Discharge Summary: Pneumocystis Carinii Pneumonia in Teen
advertisement
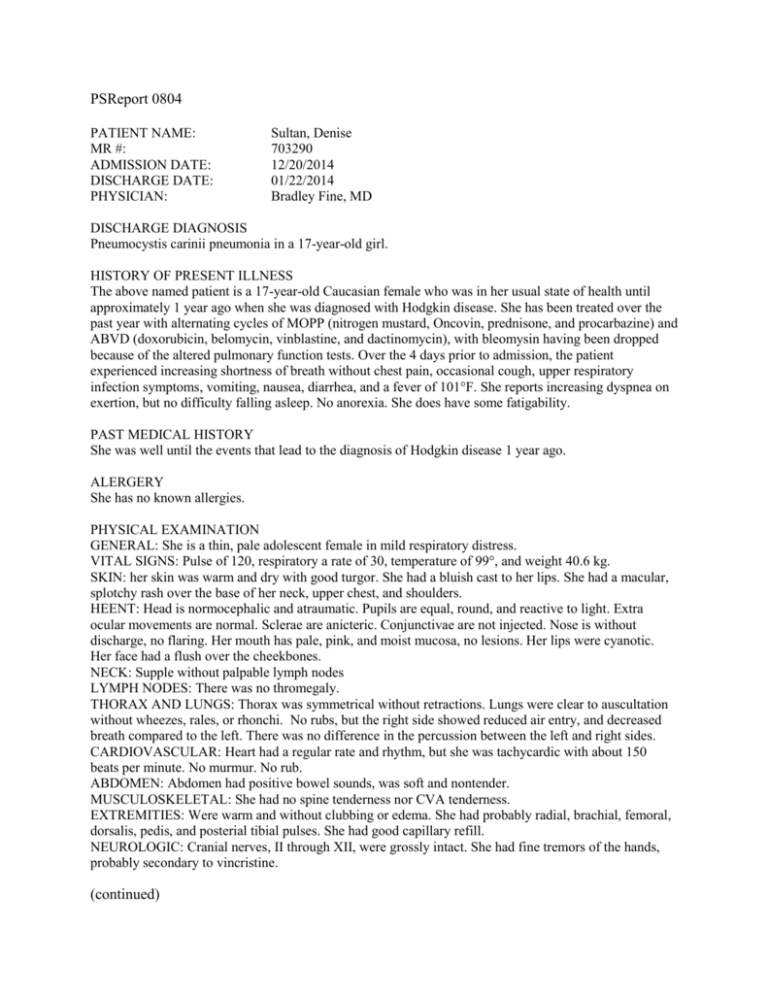
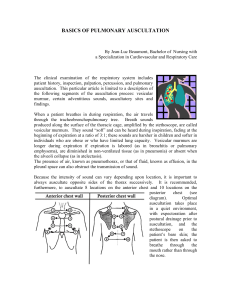
PSReport 0804 PATIENT NAME: MR #: ADMISSION DATE: DISCHARGE DATE: PHYSICIAN: Sultan, Denise 703290 12/20/2014 01/22/2014 Bradley Fine, MD DISCHARGE DIAGNOSIS Pneumocystis carinii pneumonia in a 17-year-old girl. HISTORY OF PRESENT ILLNESS The above named patient is a 17-year-old Caucasian female who was in her usual state of health until approximately 1 year ago when she was diagnosed with Hodgkin disease. She has been treated over the past year with alternating cycles of MOPP (nitrogen mustard, Oncovin, prednisone, and procarbazine) and ABVD (doxorubicin, belomycin, vinblastine, and dactinomycin), with bleomysin having been dropped because of the altered pulmonary function tests. Over the 4 days prior to admission, the patient experienced increasing shortness of breath without chest pain, occasional cough, upper respiratory infection symptoms, vomiting, nausea, diarrhea, and a fever of 101°F. She reports increasing dyspnea on exertion, but no difficulty falling asleep. No anorexia. She does have some fatigability. PAST MEDICAL HISTORY She was well until the events that lead to the diagnosis of Hodgkin disease 1 year ago. ALERGERY She has no known allergies. PHYSICAL EXAMINATION GENERAL: She is a thin, pale adolescent female in mild respiratory distress. VITAL SIGNS: Pulse of 120, respiratory a rate of 30, temperature of 99°, and weight 40.6 kg. SKIN: her skin was warm and dry with good turgor. She had a bluish cast to her lips. She had a macular, splotchy rash over the base of her neck, upper chest, and shoulders. HEENT: Head is normocephalic and atraumatic. Pupils are equal, round, and reactive to light. Extra ocular movements are normal. Sclerae are anicteric. Conjunctivae are not injected. Nose is without discharge, no flaring. Her mouth has pale, pink, and moist mucosa, no lesions. Her lips were cyanotic. Her face had a flush over the cheekbones. NECK: Supple without palpable lymph nodes LYMPH NODES: There was no thromegaly. THORAX AND LUNGS: Thorax was symmetrical without retractions. Lungs were clear to auscultation without wheezes, rales, or rhonchi. No rubs, but the right side showed reduced air entry, and decreased breath compared to the left. There was no difference in the percussion between the left and right sides. CARDIOVASCULAR: Heart had a regular rate and rhythm, but she was tachycardic with about 150 beats per minute. No murmur. No rub. ABDOMEN: Abdomen had positive bowel sounds, was soft and nontender. MUSCULOSKELETAL: She had no spine tenderness nor CVA tenderness. EXTREMITIES: Were warm and without clubbing or edema. She had probably radial, brachial, femoral, dorsalis, pedis, and posterial tibial pulses. She had good capillary refill. NEUROLOGIC: Cranial nerves, II through XII, were grossly intact. She had fine tremors of the hands, probably secondary to vincristine. (continued) DISCHARGE SUMMARY PATIENT NAME: Sultan, Denise MR #: 703290 DISCHARGE DATE: 01/22/2014 Page 2 HOSPITAL COURSE She was a thin, pale, adolescent female in moderate respiratory distress, which was increasing over the past 4 days. Blood gas in the E.R revealed a pH of 7.5, pCO2 of 31, pO2 of 35, CO2 of 24, an O2 saturation of 84.2. She was started on O2 by nasal cannula. Chest x-ray was reviewed, showing bibasilar lower lobe infiltrates. No pneumothorax but a questionable effusion on the right side. Blood culture and urinalysis were sent, and she was started on ceftazidime, 2 g t.i.d., which was 150 mg/kg/d. After admission, she was receiving 50% FIO2 via face mask, and her pulse oximetry was 98%. A CBC on admission included a white blood cell count of 8.0, hemoglobin of 11.8, hematocrit of 35.2, and 334,000 platelets; 80 segs, 2 bands, 9 lymphs, 3 monos, 5 eos, and 1 baso. She was started on Bactrim 5 mg/kg per dose divided q.6 h. for the possibility of Pneumocystis carinii pneumonia. It was decided to transfer her to the ICU because of increasing dyspnea and pain across her thorax. Bronchoscopy was done with bronchial wash and Gram stain, which was positive for PCP. She improved and became afebrile with decreasing rales. Her lungs had good air movement, but she continued to have decreased breath sounds on the right and occasional rales bilaterally. She was transferred to the adolescent floor where she continued to do well on Bactrim therapy for a 14 day course. Her Hodgkin disease remains stable throughout this hospitalization. DISCHARGE MEDICATION She was sent home on Bactrim prophylaxis, 1 double-strength tablet p.o. b.i.d. PLAN She is to be followed in Hematology-Oncology Outpatient Clinic in 3 days. ______________________________ Bradley Fine, MD BF/ps D: 01/22/2014 T: 01/25/2014