Epilepsy
advertisement
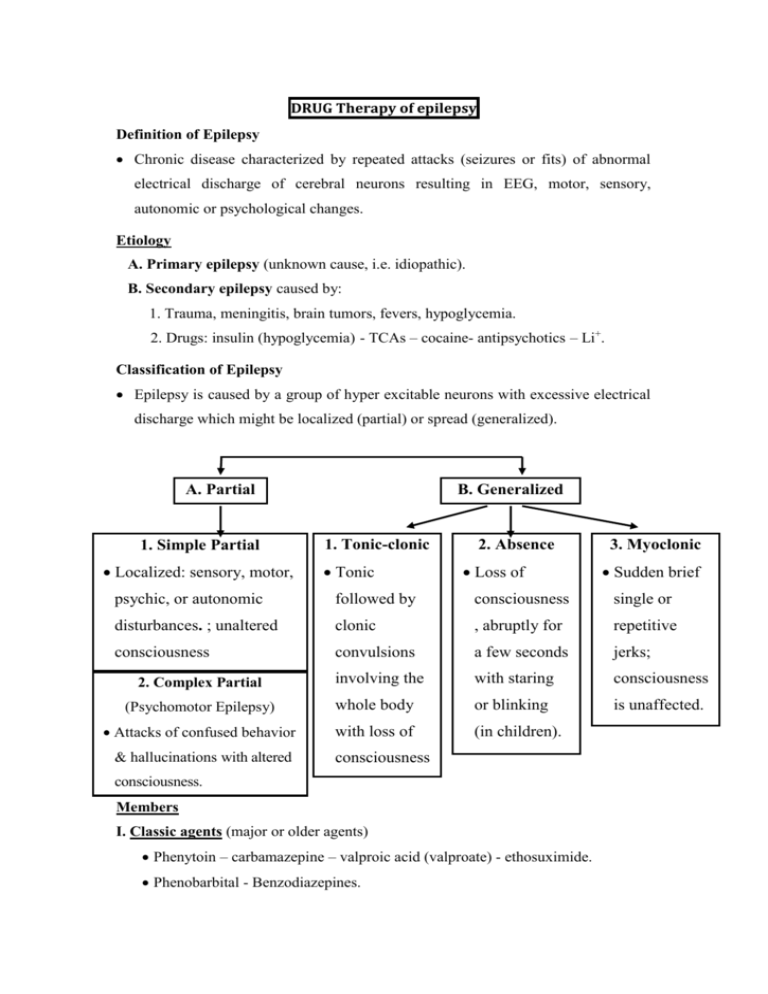
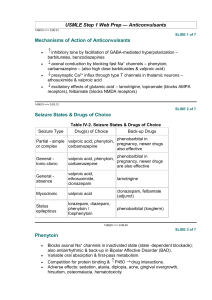
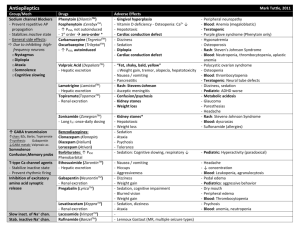
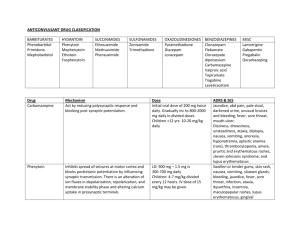
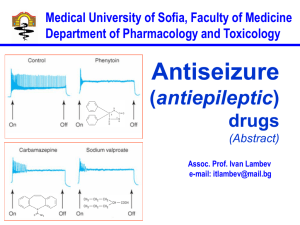
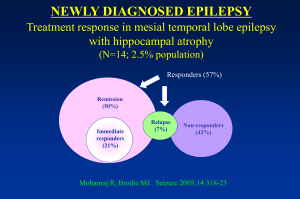
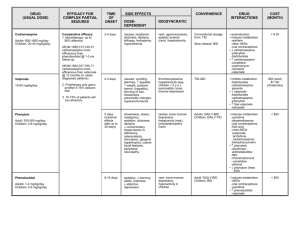
DRUG Therapy of epilepsy Definition of Epilepsy Chronic disease characterized by repeated attacks (seizures or fits) of abnormal electrical discharge of cerebral neurons resulting in EEG, motor, sensory, autonomic or psychological changes. Etiology A. Primary epilepsy (unknown cause, i.e. idiopathic). B. Secondary epilepsy caused by: 1. Trauma, meningitis, brain tumors, fevers, hypoglycemia. 2. Drugs: insulin (hypoglycemia) - TCAs – cocaine- antipsychotics – Li+. Classification of Epilepsy Epilepsy is caused by a group of hyper excitable neurons with excessive electrical discharge which might be localized (partial) or spread (generalized). A. Partial 1. Simple Partial Localized: sensory, motor, B. Generalized 1. Tonic-clonic Tonic 2. Absence Loss of 3. Myoclonic Sudden brief psychic, or autonomic followed by consciousness single or disturbances. ; unaltered clonic , abruptly for repetitive consciousness convulsions a few seconds jerks; involving the with staring consciousness (Psychomotor Epilepsy) whole body or blinking is unaffected. Attacks of confused behavior with loss of (in children). 2. Complex Partial & hallucinations with altered consciousness consciousness. Members I. Classic agents (major or older agents) Phenytoin – carbamazepine – valproic acid (valproate) - ethosuximide. Phenobarbital - Benzodiazepines. II. Newer agents Lamotrigine – topiramate - gabapentin. : felbamate, vigabatrin, pregabalin, tiagabine, zonisamide Mechanism of Action of Classic agents reducing hyper-excitability of cerebral neurons through: B. Membrane Ion Permeability A. Action on Brain Transmitters 1. Block Na+ Channels 1. Facilitate GABA Action Phenobarbital Phenytoin Benzodiazepines Carbamazepine Valproic acid 2. GABA Level 2. Block T- Ca2+ Channels (in thalamus) Valproic acid (inhibits GABA Ethosuximide. Valproic acid transaminase→ GABA breakdown) Major (classic) Antiepileptics Phenytoin Mechanism Carbamazepine Block Na channels Valproic acid Block Na channels -Block Na channels -Block Ca channels -Inhibits GABA transaminase→ GABA breakdown A: omv Ph.kinetics D:all, high ppb st M:sd(1 o)- ld(2nd o) E:U 1-Epilepsy Uses: All types except petit mal epilepsy 2-Antiarrythmic Ib 2-Mood stabiliz. in bipolar depr. 3-Trigem. Neur. Adverse effects: Hypersensitivity Skin rash stop the drug. Broadspectrum 2-Mood stabiliz. in bipolar depr. 3-Migraine GIT Disturbances Nausea - vomiting - epigastric pain (most common with valproic acid) give small dose after meals. Neurological Nystagmus, Diplopia, Diplopia, Disturbances Ataxia, Drowsiness. Ataxia, Learning in children. Drowsiness. (specially in toxic Fine hand tremors. Ataxia, Less sedative. doses) Hepatotoxicity Transient elevation of liver enzymes. Hepatotoxicity (liver function (rare but fatal). tests required). Effects on Hepatic Microsomal Enzymes (monotherapy is preferred) Hematological Effects (→regular blood picture) Teratogenicity → give folic acid Others Enzyme inducer Metabolism of other Enzyme inducer antiepileptics, warfarin Osteomalacia: vitD Metabolism Metabolism of antiepileptics & antiepileptics , other drugs. warfarin & Ca2+ supplements ). other drugs. (add folic acid supplements). of metabolism (→ vit D & Megaloblastic anemia Enzyme inhibitor Leukopenia Thrombocytopenia Agranulocytosis Lymphadenopathy Cleft palate & lip - heart Less anomalies. teratogenic. 1. Cosmetic disturbances Water Gingival hyperplasia (gum hygiene required). 1. Hair loss. 2. Appetite. dilutional 3. body weight. hyponatremia Hirsutism - acne. (potentiates ADH). level: monitor level. Ethosuximide (safest): Uses:of choice in petit mal S/E: GIT upset, skin rash, dizziness, drowsiness, headache Newer agents Neural tube defects. intoxication & Coarse facial features. 2. Unpredictable serum Spina bifida. 1. Glutamate 3. Block Na+ Channels 1- felpamate: block NMDA receptors 1- Lamotrigine (sever rash) 2- topiramate: block AMPA receptors 2- Topiramate 3-zonisamide (renal stones) 2. GABA 1-Gabapentine, pregabaline analogue increase release of GABA 2- tiagabine : decrease uptake of GABA 3- Vigabatrin: inhibit GABA transaminase...>decrease breakdown (visual defect) 4-topiramate: Uses: Refractory cases especially partial seizures + Lamotrigine: bipolar manic dis. Topiramate: migraine Gabapentine: trig.neur., postherpetic neur. Choice of Antiepileptic Drugs in Different Types of Epilepsy Partial Generalized tonic- Absence Myoclonic clonic First line Valproic acid. Valproic acid. Ethosuximide. Valproic acid. Carbamazepine Lamotrigine. Valproic acid. Topiramate. Phenytoin. Topiramate. Lamotrigine. Alternatives Topiramate. Phenytoin. Lamotrigine. Carbamazepine. Phenobarbital. Phenobarbital Clonazepam. Clonazepam. Status Epilepticus Continuous or repetitive seizures > 30 min with impaired consciousness during the interictal period. Management (drugs are given IV) 1. Lorazepam (Preferred to diazepam as its antiepileptic effect is longer & it is non irritant to veins.), midazolam or diazepam (IV or rectal) → for rapid control. 2. Fosphenytoin (soluble, prodrug, safer than pheytoin (no need for the cardiotoxic solubilizing agent propylene glycol). or phenytoin → long-acting, to maintain control. 3. Phenobarbital →2nd choice to phenytoin. 4. IV anesthesia with propofol→ in resistant cases. General Guidelines for Antiepileptic Drug Therapy 1. Proper diagnosis of type of epilepsy & prescribing appropriate drug. 2. Monotherapy is preferred since antiepileptic drugs are either enzyme inducers (phenytoin, carbamazepine & phenobarbitone) or enzyme inhibitors (valproate). Combinations could result in changes in serum level of drugs. 3. Start with a small dose & a single drug and gradually dose. If no effect, gradually substitute or add another drug. 4. Long duration of treatment: If epileptic fits are absent for 2 years, consider terminating therapy; but if fits recur, repeat treatment for another 2 years. 5. Gradual withdrawal of drugs: over six months to avoid status epilepticus or relapse. 6. Folic acid supplements: especially to women in child bearing period to ↓ risk of teratogenic defects. 7. Pregnant females should receive the lowest effective dose of the least teratogenic antiepileptic drug (e.g., carbamazepine). Pregnancy metabolism of antiepileptics adjust dose. 8. Monitoring of serum level of drugs, periodically, since a drop below therapeutic level could result in loss of seizure control while an increase in their level could result in toxicity (CNS depression stupor - coma - respiratory depression). 9. The newer antiepileptics lamotrigine & topiramate have fewer drug interactions → do not require serum monitoring.