Antibiotic Use May Lead to Juvenile Idiopathic Arthritis CME/CE
advertisement

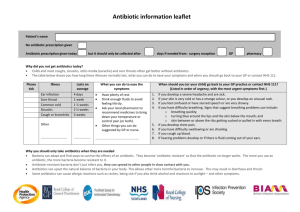
Antibiotic Use May Lead to Juvenile Idiopathic Arthritis CME/CE News Author: Jennifer Garcia CME Author: Charles P. Vega, MD Faculty and Disclosures CME/CE Released: 08/20/2015 ; Valid for credit through 08/20/2016 processing.... CME/CE InformationEarn CME/CE Credit » Clinical Context Antibiotic overprescribing is associated with frightening rates of antimicrobial resistance, as well as increased costs to the individual patient (in terms of adverse events) and society (in terms of higher costs of medical care). A previous study by Kronman and colleagues provided a unique perspective on the issue of antimicrobial overuse among children. This research, which was published in the October 2014 issue of Pediatrics, first performed a meta-analysis to estimate the prevalence of bacterial pathogens in acute respiratory tract infections among children. Second, researchers used these data to evaluate the percentage of appropriate prescriptions for antibiotics among children with acute respiratory tract infections, based on data in the National Ambulatory Medical Care Survey. There were little data on the prevalence of bacteria in upper respiratory tract infections or bronchitis. Streptococcus pyogenes was responsible for 20.2% of cases of pharyngitis among children, and 78% of children with sinusitis in 1 study had a positive bacterial culture result. The prevalence of bacteria in cases of acute otitis media was 64.7%. These data translated into an overall appropriate antimicrobial prescribing rate of 27.4% across all pediatric acute respiratory tract infections in the United States. However, the actual estimated antimicrobial rate for such infections was 56.9%, translating into more than 11 million inappropriate antimicrobial prescriptions per year. Clinicians may be less likely to prescribe antibiotics if they might contribute to a higher risk for chronic illness among children. A previous study linked the use of antibiotics during childhood with a higher risk for juvenile idiopathic arthritis (JIA), the most common rheumatic illness among children. The current study by Horton and colleagues further explores this issue while accounting for the possible effects of infection itself on incident JIA. Study Synopsis and Perspective Past antibiotic exposure may be associated with newly diagnosed JIA, which suggests that alterations in the human microbiome may be implicated in the development of the disease. The results of the case-control study were published online July 20 in Pediatrics. Using a population-representative electronic medical records database in the United Kingdom, researchers identified 152 children (aged 1-15 years) newly diagnosed with JIA between 1994 and 2013. They compared each case with 10 age- and gender-matched control participants who did not have immunodeficiency, inflammatory bowel disease, or system rheumatic diseases. The authors evaluated all antibiotic courses among both groups and included data on the timing, duration, and dose of antibiotic exposure. One or more courses of antibiotic therapy were associated with an increased risk for the development of JIA when compared with control participants (adjusted odds ratio [OR], 2.1; 95% confidence interval [CI], 1.2-3.5), and "[t]he magnitude of the association increased with additional antibiotic courses." This association was noted after adjustment for matching, previous infection, or other autoimmune disease. Furthermore, the researchers found that antibiotic prescription within 1 year of a diagnosis of JIA showed the strongest association with development of the disease, but there was no difference among antibiotic types. To address whether infections rather than antibiotic use could be associated with an increased risk for the development of JIA, the authors compared the risk among patients with treated vs untreated upper respiratory tract infections and found that those treated with antibiotics were more strongly associated with later development of JIA. The authors, led by Daniel B. Horton, MD, MSCE, from the Perelman School of Medicine at the University of Pennsylvania, Philadelphia, acknowledge limitations of the study, such as the fact that unspecified subcategories of JIA made it difficult to determine whether an association exists between antibiotic use and particular JIA categories. They also note that the relatively young patient population (median age, 3 years in both groups) limits the generalizability of these findings to older children and adolescents. "Our study supports the hypothesis that antibiotic exposure is associated with an increased risk of developing JIA," write Dr Horton and colleagues. "This public health finding is potentially important, considering that approximately one-quarter of antibiotics prescribed for children, and an estimated one-half of antibiotics for acute respiratory infections, may be unnecessary and potentially avoidable." Dr Horton and colleagues also point out that previous studies have suggested a link between disturbance of the human microbiome and inflammatory diseases, including at least 1 type of JIA. "Our finding that antibiotic exposure is most strongly associated with JIA within 1 year of diagnosis (and 6 months of first symptom/referral) supports the hypothesis that antibiotic-induced microbiome dysregulation could precipitate JIA in children predisposed to this disease," they write. In an accompanying editorial, Jennifer L. Goldman, MD, MS, and Mary Anne Jackson, MD, from Children's Mercy Hospitals & Clinics and University of Missouri-Kansas City, note that although the study does not confirm a causal relationship between antibiotic use and the development of JIA, it underscores the need for further research into the association between antibiotic use and the development of systemic inflammation. Dr Goldman and Dr Jackson posit that these findings "may represent the tip of the iceberg," and that "[b]oth the well-recognized and currently unknown, undesired sequelae of antibiotic prescribing should give clinicians and patients pause when an antibiotic is prescribed." As reported previously by Medscape Medical News, Dr Horton and colleagues presented an earlier version of their study at the American College of Rheumatology 2014 Annual Meeting. The authors and the editorialists have disclosed no relevant financial relationships. Pediatrics. Published online July 20, 2015. Full textEditorial full text Study Highlights Study data were drawn from The Health Improvement Network, which contains electronic medical records from more than 550 general practitioner practices in the United Kingdom. Specifically, researchers were interested in demographic, diagnosis, and treatment information within the database. Researchers focused on children between 1 and 15 years old. They identified children with JIA and excluded children with previous diagnoses of inflammatory bowel disease, immunodeficiency, or other systemic rheumatic disease. Control participants were paired with children with JIA in a 10:1 ratio. Researchers evaluated the relationship between antimicrobial prescriptions and the diagnosis of JIA. They performed evaluations to determine whether the type of antibiotic prescribed or when the prescription occurred might have differential effects on the risk for JIA. The study analysis accounted for the potential role of infection itself in promoting JIA by comparing rates of infection of cases of JIA and controls. 454,457 children with a total of 3.1 million person-years of follow-up were included in the study. The median age was 3 years, and 63% of children were girls. 152 cases of JIA were diagnosed in the study cohort. Rates of any infection and hospitalization for infection were higher among patients vs control children, and children with JIA had more clinician visits overall. After adjustment for the higher rate of infection, the adjusted OR of JIA associated with at least 1 antibiotic prescription was 2.1 (95% CI, 1.2-3.5). Adjustment for specific types of infections or the total number of infections failed to substantially alter this result. There was a significant trend toward a higher risk for JIA with more courses of antibiotics prescribed. The age of the child at the first prescription for antibiotics was irrelevant to the risk for JIA, but antibiotic prescriptions within 1 year of the diagnosis of JIA were most strongly associated with the risk for disease. Untreated infections were not associated with a higher risk for JIA, regardless of the age of onset. There was no difference in the associated risk for JIA in comparing antibiotics used to treat aerobic vs anaerobic bacteria. Antifungal and antiviral treatment did not substantially alter the risk for JIA. Clinical Implications A previous study by Kronman and colleagues found evidence of bacterial infection in 64.7% of cases of acute otitis media among children, and 20.2% of cases of pharyngitis were caused by S pyogenes. The estimated rate of appropriate antimicrobial prescriptions for acute respiratory tract infections among children was 27.4%, but the actual prescription rate was approximately double this value. The current study by Horton and colleagues finds that antibiotic prescriptions are associated with a higher risk for JIA, and the risk for JIA was unaffected by untreated infections. There was a progressive increase in the risk for JIA with a higher number of antibiotic prescriptions, and antifungal and antiviral treatment had no effect on the risk for JIA. Implications for the Healthcare Team: Minimizing the inappropriate application of antibiotics among children requires a team approach of listening, support, and education. The healthcare team should coordinate their policy and actions in order to minimize inappropriate prescribing. CME Test http://w w w .meds /qna/processor/3 36841 true To receive AMA PRA Category 1 Credit™, you must receive a minimum score of 75% on the post-test. Questions answered incorrectly will be highlighted. 3 INTERNAL 276341 You are seeing a 4-year-old girl with a 2-day history of mild fever, sore throat, and congestion. Her symptoms and physical examination suggest a viral upper respiratory tract infection, but her parents clearly want an antibiotic "to help her get better faster." What should you consider regarding acute respiratory tract infections and antibiotic prescriptions among children in the previous study by Kronman and colleagues? RADIOBUTTON 0 Bacteria were present in fewer than half of cases of acute otitis media Approximately 20% of cases of pharyngitis were caused by S pyogenes An antibiotic was indicated in less than 5% of all cases of acute respiratory tract infection The actual prescription rate for antibiotics was similar to the rate of appropriate treatment of bacteria in acute respiratory tract infections 276343 What should you consider regarding the results of the current study by Horton and colleagues as you evaluate this patient? RADIOBUTTON 0 There was a progressive increase in the risk for JIA with a history of more antibiotic prescriptions Only children prescribed antibiotics 5 or more times experienced a higher risk for JIA Infections, but not antibiotic prescriptions, accounted for a higher risk for JIA The risk for JIA was substantially higher among children receiving antifungal vs antibacterial medications Save and Proceed