INTRODUCTION TO LABORATORY MEDICINE OHIO UNIVERSITY
advertisement

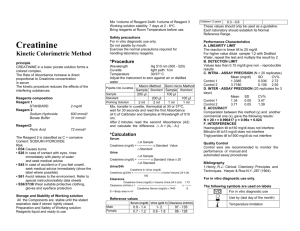
INTRODUCTION TO LABORATORY MEDICINE OHIO UNIVERSITY HERITAGE COLLEGE OF OSTEOPATHIC MEDICINE Scott Jenkinson, D.O. (class of 1983) Associate Professor of Pathology 75 Hospital Dr., ste. 370 Athens, OH 45701 740-566-4530 Pathology as a Medical Specialty Pathology is the study of disease. A.T Still implied that finding disease was easy and that looking beyond the conditions that hinder human achievement was the better goal of a physician. At present, western medicine remains heavily disease based, but there are recent encouraging signs that the maintenance of wellness may become just as important. Pathologists are sometimes called the physician’s physician. They have medical degrees and complete residencies lasting 4 years. The standard residency curriculum includes 2 years of anatomic pathology and 2 years of laboratory medicine. These subdivisions include the following disciplines: Anatomic Pathology Surgical pathology Cytology Autopsy Laboratory Medicine Hematology Clinical chemistry Microbiology Immunology/serology Transfusion medicine Coagulation An emerging discipline is molecular pathology that overlaps with both anatomic pathology and lab medicine. It involves detecting genes and genetic alleles and gene copy number using methods like fluorescent in situ hybridization, RNA microarray hybridization and gene sequencing. Another discipline that doesn’t fit neatly in the above dichotomy is forensic pathology, a field centered on autopsy pathology with the intent of providing answers for the criminal justice and public health systems. Fellowships of 1-3 years in all the pathologic disciplines and several other fields are available. Types of Laboratory Tests Qualitative. The result is positive or negative. An analyte is present in sufficient concentration to be detected by the system. Examples: pregnancy test, HIV antibody test. 1 Semiquantitiative. The result is expressed in arbitrary units for comparison, such as 0, trace, 1+, 2+, 3+, 4+. This allows some degree of comparison when the analyte is tested serially in a patient. Examples: urinalysis dipstick, HER2 protein expression in tumor cell nuclei. Quantitative. Reported as a numeric value, usually a concentration. These test results lend themselves to statistical analysis. Examples: plasma glucose concentration, blood hemoglogin concentration, CSF cell count. Interpretive. The pathologist or clinical chemist collects and reviews data and information and synthesizes an interpretation expressed in the lab report. Examples: surgical pathology report of a breast biopsy, cause and manner of death determination from an autopsy, pap smear cytologic diagnosis, serum protein electrophoresis pattern interpretation. Quantitative Test Reference Ranges Sometimes called normal ranges, a test reference range expresses the most likely test results in a group of people that are healthy and free of diseases that might influence the test results. Reference ranges are created by doing a reference range study in which a suitable number of subjects are tested and their test results analyzed statistically. When test results from the study form a bell shaped curve, it is fairly standard to define the reference range as the mean plus or minus two standard deviations. Considering the area under the bell shaped curve, 95% of the test results in the study group would be within the reference range. Laboratories are required to include a reference range on test results and the laboratory must do a reference range study with sufficient statistical power or verify a test kit manufacturer’s reference range with an in-house study. The statistical nature of reference ranges creates important caveats for physicians who interpret test results in light of the patient’s history and physical exam. 2.5% of healthy, nondiseased people will have a test value below the reference range and 2.5% will have a value above the reference range. Test results much higher or lower than the reference range are more likely to be true abnormal tests and thus indicate disease. When analyzing an abnormal test result, always ask yourself whether the reference range on the report matches the age, gender and ethnicity of your 2 patient. Some laboratories lack the data or the capability of reporting the correct reference range. Test results alone do not typically define disease. Tests have measurable sensitivity and specificity for the detection of disease. It is possible for a patient to have a disease and a false negative lab result and also possible for a healthy person to have a false positive lab result. Decision Levels and Critical Values Some tests are reported with clinical decision levels rather than reference ranges. Reference range reporting for some tests would provide misleading information for test interpretation. Total cholesterol, for example, might have a reference range in a North American population of adults of 150- 300 mg./dL. We know from data collected during the Framingham Heart Studies decades ago that people with a total cholesterol above 240 mg./dL. are at high risk for a myocardial infarction, so a decision level of 240mg./dL. is a more appropriate way of reporting. Critical values are test values so high or low compared to reference ranges that the patient’s life may be immediate danger. Laboratories have policies to notify health care workers of these critical values as soon as they are discovered. This becomes very challenging when the results are discovered after hours and on weekends and holidays. Laboratory Testing About half of all lab tests done on humans in the U.S. are performed in hospital, independent and reference laboratories and the other half are done in physician office labs. The Clinical Laboratory Improvement Amendments (CLIA) federal law enacted in 1988 regulates all human laboratory testing, regardless of location. If tests are very simple to perform or results have minimal impact on patient care, then a CLIA certificate of waiver applies. Waived tests can be performed by anyone as long as the test manufacturers’ directions are followed. Moderate and high complexity testing is generally performed by medical technologists in laboratories where detailed procedure manuals are maintained, a quality management program includes regular quality control testing and instrument calibration and preventive maintenance and lastly, participation in a proficiency testing program. Quality Control – a stabilized test material with known analyte concentrations is tested along with a run of patient samples. If the control material results are acceptable, then we have confidence that the assay system is functioning properly and the patient test results are reliable. More than one QC material with low and high analyte concentrations may be used with a patient test run to ensure test system integrity over the linear range of the system. 3 Calibration – the test instrument is tuned to recognize samples of known concentration (calibrators). If multiple calibrators are used for a particular test, the instrument stores the calibration curve and uses it to determine patient test results by interpolation or extrapolation. Calibration is done on a schedule unique to the instrument and method; it is not usually done with each patient sample run. Proficiency Testing – the lab receives 2 to 5 test samples and performs the test on each sample, then sends the results to the company providing the samples for comparison to other participants or to an industry standard. A passing score for proficiency testing is 80%. If a lab fails two consecutive proficiency test challenges for a particular analyte or a category of tests, then they must discontinue testing until they fix the assay and successfully complete repeat proficiency testing. Causes for Inaccurate Lab Test Results Random lab error – examples: tester does not follow procedure and uses variable quantities of sample or reagents, lab temperature varies day to day, reagent not brought to room temperature before use. Systematic lab error – examples: testers follow an incorrect procedure manual, samples are collected in an incompatible tube, pathologist uses outdated criteria for diagnosing biopsies. Sink testing – the tester dishonestly makes up test results and throws samples away in order to save time or sabotage medical care. Interfering substances – the sample integrity is compromised by RBC hemolysis, high bilirubin or paraproteins that interfere with spectrophotometric tests. Human anti-mouse antibodies in the patient plasma can cause tests with mouse antibody-containing reagents to have falsely elevated results. Patient’s may intentionally add interfering substances to samples, such as urine drug screens. Improper patient preparation or instruction – examples: patient not fasting when it is required, patient fails to collect all urine in a 24 hr. period. CMS (Centers for Medicare and Medicaid Services) Approved Test Panels A few groups of lab tests are recognized by CMS as panels ( also called profiles) and health care providers are reimbursed for the panel by a single payment. These panels 4 can be ordered only when each test in the panel is considered medically necessary for diagnosis and treatment. Electrolyte Panel Sodium Potassium serum or plasma Chloride Bicarbonate Basic Metabolic Panel (BMP) Sodium Potassium Chloride Bicarbonate serum or plasma Glucose BUN Creatinine Options – with or without total or ionized calcium Comprehensive Metabolic Panel (CMP) BMP plus Total protein Albumin Total bilirubin Total calcium Hepatic Function Panel Albumin Alkaline phosphatase Total bilirubin Lipid Panel serum or plasma AST ALT Alkaline phosphatase serum or plasma AST ALT Conjugated bilirubin serum or plasma Total cholesterol HDL cholesterol Triglycerides Renal Function Panel Sodium Potassium Chloride Bicarbonate BUN serum or plasma Glucose Albumin Total calcium Inorganic phosphate (HPO4) Creatinine Chemistry Tests Sodium 5 The major cation in all body fluids with predominant impact on serum osmolality. A typical reference range is 135-150 meq/L. Hyponatremia can be caused by many medical conditions with the commonalities of retention of water, salt wasting, and/or excessive antidiuretic hormone release. It is often helpful to narrow the possibilities by deciding,based on clinical exam and possibly other lab tests, whether the hyponatremia is associated with increased body fluid volume, normal fluid volume or reduced body fluid volume. Hypernatremia is often seen in conditions where fluid loss exceeds fluid intake, such as dehydration from sweating, watery diarrhea, and diabetes insipidis. Another less common cause is intake of excessive salt, such as drinking sea water or ingesting lots of salty food. Potassium This cation is much lower in concentration than sodium in the plasma; a typical reference range is 3.5 – 5.0 meq/L. Body regulatory mechanisms keep serum K within this narrow range as hypokalemia and hyperkalemia can produce dysfunction in nerve conduction and muscle contraction. Hypokalemia can be caused by salt wasting diuretics, metabolic alkalosis with renal potassium loss, diabetic ketoacidosis, adrenal gland mineralocorticoid excess and ingestion of licorice.. Hyperkalemia can be caused by impaired excretion in the urine as occurs in renal failure, mineralocorticoid deficiency and the use the certain medications, and from excessive release from body tissues as occurs in skeletal muscle necrosis and red blood cell hemolysis. If the hemolysis . hyperkalemia. Chloride The major anion in body fluids. Hypochloremia seldom occurs as an isolated electrolyte disturbance, but can be seen in severe vomiting, respiratory acidosis and metabolic alkalosis. Bicarbonate (Carbon Dioxide) A component of the bicarbonate buffer system in plasma, bicarbonate ion is the predominant form that CO2 is found in plasma. It is reduced when there is metabolic acidosis or respiratory alkalosis an and it is increased when there is respiratory acidosis, most often due to hypoventilation. Anion Gap The formula defining anion gap is serum sodium – (serum chloride + serum bicarbonate). The upper limit of normal for anion gap is typically about 11 meq./L. Conditions with excess unmeasured anions, such as lactic acidosis, diabetic ketoacidosis, alcoholic ketoacidosis, ethylene glycol poisoning and others result in an elevated anion gap. Keep in mind, however, that there is always electrical neutrality maintained in the serum, so there really is no excess in cations, only a gap based on 6 limiting the calculation to the most abundant cation and the two most abundant anions in serum. Glucose This is the major carbohydrate available for glycolytic energy metabolism. Fasting serum glucose is maintained at a steady state level by insulin secretion and to a lesser extent by glucagon. Normal fasting serum glucose should be below 100 mg./dL. Hypoglycemia is usually due to insulin excess, however transient it may be. Hyperglycemia may be transient following food intake. Sustained, fasting hyperglycemia is the hallmark of diabetes mellitus, which may be related to insufficient insulin secretion or to insulin resistance at the tissue level. The lab test for glucose is specific for glucose and does not identify other sugars that may be in excess concentration in serum or urine in patients with metabolic defects in carbohydrate metabolism. BUN Abbreviation for blood urea nitrogen. The nitrogenous waste compound measured in this test is urea and only a carried over vestige of medical laboratory science explains why we still call it BUN and not urea concentration. Since urea is excreted by the kidney, renal disease or urinary obstruction can cause an elevation in BUN, also called azotemia. Reduced blood flow to the kidneys, as in renal vascular disease or heart failure, can also cause prerenal azotemia. Since urea represents the mammalian excretion product for most organic nitrogens produced from amino acid catabolism, BUN would be expected in transiently rise when a high protein meal or a gastrointestinal hemorrhage occurs. A low serum BUN is seldom seen clinically but could occur in liver failure since the enzymes for the urea cycle are primarily hepatic. Creatinine This nitrogenous compound is formed in skeletal muscle as a catabolic product of creatine metabolism. The serum level is directly proportional to skeletal muscle mass, so most labs report gender specific reference ranges. Creatinine is excreted in the urine and at normal serum concentrations tends to be reabsorbed and secreted by renal tubular epithelial cells to the same degree, making calculation of the creatinine clearance a fairly good estimate of the glomerular filtration rate. (GFR). Calculation of a classic creatinine clearance involves a 24 hr. urine collection, so spot urine creatinine levels and estimation of the creatinine clearance using a formula using only the serum creatinine can be reported. The relatively steady formation of creatinine in muscle makes the urinary excretion rate steady, so the variability seen in serum BUN due to protein load does not exist. Serum creatinine will be increased in renal failure, but a noticeable increase requires loss of the majority of functioning nephrons. It is, therefore, not a useful test for detecting early renal disease. 7 AST and ALT (aspartate aminotransferase and alanine aminotransferase) AST is found in many body tissues but is especially rich in the liver hepatocytes, heart muscle and RBC. ALT is more hepatic specific. Both are commonly called transaminases. Elevation in the transaminases is caused by hepatocyte necrosis with release of cytoplasmic enzymes into the interstitial fluid which is then carried by lymphatics to the venous system. In the case of AST, necrosis of cardiac muscle and hemolysis of RBC could also cause an increase. A low serum AST/ALT would be seen in patients with liver failure after the initial hypertransaminasemia had dissipated. Bilirubin Bilirubin is the metabolic byproduct of heme catabolism. Heme is the oxygen carrying component of hemoglobin. Senescent red blood cells are removed in the spleen and bilirubin is created. Bilirubin is not water soluble, so it is bound to plasma proteins, largely albumin, and it is transported to the liver. Bilirubin enters hepatocytes where it is conjugated with glucuronic acid. The conjugated form of bilirubin is water soluble and it is excreted in the bile. Once in the small and large intestine, some of the conjugated bilirubin is reabsorbed and enters the bloodstream. Historic terms related to the laboratory methods for measuring unconjugated and conjugated bilirubin are indirect and direct bilirubin, respectively. The typical reference range for total serum bilirubin is 0.1 – 1.0 mg./dL. About 90% of the total serum bilirubin is unconjugated and 10% is conjugated. Hyperbilirubinemia of 2.5 or 3 mg./dL causes jaundice. Hyperbilirubinemia can be due to several disparate diseases: RBC hemolytic diseases – increased bilirubin production. Bile duct obstruction – conjugated bilirubin builds up in liver and spills over into lymphatics, which then goes to venous system. Hepatocyte conjugation ineffective – a common cause of neonatal jaundice. Alkaline Phosphatase (ALP) This enzyme is found primarily in the biliary duct lining cells of the liver and in bone osteocytes. When bile ducts are under pressure as would occur when they are obstructed, the bile duct lining cells secrete ALP which enters the venous system. Although the source of an elevated alkaline phosphatase can be determined by ordering ALP isoenzymes, it is usually fairly easy to distinguish bone from biliary diseases based on clinical information. An elevated ALP has clinical significance whereas a low value does not. Causes of elevation in alkaline phosphatase include: Biliary obstruction, small or large ducts, such as from a gallstones, pancreatic or duodenal tumors, intrahepatic masses, both primary and metastatic. Biliary atresia. Bone growth and proliferation, such as fracture healing, bone neoplasms. 8 Calcium Serum calcium concentration is tightly regulated by the secretion of parathyroid hormone (PTH). If serum calcium becomes too low, the parathyroid glands secrete PTH which stimulates osteoclasts in bone to resorb bone trabeculae and release calcium into circulation. Low calcium can cause tetany, which is sustained muscle contraction and hypercalcemia is associated with muscle weakness. About 50% of total serum calcium is bound to serum proteins and 50% is free ionized calcium, the form considered metabolically active. Lab tests for total and ionized calcium are available. Hypocalcemia can be due to: Hyperphosphatemia, as occurs in renal failure Congenital or surgical absence of the parathyroid glands. Vitamin D deficiency. Hypoalbuminemia (ionized form may remain normal, but total calcium is low) Hypercalcemia can be due to: Parathyroid gland hyperfunction (adenoma, hyperplasia, carcinoma). PTH related protein release from malignant neoplasms. Hyperparathyroidism secondary to chronic renal failure. Inorganic Phosphate The anions PO4-3, HPO4-2 and H2PO4-2 exist in serum and form the phosphate buffer system. The test for inorganic phosphate detects them all. Causes of hyperphosphatemia include: PTH deficiency; Renal failure; since ingested phosphate cannot be excreted. GI absorption of phosphate enemas. Total Protein and Albumin Hundreds of specific plasma proteins exist with functions varying from small molecule transporters, clotting factors, hormones, fibrinolytic factors, inert proteins released by somatic cells and proteins that maintain intravascular oncotic pressure. Many of them are synthesized in the liver. They are generally classified as albumin and the globulins. Albumin typically has a reference range of 3.5 – 5.0 g./dL. and as the plasma protein in the highest concentration, it provides the majority of the intravascular oncotic pressure. 9 Globulins are further classified by what bands they migrate to in a serum protein electrophoresis. Alpha-1-globulins: alpha 1 antitrypsin is the major contributer to this band. It functions as an antiprotease; protecting cells from errantly released inflammatory cell proteases. Alpha-2-globulins: two proteins make up most of this band; haptoglobin and alpha 2 macroglobulin. Haptoglobin can bind tightly to hemoglobin that abnormally could be free in the plasma to prevent it from damaging the kidneys. Alpha-2-macroglobulin, as the name implies, is a large protein that can increase in concentration to maintain oncotic pressure if serum albumin is chronically low, as it often is in renal failure associated with nephrotic syndrome. Beta globulins: three proteins make up this band: beta lipoprotein – an essential component to lipid transport and metabolism; transferrin – a transport protein that ferries iron ions absorbed in the gut to the bone marrow where they will be incorporated into hemoglobin; complement proteins, especially C3. Gammaglobulins: immunoglobulins of the IgG, IgM, IgA and IgE classes. Because of varying antibody specificities related to unique amino acid sequences in the Ig variable regions, these proteins migrate to slightly different locations on the gel and produce a broad band. Causes of hypoproteinemia: Malnutrition. Protein losses in the urine or GI tract. Liver disease – inadequate protein synthesis Causes of hyperproteinemia: Dehydration. Monoclonal gammopathy – neoplastic formation of a monoclonal immunoglobulin. Urinalysis A battery of chemical tests performed on a urine sample can provide a wealth of information about the patient’s urinary tract, kidney and metabolic functions. Dipstick chemical urinalysis is a waived CLIA test. A complete urinalysis includes a sediment analysis, which involves centrifuging about 10 ml. of urine and examining the formed elements in the urine (cells, crystals and casts) under a microscope. As a labor saving practice, many labs will not perform a sediment analysis when the urine chemical test results are normal, since it would be unusual to find significant pathology in the sediment if the chemical tests are normal. 10 Urine dipsticks have variable numbers and types of test pads on them. The standard test pads are described here and the limitations of the results are emphasized. Specific gravity The normal range is typically 1.001 to 1.030. The s.g. is increased in a concentrated urine and in urines that have iodinated radiocontrast material in them from a recent radiologic procedure. The kidney’s ability to form concentrated urine is an important function that can be lost in some renal disorders. The dipstick s.g. can be falsely elevated in highly alkaline urines. pH Normal urine pH can vary from 4 – 9. Urine pH varies widely throughout the day depending on the overall metabolic state of the patient, whether they have had a recent meal and whether they have a urinary tract infection with an organism that can metabolize urea and form ammonium compounds that can raise the urine pH. Patients with a sustained metabolic or respiratory acidosis would be expected to have an acidic urine. People with normal resting metabolic function and that are fasting should have a slightly acidic urine with a pH of 6. Blood Blood is not normally present in urine, although it may present as a contaminant in menstruating women. Blood can enter the urine at any level of the urinary tract, from the renal glomerulus to the distal end of the urethra. The dipstick reagent that detects blood relies on the peroxidase-like activity of hemoglobin. Red cells in the urine sample are lysed on the reagent pad and the released hemoglobin produces a color change. Another protein that has similar peroxidase activity is myoglobin. Myoglobin is found in high concentration in skeletal muscle. Thus, patients suffering from necrosis of skeletal muscle, also called rhabdomyolysis, may have myoglobin in their urine that will produce a false positive blood result on urine dipstick. Glucose Glucose will transiently enter the urine following a high carbohydrate meal until insulin action reduces to resting levels. Glucose in the urine of a fasting person indicates hyperglycemia. The test pad is specific for glucose; other reducing substances that might be in the urine of patients with inborn errors of carbohydrate metabolism will not be detected. Ketones Ketones are produced metabolically glucose is in short supply, such as when glycogen stores are depleted, during starvation and when insulin or insulin receptors are deficient. They include betahydroxybutyrate, acetone and _______________. 11 Betahydroxybutyrate is the most plentiful ketone produced in diabetic ketoacidosis, but the dipstick test pad is least sensitive to it, causing false negative results. Urobilinogen Bilirubin reaching the large intestine can be metabolized by gut bacteria to urobilinogen. This compound is then absorbed in the gut and some is excreted in the urine, thus a small amount of urobilinogen is normally present in urine. A complete obstruction of the biliary tract would eventually lead to no urobilinogen in the urine. Elevated bilirubin production, as in chronic hemolytic disorders, could increase urobilinogen production and excretion in urine. Urobilinogen testing in urine is little used today now that serum assays for conjugated and unconjugated bilirubin are readily available to sort out jaundice is due to biliary disease or not. Bilirubin Bilirubin is not normally present in the urine. When it is present, it is in the conjugated form and may indicate hemolysis or biliary obstruction with associated jaundice and hyperbilirubinemia. Leucocyte esterase This is a test for a neutrophil granule enzyme. A positive leucocyte esterase test in urine indicates the presence of neutrophils in the urine. Neutrophils in urine could indicate urinary tract infection, sexually transmitted diseases, kidney stones and neoplasms. Nitrite Nitrite is a surrogate marker for bacteria in the urine. Certain bacteria contain enzymes that can change nitrate to nitrite. A urinary tract infection with one of these types of organisms would produce a positive nitrite test. The test will be negative in cases of non-nitrase producing bacteria and also when frequent urination precludes accumulation of enough nitrite positive urine to be detected. 12