Evaluation of conventional v. intensive blood glucose control
advertisement

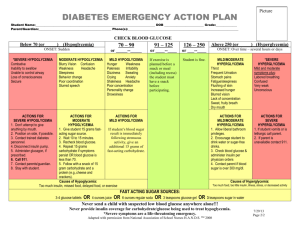
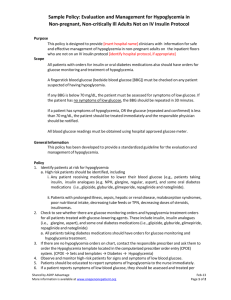
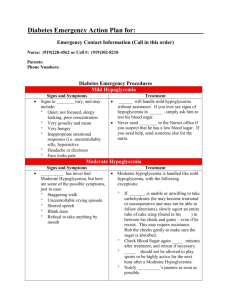
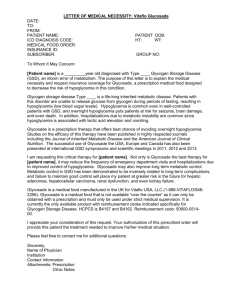
Glycemic Control in Critically Ill Patients EVALUATION OF CONVENTIONAL V. INTENSIVE BLOOD GLUCOSE CONTROL DANELLE BLUME UNIVERSITY OF GEORGIA COLLEGE OF PHARMACY 2013 PHARM.D. CANDIDATE Hyperglycemia in the ICU A common occurrence in both diabetic and non- diabetic patients Defined as a blood glucose > 200 mg/dl Etiology Severe trauma, disease, infection, surgery, etc. result in the activation of the hypothalamic pituitary adrenal (HPA) axis Release of glucagon, growth hormone, and cortisol in addition to norepinephrine and epinephrine Blood insulin levels remain normal or low Insulin resistance, preexisting or not Fluids (D5W), Medications, TPN, etc. Treatment of Hyperglycemia Insulin infusion Titrate every hour according to protocol Hypoglycemia in the ICU Blood glucose < 70mg/dl Result of overcorrection of hyperglycemia Whipple’s triad Signs and/or symptoms consistent with hypoglycemia Low plasma glucose Relief of symptoms after plasma glucose is increased Life threatening http://diabeticradio.com/?page_id=685 Treatment of Hypoglycemia Intravenous glucose (25g) as a 50% solution Followed by constant infusion of 5% or 10% dextrose If IV access not possible: Glucagon (1.0 mg for adults) SC or IM Goal glucose: 110-180, but this is a wide range and a debatable one Conflicting Findings Initial trials suggested that intensive glucose control could reduce mortality among patients in surgical ICU and reduce morbidity among those in a medical ICU* Subsequent studies have NOT confirmed this NICE-SUGAR trial shows increased risk of death in patients assigned to intensive glucose control * Van den Berghe G, Wouters P, Week- ers F, et al. Intensive insulin therapy in critically ill patients. N Engl J Med 2001; 345:1359-67. Van den Berghe G, Wilmer A, Her- mans G, et al. Intensive insulin therapy in the medical ICU. N Engl J Med 2006; 354:449-61. NICE-SUGAR Normoglycemia in Intensive Care Evaluation— Survival Using Glucose Algorithm Regulation A multicenter, randomized, controlled trial 6104 adults in ICUs in 42 hospitals between 2004 & 2008 Intensive blood glucose control group (target BG range 81-108 mg/dl) v. conventional glucose control (target 180 mg/dl or less) Intervention continued until patient was eating, discharged from ICU, or died Primary outcome: death within 90 days after randomization Severe hypoglycemia = 40 mg/dl or less Moderate hypoglycemia = between 41 and 70 mg/dl NICE-SUGAR Evidence: Ia Recommendation Grade: A Overall Conclusion: Although hypoglycemia was significantly more common among patients assigned to intensive versus conventional glucose control, the association of hypoglycemia with death was similar in the two groups NICE-SUGAR Post-hoc analysis Whether hypoglycemia leads to death in critically ill patients is unclear Findings Even after adjustment for events occurring after the first episode of hypoglycemia, moderate hypoglycemia was associated with an increased risk of death of 40% and severe hypoglycemia with a doubling of the risk Causal relationship is plausible because hypoglycemia may increase mortality by impairment of other systems Hypoglycemia may be a marker of severe underlying disease processes Autonomic function, alteration of blood flow and composition, white-cell activation, vasoconstriction, and the release of inflammatory cytokines Relevance A wise man once said, “Hyperglycemia in the acute setting isn’t going to kill you but hypoglycemia will.” Hal Richards, Pharm.D., BCNSP, Candler Hospital Thus, until we have data that says otherwise, intensive glucose control in the ICU should be avoided. A target blood glucose of 130-180 mg/dl is a reasonable goal References Annetta MG, Ciancia M, Proietti R. Diabetic and nondiabetic hyperglycemia in the ICU. Current Anaesthesia & Critical Care, 2006 17:6, 385-390. LexiComp. Version 1.10.0(159), 2012. McDonnell ME, and Umpierrez GE. Insulin therapy for the management of hyperglycemia in hospitalized patients. Endocrinology and Metabolism Clinics of North America, March 2012 41:1, 175-201. NICE-SUGAR investigators. Hypoglycemia and Risk of Death in Critically Ill Patients. N Engl J Med 2012;367:1108-18.