pharyngitis, tonsillitis
advertisement
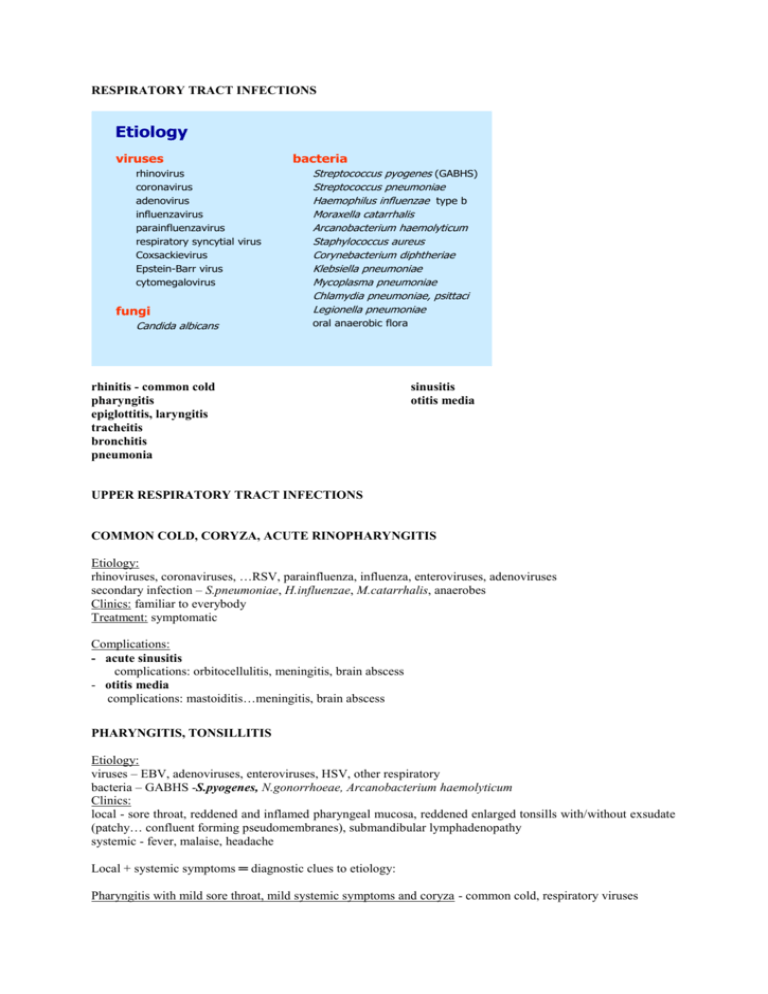
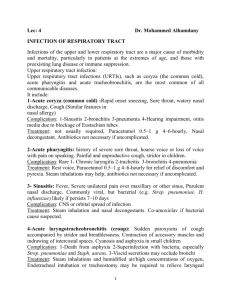
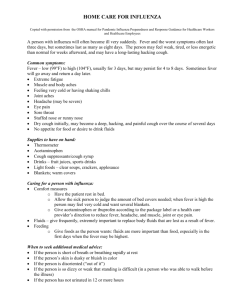
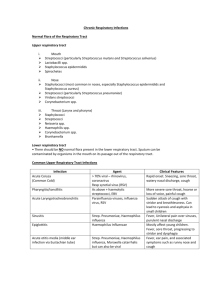
RESPIRATORY TRACT INFECTIONS Etiology viruses rhinovirus coronavirus adenovirus influenzavirus parainfluenzavirus respiratory syncytial virus Coxsackievirus Epstein-Barr virus cytomegalovirus fungi Candida albicans bacteria Streptococcus pyogenes (GABHS) Streptococcus pneumoniae Haemophilus influenzae type b Moraxella catarrhalis Arcanobacterium haemolyticum Staphylococcus aureus Corynebacterium diphtheriae Klebsiella pneumoniae Mycoplasma pneumoniae Chlamydia pneumoniae, psittaci Legionella pneumoniae oral anaerobic flora rhinitis - common cold pharyngitis epiglottitis, laryngitis tracheitis bronchitis pneumonia sinusitis otitis media UPPER RESPIRATORY TRACT INFECTIONS COMMON COLD, CORYZA, ACUTE RINOPHARYNGITIS Etiology: rhinoviruses, coronaviruses, …RSV, parainfluenza, influenza, enteroviruses, adenoviruses secondary infection – S.pneumoniae, H.influenzae, M.catarrhalis, anaerobes Clinics: familiar to everybody Treatment: symptomatic Complications: - acute sinusitis complications: orbitocellulitis, meningitis, brain abscess - otitis media complications: mastoiditis…meningitis, brain abscess PHARYNGITIS, TONSILLITIS Etiology: viruses – EBV, adenoviruses, enteroviruses, HSV, other respiratory bacteria – GABHS -S.pyogenes, N.gonorrhoeae, Arcanobacterium haemolyticum Clinics: local - sore throat, reddened and inflamed pharyngeal mucosa, reddened enlarged tonsills with/without exsudate (patchy… confluent forming pseudomembranes), submandibular lymphadenopathy systemic - fever, malaise, headache Local + systemic symptoms ═ diagnostic clues to etiology: Pharyngitis with mild sore throat, mild systemic symptoms and coryza - common cold, respiratory viruses Pharyngitis with moderate to severe sore throat and systemic symptoms: tonsillitis with/without exudate, acute onset, fever, in children vomiting and abdominal pain – S.pyogenes(GABHS) tonsillitis with confluent exsudate (pseudomembranes), palatal petechiae, cervical lymphadenopathy, hepatosplenomegaly, insidious onset, low-grade fever, no effect of ATB – Epstein-Barr virus, (CMV), infectious mononucleosis nonexudative, catarrhal pharyngitis, nonproductive cough, myalgia, fever – influenza pharyngitis with/without exudate, conjunctivitis, lymphadenopathy, fever - adenoviruses vesicles (blisters) around the soft palate, which soon rupture leaving shallow ulcers, fever Coxsackieviruses – herpangina HSV pharyngitis Diagnosis– to differentiate „strep throat“ and viral pharyngitis: ESR, blood count, differential count of leukocytes, CRP throat swab culture, rapid GABHS antigen detection tests antistreptolysin O titre ALT, AST heterophilic antibodies (agglutinate sheep, bovinne, horse erythrocytes - Ericson, Paul-Bunnell, Monospot test) Streptococcal tonsillitis: raised ESR and CRP, leukocytosis, left shift ASO titres > 400 IU - recent infection, fourfold rise in paired sera is evident of strep. disease. But may be delayed for up to 4 weeks, useful for dg. sequelae. Infectious mononucleosis: atypical lympho-monocytes, raised ALT, AST, heterophilic antibodies, anti-EBV antibodies - anti EA, VCA, EBNA Treatment and complications: Streptococcal tonsillitis Treatment: PNC, alternatively ERY or CEF I., 10days!! Complications: suppurative: peritonsilar abscess (quinsy), lymphadenitis nonsuppurative poststreptococcal sequelae: rheumatic fever, glomerulonephritis Infectious mononucleosis: Treatment: symptomatic - antipyretics, analgesics, nasal decongestant drops Complications: airway obstruction - elevated head, anti-inflammatory drugs, i.v.corticosteroids, intubation or tracheostomy is rarely needed peritonsilar abscess (quinsy) thrombocytopenia, hemolytic anaemia, spleen rupture Rare pharyngitis: Plaut –Vincent´s angina – the synergistic action of the mouth spirochetae Borrelia vincenti and the anaerobe Fusobacterium in persons with poor oral hygiene, extreme soreness of the mouth and gums with offensive halitosis tularaemia - oralglandular form HIV – seroconversion illness – mononucleosis-like illness, with generalized lymphadenopathy and unusual rash, few atypical mononuclear cells Be aware of hematologic malignancies! DIPHTHERIA - Corynebacterium diphtheriae – toxin Clinical forms: - pharyngeal diphtheria – tonsillitis with membranes, marked edema of the cervical lymph nodes („bull-neck“), fever, sore throat - laryngeal diphtheria - nasal, cutaneous, conjunctival diphtheria Resorption of toxin! Diagnosis: non-immunized patient with anamnestic exposure, quickly developing exsudative tonsillitis or respiratory distress Laboratory: specimens from throat, larynx, nose for culture on special media, confirmation of toxin production Complications: toxin - early cardiac damage – myocarditis, conduction defects – heart failure † - late neurological damage (demyelination) – palatal and ocular palsies, peripheral palsies, Guillain - Barré sy - laryngeal, tracheal membrane – airway obstruction and suffocation † Treatment: antitoxin – hyperimmune globulin antibiotics – benzyl-PNC, ERY, CEF I. elective tracheostomy Prevention: diphtheria vaccine (toxoid) ACUTE EPIGLOTTITIS Acute and severe cellulitis of the epiglottis and surrounding tissues, with rapid progression and threatening airway obstruction. Children 1-5 years, average 3y, the incidence has decreased since the introduction of Hib vaccination. Etiology: H. influenzae type b, rarely H. parainfluenzae or GABHS Clinics: abrupt onset with sore throat, fever and toxicity, dysphagia, drooling, respiratory distress with stridor, retractions of the chest wall cherry-red epiglottis may be seen, this should not be attempted, not depress the tongue, fatal occlusion of the airway may occur Diagnosis: history and clinics → emergent transport to the hospital: - direct inspection of the epiglottis only with trained personnel and equipment for maintaining the airway - blood culture, respiratory secretions culture - leukocytosis, left shift, CRP - (lateral neck X-ray – „thumb sign“, in early, less toxic patients) Treatment: adequate airway - intubation, (corticosteroids) antibiotics – CEF III, AMO/inh, CEF II, CHMF Prevention: Hib vaccine LARYNGITIS and CROUP I. Acute viral laryngitis self-limited illness of viral etiology, symptomatic treatment II. Acute viral laryngotracheitis (croup) Clinically distinctive syndrome, characterized by respiratory distress, inspiratory stridor and subglottic swelling. Children few months to 3 years. Etiology: parainfluenza virus type 1,2,3, less freq. influenza, RSV, adenoviruses, Mycoplasma pn. Clinics: often preceding common cold, pharyngitis, fever is variable, hoarseness, „barking“ cough (like a „barking seal“)....at night abruptly respiratory distress with inspiratory stridor Diagnosis: characteristic clinics (neck X-ray shows narrowing of the tracheal air shadow in the subglottic region, not routinely done) Laboratory: resp. secretions - virus isolation (not routinely), serology Treatment: sedation humidification, humidified oxygen corticosteroids nebulized epinephrine (intubation rarely necessary) PERTUSSIS, WHOOPING COUGH Etiology: Bordetella pertussis, parapertussis……..toxins! (Viruses, chlamydiae and mycoplasma can mimic the cough.) Clinics: IP 7-14days, a catarrhal cold with simple cough and slight fever develops (catarrhal phase), after 45days cough progresses to paroxysms (paroxysmal phase), followed by rapid inspiration causing „whoop“, with cyanosis, they repeat 30-40times a day, are often terminated by vomiting or expelling a piece of thick sputum. The infants may have apnoeic attacks. It lasts at least 2-3weeks. Complications: haemorrhage due to raised venous pressure during paroxysms – facial and subconjunctival petechiae, intracerebral haemorrhage in infant encephalopathy (combination of hypoxia and haemorrhage) secondary pneumonia malnutrition Laboratory: absolute and relative lymphocytosis Diagnosis: culture of nasopharyngeal swab on Bordet-Gengou agar serology Treatment: symptomatic: careful observation, a humidified atmosphere, cot oxygen tent, lifting and comforting during paroxysms, cleaning away the mucus, minimizing inhalation of vomit, small frequent feeds, re-feeding when necessary, antitussives have a limited effect antibiotics – ERY Prevention: vaccine – whole-cell killed vaccine (associated encephalopathy not supported by studies), subunit vaccine LOWER RESPIRATORY TRACT INFECTIONS Laboratory diagnosis Sputum microscopy – Gram-stain Sputum culture - the common respiratory pathogens also occur in the normal upper resp. tract flora, semiquantitative culture methods – pathogens reach higher concentrations than commensals ( > 10 6 CFU/ml) Serology for retrospective diagnosis Specimen collection from the lower RT: - sputum obtained by coughing - tracheal aspirate - bronchoscopy with bronchoalveolar lavage or protected brush specimen – when suspicion of unusual pathogens or in immunocompromised pts: tuberculosis, legionellosis, fungal infections, Pneumocystis carinii infection VIRAL INFECTIONS OF THE LOWER RT Bronchiolitis Etiology: RSV, ….parainfluenza 3, other respir. viruses Infants up to 2 years, possible role of RSV in the etiology of SIDS, preterm infants and those with congenital heart disease are at particular risk. Clinics: initially common cold, loose cough, after 3-4 days respiratory distress occurs with tachypnea and intercostal and subcostal retractions, exspiratory wheezing, rhonchi, crepitations resembling asthma, …respiratory insufficiency, cyanosis….heart failure X-ray: hyperinflation with or without infiltrates from atelectasis or concomitant pneumonia Diagnosis: RSV Ag in nasopharyngeal secretions – IFT, EIA virus isolation serology – CFR, IFT, EIA Treatment: oxygenation - cot-sized oxygen tent, ventilatory support bronchodilators (salbutamol) to differentiate asthma adequate hydration virostatics - nebulized ribavirin Complications: secondary bacterial infection…antibiotics Prevention: vaccination Influenza ( x flu-like disease) Etiology: influenzaviruses type A, B, C (orthomyxovirus), the envelope contains 2 glycoproteins – haemagglutinin H and neuraminidase N, both are antigenically variable, type A exists in many H a N subtypes Epidemiology: Epidemics are due to a great antigenic variability: drift (A, B) – a little change in H or N antigen, responsible for the yearly winter epidemics, infection with an epidemic strain provides antibody which will cross-react with closely related types and provides partial immunity to infection by slowly evolving types from year to year shift (A) – major change in H or N antigen, the population has little or no cross-reacting antibody to a new subtype and a pandemy results. Infects and kills ciliated epithelium, airways then susceptible to colonization and invasion by bacterial pathogens. Clinics: IP 1-5 days, abrupt onset of symptoms: systemic – fever (1-5 days), shivering, headache, myalgia, arthralgia, severe malaise, loss of appetite respiratory – dry cough, substernal burning, nasal and pharyngeal symptoms, hoarseness eye – photophobia, painful eye movement uncomplicated lasts 5-7 days Laboratory: nonspecific Diagnosis: epidemic period Ag in respiratory secretions – direct IFT virus isolation in respiratory secretions serology – CFR, IFT, EIA Complications: 1. Pulmonary complications: (viral pneumonitis is common and usually mild) a) severe „influenza“ viral pneumonia - rapid progression of fever, cough, haemorrhagic sputum, dyspnea, hypoxemia, cyanosis, ....progressive deterioration, high mortality despite intensive care - physical exam and X-ray - pulmonary edema, similar to ARDS b) secondary bacterial pneumonia – often elderly or with pulmonary disease - after the period of improvement 1-4 days, relaps of fever with symptoms and signs of bacterial pneumonia – productive cough, chest pain, dyspnea - physical exam and X-ray consistent with bacterial pneumonia - sputum Gram stain and culture – S. pneumoniae, H. influenzae, S. aureus - ATB – AMP(AMO)/inh, CEF I, II 2. Other bacterial infection: sinusitis, otitis media 3. Reye‘s syndrome Most often after influenza B, prior ingestion of aspirin and other salicylates is associated with an increased risk, most patients under 16 years, mortality 20-40%. After several days of influenza CNS signs such as lethargy or drowsiness occur, which may progress rapidly, the liver is enlarged, liver function tests abnormal, treatment only supportive. 4. Myocarditis, pericarditis often subclinical 5. Myositis and myoglobinuria after B, less A, painful leg muscles, elevated serum creatinkinase and urine myoglobin 6. (Meningo)encephalitis, Guillain - Barré syndrome, encephalopathy Treatment: Symptomatic: rest, warmth, adequate hydration, analgesics, vitamin C Antivirotics: amantadine, rimantadine – A, within 48h of onset, side-effects neuraminidase inhibitors: zanamivir, oseltamivir – A,B ATB for bacterial complications Prevention: Vaccination - vaccines are prepared each year from strains similar to those considered most likely to circulate in the forthcoming season. Recommended for persons with chronic respiratory and cardiac disease, chronic renal failure, diabetes and immunosuppression, residents of nursing homes, event. health care workers. Chemoprophylaxis: for high-risk group persons, for whom vaccination is contraindicated, or in the 2 weeks following vaccination before Ab develop amantadine, rimantadine - A neuraminidase inhibitors: zanamivir, oseltamivir – A,B A) community – acquired (CAP) B) hospital – acquired (HAP) PNEUMONIA A) Community – acquired pneumonia Etiology: bacteria, viruses, fungi Predisposing factors: Exposure (epidemiological data): family, job, hobby, travelling Age: very young and elderly neonate: S. agalactiae infant: RSV, influenza, S.pneumoniae, H.influenzae children to teenagers: S.pneumoniae, viruses, H.influenzae (< 5y), Mycopl.pneumoniae (> 5y) young adults (18-45y): Mycoplasma spp., Chlamydia pn., influenza elderly: S.pneumoniae, Legionella, anaerobes, MycoTBC Underlying conditions: alcoholism – S.pneumoniae, anaerobes, H.infl., Kl.pneumoniae, Mycotbc disturbed consciousness, dysphagia - anaerobes COPD – H.infl., S.pneumoniae, Moraxella cat. cystic fibrosis – S.aureus, Pseudomonas preceeding influenza – S.aureus, H.infl., S.pneumoniae Diagnosis: • • • clinical features X-ray laboratory: – blood count, CRP, ESR – biochemistry incl. arterial blood gas analysis microbiology: – sputum Gram stain, culture, ATB sensitivity test – blood culture – – – – pleural effusion culture serology – if no response to beta lactam ATB, test admission serum Ab to Legionella and atypical pathogens (and repeat in 7-14 days) and cold agglutinins (for Mycoplasma infection) bronchoscopy with bronchoalveolar lavage (or bronchial brushing) – microscopy, culture, histology – if severe infection not responding to antibiotics molecular diagnostic methods (PCR) in future Assessment of severity → referral to hospital or home therapy: factors associated with increased mortality: • core factors - if > 2 present, refer to hospital confusion tachypnea > 30/min hypotension < 90/60 tachycardia > 140/min (= signs of sepsis and/or respiratory insuficiency) • age, underlying chronic illness (pulmonary, cardiac, renal, hepatic, diabetes, immunodeficiency), bilateral or multilobar X-ray changes and signs of necrosis (cavitation), signs of complications: pleural effusion, empyema pericarditis metastatic infection sepsis, ARDS, MODS Treatment Choice of initial empirical antibiotic depends on severity: not severe: amoxicillin 500mg-1g q8h oral or clarithromycin 500mg q12h if hospitalised: benzylpenicillin 5-10 mil IU/day i.v. severe: i.v. co-amoxiclav 1,2g q8h or cephalosporin I,II plus erythromycin or clarithromycin (alternative - levofloxacine) Adjustment of antibiotics according to microbiological results: Legionella: erythromycin +/- rifampicin..........or ciprofloxacin Staph. aureus: oxacillin or clindamycin Supportive management: rest, stop smoking, analgesics, humidified oxygen, adequate fluid intake Lobar pneumonia, bronchopneumonia Etiology: S.pneumoniae, H.influenzae, Moraxella cat., S.aureus, Kl.pneumoniae ant other gramnegative aerobes, anaerobes Clinics: rapid onset, high fever and rigors, dry cough, pleuritic chest pain, later sputum volume and purulence increase elderly patients – afebrile, confused severe cases – sepsis syndrome...MOSF on examination - signs of consolidation, bronchial breathing, dull percussion note, crepitations X-ray: lobar pneumonia - dense infiltration, consolidation of lung tissue filling the lobe bronchopneumonia – patchy shadowing, air bronchograms Laboratory diagnosis and treatment – see above. Complications: pleural effusion, empyema pericarditis metastatic infection sepsis, ARDS, MODS Pneumonia associated with influenza epidemics (see in influenza) 1. 2. influenza viral pneumonia secondary bacterial pneumonia Aspiration pneumonia Reduced level of consciousness, seizure disordes, dysphagia due to esophageal or neuromuscular disease, poor dentition. The right lower lobe more often affected. Etiology: mixed (aerobic+anaerobic) oral flora Acute chemical injury due to aspiration of gastric content. Clinics: symptoms of pneumonia + putrid breath odour severe cases – lung abscess, empyema Treatment: G-PNC or AMO/inh or CEF + metronidazole thoracic drainage of empyema, bronchoscopy Atypical pneumonia The term initially used to describe pneumonia which failed to respond to penicillin or sulphonamides and bacteriology failed to provide a diagnosis, is no longer recommended. „Atypical pathogens“ - Mycoplasma pneumoniae, Chlamydia pneumoniae, C. psittaci, Coxiella burnetii Mycoplasma – all ages, commonest in school-age children and young adults, epidemics at 3-4 years interval Chlamydia psittaci – birds: parrots, duck, poultry Coxiella burnetii (Q fever) – sheep Clinics: insidious onset, low-grade fever, sweating, fatigue, dry cough, poor physical findings - discrete crepitations. X-ray: anything from faint segmental opacity to a large and dense consolidation, often much greater than the physical signs suggest. Small or moderate pleural effusion with pleuritic pain. Laboratory: modest neutrophilia or normal blood count, elevated ESR, mildly elevated transaminases Diagnosis: serology cold agglutinins in Mycoplasma infection (may cause hemolysis) Treatment: erythromycin 2-3g/day or doxycycline 200mg/day, 10-14days Legionellosis (Legionnaire´s disease) Legionnaire´s disease – severe systemic infection with pneumonia Pontiac fever – the milder nonpneumonic form Etiology: Legionella pneumophila Transmission by inhalation of contaminated aerosols generated from air condition, hot-water tap, shower outlets, water-cooling towers and whirlpool spas. Can exist within free-living amoebae. The middle-aged and elderly, particularly males, smokers, with underlying chronic respiratory disease. Clinics: symptoms of severe pneumonia, fever, prostration, confusion, vomiting, diarhea, area of consolidation or coarse crepitations Laboratory: neutrophilia, ↑ ESR, signs of renal (↑ urea, creatinine) and hepatic dysfunction (↑ transaminases), hyponatremia X-ray: one or more large opacities Diagnosis: • clinical features – pneumonia + other organs involvement (GIT, kidney, liver, CNS) • L.pneumophila serogroup 1 Ag in urine (ELISA) • L.pneumophila serogroup 1 in sputum (IFT) • culture (on request) of sputum, tracheal aspirate • serology – late positivity!, retrospective dg. Treatment: erythromycin i.v. 3-4g/day plus rifampicin 600-1200mg/d or ciprofloxacin i.v. 400-600mg/day oxygenation, ventilatory support, supportive management Prevention: chlorination of water supplies, heating of hot water over 60 o C, cleaning and disinfection of whirlpool spas. B) Hospital – acquired, nosocomial pneumonia Occurs > 48 h after admission, different etiology, different treatment. Ventilator associated pneumonia (VAP) – particular subgroup. Risk factors: age, underlying chronic/acute illness, immobility, reduced level of consciousness, recent anesthesia, dysphagia, instrumentation of respiratory/GIT tract, use of broad-spectrum ATB. Etiology: early onset – 2-5days – similar to CAP – S.pneum., H.infl. S.aureus late onset - gram-negatives – Enterobacteriacae, Pseudomonas, Acinetobacter, S.aureus, anaerobes, rarely Legionella sp. Clinics: fever, purulent respiratory secretions, respiratory symptoms, new X-ray signs Microbiology: - tracheal aspirate widely used for detection of etiology, of doubtful value, as tracheobronchial colonization is common in critically ill - bronchoalveolar lavage or protected bronchial brushing specimen - blood culture, pleural fluid culture Antibiotic therapy must be guided by culture and sensitivity results. FUNGAL INFECTIONS OF THE LOWER RT Aspergillosis In pre-existing cavities fungal hyphae may produce a ball-shaped growth, which irritates the cavity wall, causing cough and hemoptysis. X-ray – a round, space-occupying lesion surrounded by a narrow clear air space. Treatment: itraconazole, amphotericin B surgery – segmental or lobar resection Histoplasmosis Dry, hot areas, often from dried bird droppings. X-ray resembles tuberculosis, nodular apical lesions, cavities Treatment: amphotericin B, additional itraconazole, fluconazole, surgery for advanced disease Blastomycosis – confined to the USA, similar disease to histoplasmosis Coccidioidomycosis – rapidly progressive bronchopneumonia unresponsive to ATB