An Overview of Hypoglycemia
advertisement

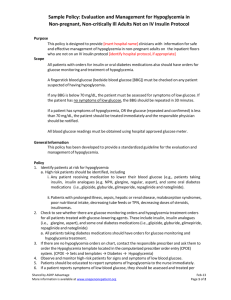
An Overview of Hypoglycemia Karen K. O’Brien, BS Pharm, PharmD Assistant Professor of Pharmacy Science Creighton University School of Pharmacy and Health Professions Omaha, Nebraska Alan W. Y. Chock, PharmD Assistant Professor of Pharmacy Practice Creighton University School of Pharmacy and Health Professions Omaha, Nebraska Janet L. Shea, RN, BSN, MPA Nursing Staff Hampden-Wilbraham Regional School District Wilbraham, Massachusetts 6/20/2012 US Pharm. 2012;37(6):50-56. Hypoglycemia is a low concentration of glucose in the blood, but no specific plasma glucose level defines the condition.1 Rather, hypoglycemia is best described as a plasma glucose concentration sufficiently low to elicit signs and/or symptoms.1 In healthy individuals, the glycemic threshold for symptoms is 50 to 55 mg/dL, although plasma glucose levels under 70 mg/dL signal impending hypoglycemia.2 Symptoms can occur at higher concentrations in patients with poorly controlled diabetes, and at lower levels in those with tight glycemic control or recent hypoglycemic exposure.2 Most hypoglycemia is iatrogenic and associated with drug-treated diabetes mellitus.1 Other causes of hypoglycemia, rare in individuals older than 10 years of age, will be briefly discussed later. Glucose supplies immediate energy needs and fuels metabolic functions between meals. If it is not needed for immediate use, glucose is stored as glycogen in the liver and muscles, or else as fat.3 Glucose is a requisite metabolic fuel for brain cells. Because the brain can neither synthesize glucose nor store more than a few minutes’ supply in the form of glycogen, it is critically important that a steady glucose supply be available to brain cells via the circulation.2 In healthy individuals, a finely choreographed interaction between insulin and several counterregulatory hormones, including glucagon, epinephrine, cortisol, and growth hormone, ensures that blood glucose concentrations are maintained within the physiological range. This process is called glucose counterregulation. As plasma glucose concentrations drop below physiological range, insulin secretion decreases and ultimately ceases. Glucagon and epinephrine concentrations increase concurrently to produce a rapid rise in plasma glucose, thus averting or swiftly correcting hypoglycemia.2 Glucagon stimulates glycogenolysis (the breakdown of glycogen into glucose) in the liver, as well as hepatic gluconeogenesis (the formation of glucose from noncarbohydrate substrates). Epinephrine promotes hepatic glycogenolysis and hepatic and renal gluconeogenesis. Cortisol and growth hormone work slowly over hours to defend against prolonged hypoglycemia, but they play a minimal role in reversing hypoglycemia.1 HYPOGLYCEMIA IN PATIENTS WITH DIABETES The goal of diabetes management is a lifetime of euglycemia without hypoglycemia.4 Hypoglycemia constitutes a significant roadblock to achieving both short-term and long-term glycemic control, which may lead to the development of long-term complications of diabetes.2 It is estimated that, on average, individuals with type 1 diabetes mellitus (T1DM) experience two symptomatic episodes of hypoglycemia weekly and one severe event annually. With declining pancreatic function, the incidence of hypoglycemia increases in type 2 diabetes mellitus (T2DM).2 The negative effects of hypoglycemia include psychological morbidity, physical morbidity, and mortality. In patients with diabetes, the fear of hypoglycemia exceeds the fear of long-term complications.2 Pathophysiology In T1DM and advanced T2DM, glucose counterregulation is compromised by the impaired secretion of insulin, glucagon, and epinephrine, breaching three physiological defenses against hypoglycemia. First, falling plasma glucose concentrations fail to elicit a corresponding decrease in insulin secretion in patients taking insulin or insulin secretagogues. With absolute or relative exogenous insulin excess, insulin activity is dictated by the pharmacokinetic characteristics of the drug. Second, hypoglycemia does not trigger glucagon secretion. Third, a lower plasma glucose concentration is required to stimulate an epinephrine response.2 Hypoglycemia Unawareness Some patients with T1DM or advanced T2DM lose the neurogenic warning symptoms that herald impending hypoglycemia. This state, hypoglycemia unawareness, is likely the result of repeated iatrogenic hypoglycemia episodes that lead to impaired epinephrine response and diminished neurogenic symptoms.2 The weakened counterregulatory response, hypoglycemia-associated autonomic failure (HAAF), puts the patient at high risk for severe hypoglycemia. Fortunately, a 2- to 3week period of strict avoidance of hypoglycemia appears to improve the epinephrine response and restore hypoglycemia awareness.2,3 Causes and Risk Factors Iatrogenic hypoglycemia results from therapy that raises insulin concentrations and lowers plasma glucose concentrations.1 Agents include insulin and insulin secretagogues. Other diabetes drugs may cause hypoglycemia when combined with insulin or insulin secretagogues (TABLE 1). Conventional risk factors for iatrogenic hypoglycemia relate to relative or absolute insulin excess (FIGURE 1). As discussed previously, HAAF is associated with a high risk of hypoglycemia. Risk factors include an absolute deficiency of endogenous insulin; a history of severe hypoglycemia and/or hypoglycemia unawareness, as well as recent hypoglycemia, prior exercise, and sleep; and intensive glycemic therapy as evidenced by lower glycosylated hemoglobin concentrations and/or lower glycemic goals.1 Symptoms of Hypoglycemia A reduction in blood glucose initiates an autonomic nervous system response, resulting in neurogenic signs and symptoms (categorized as adrenergic or cholinergic) that alert the patient to a hypoglycemic episode (TABLE 2). Each patient’s array of symptoms is unique and may vary in magnitude over time. However, signs and symptoms often present in diabetes are also frequently associated with other disease states, and hypoglycemia does not necessarily elicit these signs and symptoms. Thus, hypoglycemia is best confirmed by Whipple’s triad: symptoms consistent with hypoglycemia, a low plasma glucose concentration, and symptom relief when the glucose concentration is raised.4 Optimally, the presence of signs and symptoms during mild hypoglycemia prompts the patient to ingest carbohydrates, thereby enabling blood glucose concentrations to normalize. If the episode progresses, the deficiency of glucose in brain cells results in neuroglycopenic symptoms. Lack of attention to mild symptoms or compromised autonomic response signals may preclude recognition of a hypoglycemic event. The pharmacist should counsel the patient to be attentive to symptoms, self-monitor blood glucose (SMBG) whenever suspicious, and treat for hypoglycemia if monitoring is not available.2 It is estimated that more than 50% of hypoglycemic episodes occur during sleep, and the sufferer usually is unaware of them.4 An individual might assume the occurrence of hypoglycemia if he or she awakens with bedclothes damp with sweat and is confused, irritated, or tired, or was calling out or having nightmares during sleep.3 In such cases, periodic 3-AM SMBG is recommended to determine whether hypoglycemia is occurring overnight. Nighttime hypoglycemia is suspected of causing arrhythmias that lead to unforeseen death, or dead-in-bed syndrome.1 Treatment of Mild-to-Moderate Hypoglycemia When hypoglycemia is suspected, SMBG should be performed if a meter is available. A reading below 70 mg/dL indicates the need for immediate consumption of 15 to 20 g of simple carbohydrates, preferably glucose.5 If testing is not possible, remember: “When in doubt, treat.” Untreated hypoglycemia presents a greater risk than that posed by an episode of hyperglycemia. Severe and protracted neuroglycopenia, although rare, may lead to permanent brain damage and even death.2 Recommended carbohydrates include 3 to 4 glucose tablets (5 g each); 1 tube of glucose gel; 4 oz. fruit juice or soft drink (not sugar free); 8 oz. milk (low-fat preferred); 4 to 6 pieces of hard candy (not sugar free); or 1 tbsp. sugar, honey, or corn syrup. Protein does not impair the desired glycemic response, but fat does. Therefore, chocolate candy is not recommended unless no other simple carbohydrate is available. Blood glucose should be rechecked at 15-minute intervals, and treatment repeated if glucose remains below 70 mg/dL. Once blood glucose is at or above 70 mg/dL, the patient should eat a snack or meal to maintain euglycemia.3 Treatment of Severe Hypoglycemia Neuroglycopenia can impair an individual to the extent that someone else must administer treatment. If the patient can safely swallow, glucose gel, honey, jelly, or syrup should be placed inside the cheek for absorption. If the patient is unable to swallow or is unconscious, a glucagon injection is required to rapidly elevate the serum glucose level.3 IV dextrose is the preferred treatment for hospitalized patients. Once conscious, the patient should drink a carbohydrate-rich fluid, followed by a snack once he or she is no longer nauseated. Medical supervision is indicated until the risk of recurrent hypoglycemia has passed.2 HYPOGLYCEMIA PREVENTION A prudent pharmacist counsels patients with diabetes on hypoglycemia avoidance during each contact.1 Patients should follow a diabetes management plan that includes blood glucose monitoring (with scrupulous monitoring when ill), a medication protocol, meal and snack planning, management of activity and exercise, and moderate alcohol ingestion.3 The patient should be reminded that diabetes medication may need to be adjusted to respond to changes in food ingestion and physical activity. The pharmacist should ascertain that the patient knows how to use his or her meter, and should suggest alternative solutions if medications or meter supplies are a financial hardship. Information on medications that are more likely to cause hypoglycemia should be provided, and patients taking acarbose or miglitol should be cautioned that only dextrose will raise blood glucose during a hypoglycemic episode.3 The pharmacist should offer glucagon emergency kit training to the patient’s family members. The patient should be reminded to carry a simple carbohydrate source—preferably glucose tablets—at all times and to avoid the accidental consumption of sugar-free candy or soft drinks in the treatment of hypoglycemia. The patient should be advised to perform SMBG before driving if he or she is at risk for hypoglycemia, to test often during long driving trips, and to refrain from driving until blood glucose is at least 70 mg/dL.3 The pharmacist must recognize that information and willingness to follow a diabetes management plan are essential for enabling a patient to avoid hypoglycemia and live successfully with diabetes.2 NONIATROGENIC HYPOGLYCEMIA Hypoglycemia can occur in those not being treated for diabetes. Organizations such as the National Institutes of Health and the National Diabetes Information Clearinghouse note the existence of several types of noniatrogenic hypoglycemia. Reactive (Postprandial) Hypoglycemia Reactive hypoglycemia occurs within 4 hours after a meal is consumed, with diagnosis based on documentation of Whipple’s triad.1,3 Several causes have been proposed but are unsubstantiated, including excessive release of insulin following high sugar intake, enhanced sensitivity to the normal secretion of epinephrine and its attendant hypoglycemic symptoms, and deficient glucagon secretion.3 Gastrointestinal surgery can cause hypoglycemia if food passes into the small intestine too quickly, but this is uncommon. Rare hereditary enzyme deficiencies can lead to fructose intolerance and reactive hypoglycemia.3 Fasting (Postabsorptive) Hypoglycemia This condition may be diagnosed when the serum glucose concentration is below 50 mg/dL after overnight fasting, between meals, or following physical activity.3 Several underlying conditions can contribute to fasting hypoglycemia, including the consumption of medications other than those used to treat diabetes (TABLE 3). Alcohol consumption, especially binge drinking, can cause severe or even fatal hypoglycemia by halting gluconeogenesis and depleting hepatic glycogen.6 Critical illnesses affecting the liver, heart, or kidneys can contribute to fasting hypoglycemia.3 Sepsis can deplete hepatic glycogen stores and impair gluconeogenesis.7 Disorders involving renal insufficiency can decrease drug elimination and affect serum glucose concentration.8 Starvation conditions (e.g., anorexia nervosa) can deplete glycogen and fat stores used for energy between meals, as well as substrates used in gluconeogenesis. Treatment of the underlying cause will help resolve hypoglycemia. Deficiencies of glucagon, epinephrine, cortisol, and growth hormone, which are rare, are usually corrected by exogenous hormone supplementation.3 Such conditions are more common in very young children than in adults. Insulinomas—rare, usually benign pancreatic tumors that secrete excessive amounts of insulin—can cause hypoglycemia.1,3 Surgical removal of the insulinoma is preferred, but pharmacologic agents such as diazoxide or octreotide also may be used to lower serum insulin concentrations. CONCLUSION Hypoglycemic episodes compromise wellness in all who experience them. In diabetic patients, the risk of hypoglycemia may limit the potential for lifelong euglycemia.2,4 Pharmacists who offer education and support afford their patients the opportunity to better understand and follow their disease-management plans and to enjoy better health. REFERENCES 1. Cryer PE, Axelrod L, Grossman AB, et al. Evaluation and management of adult hypoglycemic disorders: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2009;94:709-728. 2. Cryer PE, Davis SN, Shamoon H. Hypoglycemia in diabetes. Diabetes Care. 2003;26:1902-1912. 3. National Diabetes Information Clearinghouse. Hypoglycemia. http://diabetes.niddk.nih.gov/dm/pubs/hypoglycemia/#nodiabetes. Accessed October 6, 2011. 4. American Diabetes Association. Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia. Diabetes Care. 2005;28:1245-1249. 5. American Diabetes Association. Executive summary: standards of medical care in diabetes—2012. Diabetes Care. 2012;35(suppl 1):S11-S63. 6. Masharani U. Diabetes mellitus and hypoglycemia. In: McPhee SJ, Papadakis MA, Rabow MW, eds. CURRENT Medical Diagnosis and Treatment 2012. 51st ed. New York, NY: McGraw-Hill Medical; 2011. 7. Miller SI, Wallace RJ Jr, Musher DM, et al. Hypoglycemia as a manifestation of sepsis. Am J Med. 1980;68:649-654. 8. Mayo Clinic. Hypoglycemia. Causes. www.mayoclinic.com/health/hypoglycemia/DS00198/DSECTION=causes. Accessed March 27, 2012. 9. Thomson Reuters Micromedex 2.0. www.micromedex.com. Accessed March 25, 2012. 10. Vue MH, Setter SM. Drug-induced glucose alterations part 1: drug-induced hypoglycemia. Diabetes Spectrum. 2011;24:171-177. 11. MedlinePlus. Drug-induced hypoglycemia. www.nlm.nih.gov/medlineplus/ency/article/000310.htm. Accessed March 25, 2012. 12. CDC. Treatment of malaria (guidelines for clinicians). www.cdc.gov/malaria/resources/pdf/clinicalguidance.pdf. Accessed May 1, 2012. 13. Kojak G Jr, Barry MJ Jr, Gastineau CF. Severe hypoglycemic reaction with haloperidol: report of a case. Am J Psychiatry. 1969;126:573-576. 14. Walter RB, Hoofnagle AN, Lanum SA, Collins SJ. Acute, life-threatening hypoglycemia associated with haloperidol in a hematopoietic stem cell transplant recipient [letter]. Bone Marrow Transplant. 2006;37:109-110. To comment on this article, contact rdavidson@uspharmacist.com.