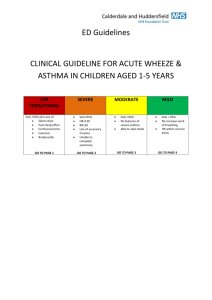
clinical guideline for acute wheeze & asthma in children aged 1
advertisement

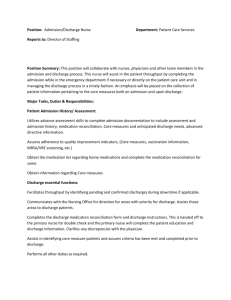
ED Guidelines CLINICAL GUIDELINE FOR ACUTE WHEEZE & ASTHMA IN CHILDREN AGED OVER 5 YEARS LIFE THREATENING Sats <92% plus any of PEFR<33% best/predicted Silent chest Poor Resp effort Confusion/coma Cyanosis Bradycardia GO TO PAGE 1 SEVERE Sats<92% PEFR<50% best/predicted HR>120 RR>30 Use of accessory muscles Unable to complete sentences GO TO PAGE 2 MODERATE Sats >92% PEFR 50-75% best/predicted No features of severe asthma MILD GO TO PAGE 3 Sats > 95% PEFR >75% best/predicted No increase work of breathing HR within normal limits GO TO PAGE 4 LIFE THREATENING ASTHMA Obtain senior Emergency Department help & paediatric registrar immediately (consider anaesthetist). Patient must be managed in Resuscitation Area. AIRWAY & BREATHING 1. 2. 3. 4. Check airway Give high flow oxygen with non re-breath mask Give Salbutamol nebuliser 5mg Give Ipratropium nebuliser 0.25mg IV ACCESS 1. Insert appropriately sized IV cannula 2. Obtain samples for FBC, U&E, glucose & Venous gas 3. Give IV hydrocortisone 4mg/kg OBSERVATIONS PAWS should be calculated and documented every 15 minutes CONTINUING MEDICATION 1. Continue nebulised Salbutamol every 20-30mins FURTHER SUPPORT Discuss case with Paediatric and Anaesthetic middle grades regarding: 1. IV Salbutamol infusion 1-5 micrograms/kg/min 2. Aminophylline infusion 1mg/kg (preceded by loading dose if not already taking theophyllines) 3. Magnesium sulphate infusion 40mg/kg (max 2g) over 20 mins ADMISSION/DISCHARGE All children that present to Accident and Emergency with life-threatening asthma need admission for a period of observation/treatment. 1 SEVERE ASTHMA AIRWAY & BREATHING 1. 2. 3. 4. 5. 6. Check airway Give O2 via face mask to maintain oxygen saturations above 95% Give Salbutamol nebuliser 2.5mg Give Ipratropium nebuliser 250 micrograms Give oral prednisalone 2mg/kg Consider repeating nebuliser CONTINUING MEDICATION 1. Continue nebulised bronchodilators every 20-30mins. OBSERVATIONS PAWS should be calculated and documented every 15 minutes. ADMISSION/DISCHARGE All children that present to Accident and Emergency with severe asthma need admission for a period of observation/treatment. 2 MODERATE ASTHMA AIRWAY & BREATHING 1. Check airway 2. Give oxygen via facemask to maintain SaO2 above 95% 3. Give Salbutamol inhaler 10 puffs via a spacer CONTINUING MEDICATION 1. Repeat Salbutamol 4-10 puffs via a spacer after 30 mins in no improvement 2. Give oral prednisalone 2mg/kg OBSERVATIONS PAWS should be calculated and documented every 30 minutes ADMISSION/DISCHARGE If continues to have raised RR or increased work of breathing arrange admission. If condition worsens, then reassess looking for features of life threatening and follow appropriate guidance. Consider discharge if HR & RR normal, no increased work of breathing, Oxygen Sats>95% on air and fulfils all criteria of discharge plan Have a low threshold for admission if there are any social concerns 3 MILD ASTHMA INITIAL MANGEMENT 1. Give Salbutamol 4-6 puffs via spacer CONTINUING MEDICATION 1. Continue inhaled bronchodilators every 20-30mins. OBSERVATIONS PAWS should be calculated and documented every 30 minutes If continues to have raised RR or increased work of breathing arrange admission. If condition worsens, then reassess looking for features of life threatening Consider discharge if HR & RR normal, no increased work of breathing, Oxygen Sats>95% on air and fulfils all criteria of discharge plan ADMISSION/DISCHARGE If continues to have raised RR or increased work of breathing arrange admission. If condition worsens, then reassess looking for features of life threatening and follow appropriate guidance. Consider discharge if HR & RR normal, no increased work of breathing, Oxygen Sats>95% on air and fulfils all criteria of discharge plan (page 5 of this document) Have a low threshold for admission if there are any social concerns 4 DISCHARGE PLAN BEFORE DISCHARGE CONSIDER 1. The patient must be stable, have a heart rate within normal limits for their age, have no recessions or use of accessory muscles. 2. Any patient with signs of life threatening or severe asthma at any time MUST BE ADMITTED 3. Children must be observed for at least 2 hours after a nebuliser (including those given by the paramedics) has been given before discharge can be considered. If the patient is going to breach the child needs to be admitted to complete this period of observation 4. If a patient presented with intercostal recessions that has settled at the time of discharge consider discharge on oral prednisalone 10-20mg for 5 days 5. If a patient has re-attended within 6 hours a period of extended observation must be considered CONSIDER REFFERAL FOR ADMISSION/PAU REVIEW IF ANY OF THE FOLLOWING 1. 2. 3. 4. 5. 6. 7. Signs of Life threatening/severe asthma Significant co-morbidity Taking oral steroids prior to presentation History of poor compliance Previous near fatal attack / brittle asthma Psychological problems/ learning difficulties Poor social circumstances AT TIME OF DISCHARGE 1. 2. 3. 4. Check inhaler technique Ensure the patient is clear about their treatment Ensure the patient has an adequate supply of inhalers and oral medications Give the patient a copy of their treatment plan and advise them to see their GP/asthma nurse within 2 days 5. Advise the patient to seek further medical advice if there is any deterioration in their symptoms Dr Paul Jarvis, Consultant in Emergency Medicine Dr Nadeem Akhtar, Foundation Year 2 Doctor 5 February 2010