provide interventions listed above, as appropriate Teach patient/family the importance of changing positions for prevention of pressure ulcers Chair cushion ___________________________________________________________________________________________________________________________________ 2. Chairfast - ability to walk severely limited or nonexistent. Cannot bear own weight and/or must be assisted into chair or wheel chair Provide interventions listed above as appropriate Assist with small frequent position changes (minimum every 2 hours) Select a position that minimizes pressure and shear Place feet on footstool or footrest if feet do not reach the floor Limit chair time to 1-2 hour intervals Specialty support surface Develop pressure-relief schedule ___________________________________________________________________________________________________________________________________ 1. Bedfast- confined to bed Provide interventions listed above as appropriate ___________________________________________________________________________________________________________________________________ Page 2 of 6 Ability to change and control body position Mobility Attachment A3 - BHCS Pressure Ulcer Prevention and Intervention Guideline o 4. No Limitation – makes major and frequent changes in position without assistance o 3. Slightly Limited – makes frequent though slight changes in body or extremity position independently o o Usual food intake pattern Provide interventions listed above as appropriate Teach patient/family the importance of changing positions for prevention of pressure ulcers Encourage and assist small frequent position changes (minimum every 2 hours) Chair - assist with small frequent position changes (minimum every 2 hours) Elevate heels off bed Foam wedges to maintain position HOB at or below 30 degrees Assistive devices Perform ROM Specialty support surface Develop pressure-relief schedule ________________________________________________________________________________________________________ 2. Very Limited – makes occasional slight changes in body or extremity position but unable to make frequent or significant changes independently Provide interventions listed above as appropriate ________________________________________________________________________________________________________ 1. Completely Immobile – does not make even slight changes in body or extremity position without assistance Nutrition Provide skin care as appropriate for patient __________________________________________________________________________________________________________ Provide interventions listed above as appropriate o 4. Excellent – eats most of every meal. Never refuses a meal o 3. Adequate – eats over half of most meals. Occasionally will refuse a meal, but will usually take a supplement when offered o o Provide tray set up and other routine assistance as needed __________________________________________________________________________________________________________ Provide interventions listed above as appropriate Encourage meals and assist with meals as needed Ask family members to participate in selecting meal options, sharing meal with patient Encourage ordered supplements Oral care Daily weight Nutrition consult __________________________________________________________________________________________________________ 2. Probably inadequate – rarely eats a complete meal and generally eats only about ½ of any food offered Provide interventions listed above as appropriate Feed patient __________________________________________________________________________________________________________ 1. Very Poor – never eats a complete meal / rarely eats more than 1/3 of any food offered. Is NPO or maintained on clear liquids or IVs for more than five (5) days. Provide interventions listed above as appropriate Address NPO status __________________________________________________________________________________________________________ Page 3 of 6 Friction – when skin moves against support surfaces Shear – when skin and adjacent bony surface slide across one another Tissue Perfusion & Oxygenation (Braden Q only) Ages 8 and below Friction and Shear Attachment A3 - BHCS Pressure Ulcer Prevention and Intervention Guideline o 3. No Apparent Problem – moves in bed and in chair independently and has sufficient muscle strength to lift up completely during move. Maintains good position in o 2. Potential Problem – moves freely or requires minimum assistance o bed or chair. Provide skin care as appropriate for patient __________________________________________________________________________________________________________ Provide intervention listed above as appropriate Assist with repositioning (agitation, generalized weakness with need for repositioning) Use assistive devices Elevate knee gatch (10-20 degrees) prior to elevating HOB Keep HOB at or below 30 degrees Protect bony prominences __________________________________________________________________________________________________________ 1. Problem – requires moderate to maximum assistance in moving Provide interventions listed above as appropriate __________________________________________________________________________________________________________ o 4. Excellent – normotensive, oxygen saturation >95%, normal hemoglobin, capillary refill <2 seconds o 3. Adequate – normotensive; oxygen saturation may be <95%; hemoglobin may be <10mg/dl; capillary refill may be > 2 seconds; serum pH is normal o o __________________________________________________________________________________________________________ Slow, gradual turns Frequent small shifts in position __________________________________________________________________________________________________________ 2. Compromised – normotensive; oxygen saturation may be < 95%; hemoglobin may be <10mg/dl; capillary refill may be >2 seconds; serum pH is <7.40 Provide interventions listed above as appropriate __________________________________________________________________________________________________________ 1. Extremely Compromised – Hypotensive (MAP<50mmHg; <40 in newborn) or the patient does not physiologically tolerate position changes Provide interventions listed above as appropriate Oxygen as ordered Fluid bolus or vasoactive drug therapy as ordered Specialty support surface __________________________________________________________________________________________________________ Page 4 of 6 STAGE II PRESSURE ULCER A stage II pressure ulcer is a partial thickness loss of dermis presenting as a shallow open ulcer with a red pink wound bed, without slough over a bony prominence. It may also present as an intact or open/ruptured serum-filled or sero-sanginous filled blister over a bony prominence. In addition to Braden interventions: Stage I interventions as appropriate Protect blister to prevent rupture Ruptured blister/open ulcer – cleanse, gently blot dry, protect with moisture barrier or non-adherent dressing Heel ulcer: notify physician if diminished pulses are present Draining ulcer: Calcium Alginate and protective dressing Notify physician _____________________________________________________________________________________________________________ STAGE III PRESSURE ULCER A stage I pressure ulcer is a localized area of intact skin with non-blanchable redness predominantly over bony prominences with possible associated pain, warmth, coolness, firmness, and or softness as compared to surrounding skin. Dark pigmented skin may not have visible blanching but the color of the skin may differ from the surrounding area. In addition to Braden interventions: Position patient off affected area Float heels Protect skin from medical device pressure Protective barrier Specialty support surface Wound care consult Nutrition consult _____________________________________________________________________________________________________________ A stage III pressure ulcer is a full thickness tissue loss. Subcutaneous fat may be visible but bone, tendon or muscles are not exposed. Slough may be present but does not obscure the depth of tissue loss. It may include undermining and tunneling. The depth of a stage III pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have subcutaneous tissue and stage III ulcers can be shallow. In contrast, areas of significant adipose tissue can develop extremely deep stage III pressure ulcers. Bone/tendon is not visible or directly palpable. In addition to Braden interventions: Notify physician Stage I and Stage II interventions as appropriate Notify wound care clinician _____________________________________________________________________________________________________________ STAGE IV PRESSURE ULCER STAGE I PRESSURE ULCER Attachment A3 - BHCS Pressure Ulcer Prevention and Intervention Guideline A stage IV pressure ulcer is a full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present on some parts of the wound bed. Often include undermining and tunneling. The depth of a stage IV pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have subcutaneous tissue and these ulcers can be shallow. Stage IV ulcers can extend into muscle and/or supporting structures (e.g., fascia, tendon or joint capsule) making osteomyelitis possible. Exposed bone/tendon is visible or directly palpable. In addition to Braden interventions Notify physician Stage I, Stage II and Stage III interventions Notify wound care clinician _____________________________________________________________________________________________________________ Page 5 of 6 DEEP TISSUE PRESSURE ULCER Deep tissue pressure ulcer is a purple or maroon localized area of discolored intact skin or blood-filled blister due to damage of underlying soft tissue from pressure and/or shear. The area may be surrounded by tissue that is painful, firm, mushy, boggy, warmer or cooler as compared to adjacent tissue. Deep tissue injury may be difficult to detect in individuals with dark skin tones. Evolution may include a thin blister over a dark wound bed. The wound may further evolve and become covered by thin eschar. Evolution may be rapid, exposing additional layers of tissue even with optimal treatment. In addition to Braden interventions Notify physician Stage I and Stage II interventions as appropriate Notify wound care clinician _____________________________________________________________________________________________________________ UNSTAGEABLE PRESSURE ULCER Attachment A3 - BHCS Pressure Ulcer Prevention and Intervention Guideline Unstageable pressure ulcers are full thickness tissue loss in which the base of the ulcer is covered by slough (yellow, tan, gray, green or brown) and/or eschar (tan, brown or black) in the wound bed. Until enough slough and/or eschar is removed to expose the base of the wound, the true depth, and therefore stage, cannot be determined. Stable (dry, adherent, intact without erythema or fluctuance) eschar on the heels serves as "the body's natural (biological) cover" and should not be removed. In addition to Braden interventions. Notify physician. Stage I and Stage II interventions as appropriate Keep stable eschar dry, adherent and intact Consult physician if signs of change, erythema or fluctuance _____________________________________________________________________________________________________________ Page 6 of 6