Word - Gold Coast Primary Health Network
advertisement

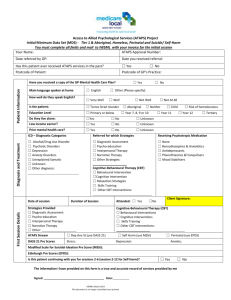
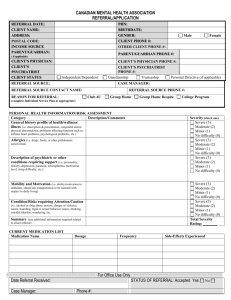
ATAPS Mental Health Referral Form Access to Allied Psychological Services Forward completed referral form together with the Mental Health Treatment Plan/Child Treatment Plan to Gold Coast Primary Health Network via Medical Objects (GCML Referrals) or Fax: 07 5612 5499 Referring GP: Phone: Practice Address: (practice stamp if available) Practice Post Code: Name of preferred ATAPS Mental Health Professional: *If MHP is not nominated GCPHN will allocate to most appropriate provider Preferred Gender of MHP: Either Male Female Referring GP Signature: Please note one referral = 6 sessions. A Patient must be reviewed by the GP before a further 6 sessions can be provided. The subsequent allocation of 6 sessions requires an ATAPS Mental Health Review form to be completed. Referral Date: Patient Name: DOB: M F Gender: Address: Postcode: Home Ph: Mobile Ph: Next of Kin/Guardian: Relationship to Patient: Patient/Parent or Guardian provides consent for this referral: Medicare No: Y N Health Care/ Pension Card No: Expiry Date: (*Must hold one of these to be eligible for ATAPS) Is the Patient a low income earner? Y N Does the Patient have Private Health Insurance? Y Date Mental Health Treatment Plan (MHTP) or Child Treatment Plan (CTP) Completed (*Must have one of these to be eligible for ATAPS) __________ /__________/___________ Does the Patient speak a language other than English? Y Does the Patient identify as Aboriginal or Torres Strait Islander? Does the Patient live on their own? Y N (* MHTP or CTP is required to accompany this referral) If yes, what language? N Very Well If yes, how well does the Patient speak English: MHTP or CTP Attached : Y N Well Not Well Not at all No Aboriginal Torres Strait Islander Both N Does the Patient have access to transport? Y N What is the highest level of education the Patient has completed? Primary Year 10 Year 11 Year 12 Tertiary Has the Patient received Better Access services this calendar year? Has the Patient received Specialist Mental Health Care before? Y N Y N OUTCOME TOOL SCORE: ATAPS Program Referred to: (select one) Aboriginal & Torres Strait Islander Mental Health Service Child ATAPS (12 years and under) General ATAPS (Anxiety/Depression) Perinatal Depression If Postnatal - Infant DOB: K5 Score: SDQ Score: K10 Score: EPDS Score: (up to 1 year of age to be eligible for ATAPS Perinatal Program) Suicide Prevention (non acute/non crisis) MSSI Score: Suicide Prevention Referrals ONLY Please select rating category for each issue or attach Mental Health Service Acute Care Team, discharge summary. Issue Suicide / Self Harm History Intent / Plan / Thoughts Longstanding Problems Psychological Factors Lack of strengths / Support Overall Assessment of Risk High High High High High High / / / / / / Risk Categories Moderate / Low Moderate / Low Moderate / Low Moderate / Low Moderate / Low Moderate / Low Please note: If majority of Risk Categories are rated High Acute Care Team referral may be more appropriate. V1.0 09/07/2015 Diagnosis/Presenting Complaint (please specify below) Adjustment Disorder Depression Eating Disorder Neurasthenia Sexual Disorders No formal diagnosis Anxiety Disorders Dissociative Disorder Enuresis Psychotic Disorders Unexplained Somatic Disorder Other: Conduct Disorder Drug & Alcohol / Substance Abuse Hyperkinetic Disorder Sleep Problems Unknown If a child is ‘at risk of’ developing any of the above, please explain under the ‘Presenting Issues’ below. Referred for which Focused Psychological Strategies: (please specify below) Diagnostic Assessment Cognitive Intervention (CBT) Skills Training (CBT) Narrative Therapy Psycho-Education Interpersonal Therapy Behavioural Intervention (CBT) Relaxation Strategies (CBT) Other CBT Intervention Parent Training in Behaviour Management (Child ATAPS Referral Only) Is the Patient receiving Psychotropic Medication? If yes, please indicate below: Benzodiazepines and Anxiolytics Phenothiazines and Major Tranquillisers Y N Antidepressants Mood Stabilisers Presenting issues are mild to moderate in severity? Y N Patient requires short-term psychological intervention? Y N Presenting Issues: Patient History: (Medical, Surgical, Social & Family) Treatment Goals: V1.0 09/07/2015 Suicide Prevention Program Risk Assessment (Circle Issue or Example of Issue): Issue Examples of High Rating Examples of Medium Rating Suicide/Self-Harm History; Family History of suicide; Multiple attempts of low lethality; Previous attempts or exposure to Previous attempt of high attempts lethality; Repeated threats; Lethality Repeated self-harm. Infrequent self-harm; Examples of Low Rating Nil or vague thoughts; No recent attempt of low lethality and low intentionality Recent attempt of moderate lethality. Long standing problems; History of mental illness History of sexual/physical abuse/neglect/domestic violence Family breakdown, child custody issues Financial difficulties, unemployment, homeless Serious physical illness/ disability Chronic pain or illness Intent/Plan/Thoughts; Access to means Clear plan Evidence of clear intention Suicidal Thoughts Psychological factors; Depression/hopelessness/ isolation/anger; Psychotic symptoms; Stressors in last 6 months (eg. Recent crisis, major loss or trauma, or anniversary) Several factors in this list are involved Some factors in this list are involved Nil or one factor in this list are involved Continual/specific thoughts; Frequent thoughts; Nil or vague thoughts; Evidence of clear intention; A plan that is not fully developed; No real plan; Access to means; A well-developed plan Moderate depression; Nil or mild depression; Command hallucinations or delusions about dying; Some sadness; Nil or mild sadness; Some symptoms of psychosis; No psychotic symptoms; Preoccupied with hopelessness, despair, feelings of worthlessness; High level of stressors in last 6 months. Unemployed; Lack of supportive and stable relationships / hostile relationships; Others not available or unwilling / unable to help. Overall Assessment of Risk; Clinical judgement based on the ratings for the Issues listed above. Ambivalent desire to end their life Severe depression; Severe anger, hostility; Lack of Strength & Supports; Availability of supports Stability of employment and Relationships No intention to end their life Potential access to means; Most of the Issues above rate in the High Category Some feelings of hopelessness; Moderate anger, hostility; Moderate level of stressors in last 6 months Employment either unstable or unsatisfying; Few relationships lacking stability; Feels hopeful about the future; Nil/mild anger, hostility; Nil or mild stressors in the last 6 months. Stable satisfying employment/study; Stable relationship/s; Others available but unwilling / unable to help consistently. Support from others that are willing and able to help consistently. Most of the Issues above rate in the Moderate category. Most of the Issues above rate in the Low category. Acute Care Team referral may be more appropriate V1.0 09/07/2015