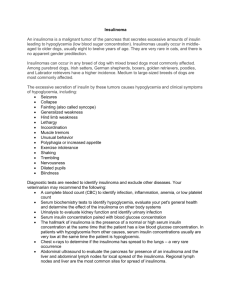
Insulinoma 2012
advertisement

Insulinoma 2012 30 years experience with diagnosis and treatment Jan Škrha 3rd Department of Internal Medicine, 1st Faculty of Medicine, Charles University in Prague 27th Symposium of the Federation of the International Danube-Symposia of Diabetes Mellitus, Budapest, 28-30th June, 2012 CAUSE OF HYPOGLYCEMIA 1. According to pathogenesis a) decreased glucose production - lack of contraregulatory hormones - liver or kidney disease, alcohol b) increased glucose utilisation - exogenously caused (DM treatment) - endogenously caused (insulinoma) 2. According to timing of the food ingestion a) fasting hypoglycemia (!!!) b) random hypoglycemia during the day - reactive (functional), postoperative Hypoglycemia and activation of contraregulatory hormones Glucose Hormone 3,8-3,6 mmol/l 3,5-3,2 mmol/l 3,1-2,7 mmol/l 2,8-2,6 mmol/l glucagon catecholamines growth hormone cortisol neurogenic symptoms neuroglycopenic symptoms HYPOGLYCEMIC SYMPTOMS 1) neurogenic: (adrenergic) sweatting, palpitations, tachycardia, anxiety, tremor 2) neuroglycopenic: a) neurologic: confusion,headache, blurred vision, diplopy, dysarthria, decreased abbility to concentrate, impaired speech and consciousness, cramps, epilepsy b) psychiatric: unusual hesitation, temper changes (depression, euphory) impaired thinking Characteristics of the patients (3rd Departmrent of Internal Medicine: 1980 – 2012) Males / females Age (yrs) Organic Functional hyperinsulinism hyperinsulinism (n = 125) (n = 30) 32 / 93 (~ 75 % women) 7 / 21 52 ± 17 27 ± 5 Duration of the disease (yrs) 3 (0,1 – 25) 1 (0,5 – 2) BMI (kg/m2) 28,2 ± 5,3 (32 % normal) 24,3 ± 2,9 Blood pressure – systolic (mm Hg) diastolic 134 ± 17 125 ± 15 (55 % normal) 79 ± 10 78 ± 6 Fasting test 100 7 60 6 50 4 3 IRI/G (mU/mmol) 5 IRI (mU/l) Glucose (mmol/l) 80 60 40 40 30 20 2 20 10 1 0 Before Positive: After 100 % 0 Before After 91 % 0 Before After 98 % Organic hyperinsulinism (3rd Department of Internal Medicine: 1980 – 2012) Imaginating method Positive Negative Finding by surgery Confirmed from positive Removed US 4 (8 %) 47 (92 %) 2 (50 %) 45 (88 %) EU 41 (84 %) 8 (16 %) 33 (83 %) 45 (94 %) CT 27 (30 %) 64 (70 %) 22 (85 %) 86 (95 %) AG 39 (43 %) 52 (57 %) 25 (64 %) 89 (94 %) Localised ~ 70 % of insulinomas before operation Octreoscan TREATMENT a) surgical - by laparotomy - by laparoscopy b) conservative - regimen (diet, activity) - pharmacological (diazoxide, octreotide) Enucleation Resection (hemipancreatectomy) INSULINOMA – RESULTS OF TREATMENT (3rd Department of Internal Medicine, 1980-2012) 125 insulinomas / microadenomatosis 115 operated 10 conservatively in 104 removed (90 %) in 11 undiscovered 3 removed 8 conservative (by reoperation) Surgical success: 93 % Agreement with preoperative examination : 64 of 81 (79 %) Histology Surgical and histological finding a) localization (n=115) Head: 30 % Body: 28 % Tail: 42 % b) histology Benign adenoma: 103 Malign carcinoma: 4 Uncertain biological activity: 5 Multiple microadenomatosis: 3 DIAGNOSIS Algorithm of diagnosis in organic hyperinsulinism Clinical suspition Biochemical examination Diagnosis confirmed Diagnosis unconfirmed Topographic localisation TREATMENT CT Angiography Endosonography Localisation confirmed Localisation unconfirmed Surgery Insulinoma removed Insulinoma unremoved Conservative treatment In differential diagnosis: HYPOGLYCEMIA FACTITIA HYPOGLYCEMIA FACTITIA Characteristic signs: - suspicion on insulinoma - uncertainty from clinical picture - uncertainty from laboratory findings - frequent relationship of the patient to health care providers Attention: IATROGENIC HYPOGLYCEMIA Insulinoma vs hypoglycemia factitia Laboratory variable Plasma glucose Insulinoma Hypoglycemia Hypoglycemia factitia factitia caused by insulin caused by sulphonylurea ↓↓↓ ↓↓↓ ↓↓↓ Plasma insulin ↑ - ↑↑↑ ↑↑↑ ↑↑↑ ↓ - ↓↓ ↑ - ↑↑ ↑ - ↑↑ ↔ ↔ negative negative positive Serum C-peptide ↑ - ↑↑ Plasma proinsulin Sulphonylurea (urine) Conclusions for clinical practice Hypoglycemia is deleterious for organism and is life threatening • to analyse symptoms (history !) • to confirm hypoglycemia • to elucidate cause of hypoglycemia (confirm diagnosis) • to realize reliable treatment strategy removing hypoglycemia (related to diagnosis and clinical state of the patient) Collaboration Surgery: Jan Šváb, Ladislav Krušina (†) Biochemistry: Jirina Hilgertová Marcela Jarolímková Pathologist: Jaroslava Dušková Metabolic ward staff: Eva Kotrlíková Gustav Šindelka (†) Imaging: Josef Hořejš, Radan Keil