B1-U2-Diseases-Drugs
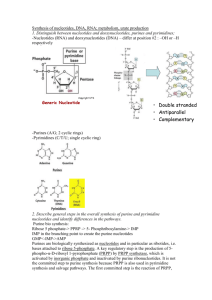
advertisement

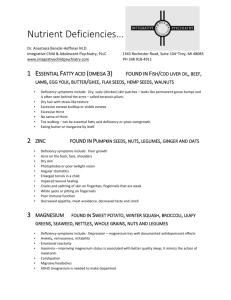
Carbohydrates: General Properties 9/4 HbAic –use glycosylated derivative of Hemoglobin to observe efficacy of treatment of Type II Diabetes HbAic levels are directly related to [glucose] in blood, b/c this is a non-enz. Rxn Glycolysis 9/5 Excess Ethanol consumption leads to: Increased fatty acid biosynthesisFatty Liver Depletion of NAD+, inhibiting Gluconeogenesis post-vigorous and in fasting state o RESULTING CONDITIONS: Lactic Acidosis & Hypoglycemia DRUGS: Antabuse (Disulfram)— Inhibits acetaldehyde dehydrogenase (DHDII) Leads to build up of Acetic acid (which is toxic) and causes user to become very ill Intended use is for pts who abuse alcohol PPP 9/6 Diagnostic Test for Thiamine Deficiency Thiamine deficiency diseases: Beri-Beri, and Wernicke-Korsakoff Syndrome Dx: Increase in erythrocyte transketolase activity observed upon addition of thiamine pyrophosphate Interconversion of Hexoses 9/9 Enzymatic Deficiencies in Fructose Enzymes Cause Disease: 1) Deficiency of phosphfructoaldolase B—Hereditary Fructose Intolerance (HFI). This causes a build-up of F-1-P which becomes toxic and can lead to hepatic failure. Tx: avoid fructose in diet 2) Deficiency of FructokinaseLeads to fructose uria (benign condition) Inability to digest fructose causes secretion in urine Enzymatic Deficiencies in Galactose Enzymes: 1) GalactosemiaDeficiency of Galactose-1-Phosphate Uridyl Transferase --Enzyme is key in metabolism of dietary galactose from milk. It produces UDP-Galactose which can form UDP-Glucose or lactose. Hereditary Autosomal Recessive Disease When the enz. is deficient you get a build up of Galactose-1-P and Galactitol which are toxic. o Galactitol is formed by reduction of Galactose by NADPH o High Levels of Galactitol can lead to cataracts (opacity in the lenses) Can see mental retardation and failure to thrive Sx: Vomiting and Diarrhea after milk consumption, as well as enlargement of the liver and jaundice Tx: Remove Galactose from diet (No milk) This is ok because if you have glucose, Epimerase can interconvert UDP-Glucose to UDP-Galactose, allowing galactose to be incorporated into galactose lipids, other metabolites and lactose Lipids 1: -Oxidation 9/5 Enzymatic deficiencies leading to disease: 1) Carnitine Palmityltransferase Deficiencies (CPT I & CPT II deficiencies) Autosomal recessive Onset: Sx triggered by exercise or fasting state SX: muscle pain, stiffness, myoglobinuria, maybe enlarged liver Tx: high CHO, low fat diet and medium chain triglycerides Pathology: myoglobinuria—need to burn fat from -ox but can’t and muscle becomes damaged why exsc and fasting are triggercan’t trans. palmityl-CoA to IMM when they run out of CHO Enlarged liver—FA are building up b/c they can’t be utilized properly 2) Med Chain Acyl-CoA Dehydrogenase Deficiency (first step of -ox) Causes termination of -ox at C12 until C6 (LC Acyl-CoA DH will perform the fx. up to C14) Frequency: 1/17,000 Onset of sx in first 2 years of life, and can cause long term disability or fatality if not txd Sx: vomiting, lethargy, coma, hypoglycemia Dx: Urine contains MCFA esters of glycine and carnitine Tx: IV Glucose, High CHO diet, avoid fasting state 3) Zellweger Syndrome Mutation in PXR1 gene product---which is a receptor found on the surface of peroxisomes o PXR1 receptor— vital for proper import of enzymes into the peroxisomes Problems: Prenatal develop. Issues Enlarged liver High levels of copper and iron in the blood Muscle/vision abnormalities Death by age 6 Lipids 2: FA Synthesis 9/6 1) Essential FA Deficiency Extremely RARE IN USAFind more in impoverished countries Causes: Infants fed EFA-deficient formula Long-term parenteral nutrition Sx: Decreased growth, skin abnormalities, impaired immune response Tx: Supplement diet with essential FA (EFA) e.g. vegetable oils Lipids 3: Triacylglycerides Lipids 4: Phospholipids, Sphingolipids, and Arachidonic Acids 9/12 I. DISEASES 1) Respiratory Distress Syndrome Due to lack of Dipalmitoyl-Phosphatidylcholine—maj. Comp. of lung surfactant This phosphatidyl choline is not formed until late stages of gestation In premature infants see RDS due to lack of surfactant and collapsing of alveoli Tx: Synthetic Surfactant allows opening of alveoli for O2 exchange in lungs Partial Liquid Ventilation allows filling of alveoli with fluid to open them and subsequent O2 exchange via the added liquid Diseases due to lack of Specific Enzymes: 1) Tay-Sachs Disease – Autosomal recessive Defect in -N-Acetylhexosaminidase (Hexosaminidase A) o Normally degrades gangliosides that end with GalNAc (Ceramide—GalNAc) Lysosomes in neurons become filled with lipidscauses neuron degradation Sx: early neurological deterioration, blindness, deafness, paralysis, death by age 3 Tx: NO TREATMENT currently exists, but you can perform a prenatal test (hexA) Note: GalNac comes from N-Acetylneuraminate found in gangliosides 2) Gaucher’s Disease Defect in Glucocerbrosidase/ -Glucosidase Accumulation of glucocerebroside (Ceramide—Glu) 3 Types of Gaucher’s disease due to different isoforms of enzyme by tissue (2 and 3 are RARE) Type I: Affects Hematopoetic Organs Sx: varied onset with easy bruising, fatigue (anemia), enlargement of liver and spleen, skeletal weakness, occasional lung and kidney impairment Tx: IV Enzyme replacement therapy (Ceradase, Cerezyme)since it can easily traverse cell membrane Type II: Most severe Affects Brainearly onset with severe brain damage Tx: NONENo IV enz. replacement because enzyme can’t easily pass through blood-brain barrier Note: Glucocerebroside is just cerebroside (glycosphyngolipid) 3) Niemann-Pick Disease (Type A) – Autosomal Recessive Deficiency of Sphingomyelinase Accumulation of Sphingomyelin (Ceramide—P—Choline) o in nuerons, and foamy reticuloendothelial cells in liver, spleen, bone marrow and other tissues Sx: Enlarged liver and spleen, mental retardation, anemia, neurological and physical deterioration Onset: during early infancyDeath before age 3 II. DRUGS: 1) Aspirin Permanent modification and inactivation of COX 1 and COX 2 Acetylation of Ser residue Inhibits formation of prostaglandins o Decrease inflammation and fever Inhibits formation of TXA2 –stimulator of platelet aggregation = Dec. Aggregation/clotting 2) Ibuprofen (Advil and Motrin) Blocks active site of cyclooxygenase (hydrophobic channel where arachidonate enters) Inactivates COX 1 and COX 2 Inhibits formation of prostaglandins o Decrease inflammation and fever Inhibits formation of TXA2 –stimulator of platelet aggregation = Dec. Aggregation/clotting 3) Acetaminophen (Tylenol) Inhibits Prostaglandin H2 Synthase (COX 3) reversibly Fx is mainly centralDecreased fever and reduced pain threshold NO peripheral effects –NO anti-inflammatory or anti-clotting effectsOK pre-surgery TOXIC in large quantities—when liver detoxifies, induces enz. that converts acetaminophen to toxic derivatives (Acetaminophen itself is not toxic) NOTE: COX 1 helps maintain normal body fx, while COX 2 is induced with inflammation When both COX 1&2 blocked: see neg side effects—upset stomach, bleeding, kidney damage New NSAIDS: (celebrex)—only block COX2causes unanticipated side effects… Nucleotide Metabolism 9/9 Antimetabolite Blocking of Nuc Metabolism 1) Glutamine Analogs (Azaserine)—Inhibit Amidotransferases Used as antineoplastic agentPrevent RNA and DNA synthesis, prevent proliferation PURINES: Inhibit PRPP Glutamyl Amidotransferase o Made up of 2 enzymes: amidophsphoribosyl transferase and poshphribosyl-formyl glycine amidine synthetase PYRIMIDINES: Inhibit CTP Synthetase (convert UTP CTP), uses glutamine as amino donor 2) 5-Fluorouracil (5-FU)—Uracil Monophosphate analong in a sense Used as treatment for solid tumors 5-FU converted in cell to FdUMP=Irreversible Inhibitor at active site Inhibits TMP formation via Thymidylate Synthase inactivation 3) Purine Nucleotide Analogs Mercaptopurine—converted to ribonucleotides Inhibit PRPP Glutamyl Amidotransferase 4) Sulfa Drugs Inhibit Folate Synthesis in bacteria Substitute for p-aminobenzoic acid in the rxn of dihydropteroate synthase 5) Antifolates: Methotrexate and Aminopterin Inhibit Dihydrofolate Reductase (DHFR)depletion of THF Purine Synth: Steps 4 and 10 Pyrimidine Synth: Formation of dTMP from dUMP 6) DPD Deficiency (dihydropyrimidine dehydrogenase from catabolism of Uracil and Thymine) Severe cases can cause develop. Delay and seizures Mild cases are fairly common, 3-8% and cause hypersensitivity to chemotherapeutic agent 5-FU o 5-FU has a prolonged half life in these patients and can be fatalprolonged blockage of TMP synthesis 7) Excessive -Aminoisobutyrate urine concentrations are indicative of excessive DNA breakdown in cancer and chemotherapy This is produced exclusively in degradation of thymine 8) Gout Genetic Causes: PRPP Synthetase—mutant form—Deregulated= Increased PRPP and Nucleotide production HGPRTase Deficiency—for purine salvage pathway o decreased salvaging = increased synthesis o reduced levels of GMP and IMP reduce feedback inhibition o PRPP that is normally used for salvage rxns is now used for de novo purine synth. Glucose-6-Phosphatase Deficiency—Von Gierke’s Diseaseglycogen storage disease o Metabolic derangements caused increased synthesis and dec. excretion of uric acid! Tx: Allopurinol—inhibits Xanthine Oxidase—Forms alloxanthine (suicide inhibitor at active site) o Blocks urate production in the first place Uricosurics (Probenecid)—increase renal clearance, inhibit reabsorption Anti-Inflammatory agents—(Colchicine, NSAIDs) o Cause reduced inflammation in joints by inhibiting microtubule assembly in leukocytes 9) Lesch Nyan Syndrome HGPRTase AbsenceSee increased uric acid Sx: neurological problems including self-mutilation and mental retardation **BRAIN relies on salvage pathways for nucleotides, w/o HGPRTase brain is deprived of hypoxanthine and guanine Tx: Allopurinol will resolve hyperuricemia, but nothing exists for the neurological symptoms 10) Orotic Aciduria UMP Synthase (Defect in gene encoding this enz): OMP-Pyrophosphorylase, OMPDecarboxylase UMP Synthase leads to formation of all pyrimidine nucleotides for DNA and RNA Synth. Block in pathway leads to def. of UTP for feedback inhibition, flux through first steps of pathway incrasesinc. synth and accumulation of orotic acid Sx: megaloblastic anemia, growth retardation, excess orotic acid in urine Tx: Oral Uridine Uridine(kinase)UMPUDPUTP, which inhibits CPSII and down reg. pathway C and T nucleotides can now form from Uridine Nucleotides 11) Xanthinuria Xanthine Oxidase deficiency—used in catabolism of nucleotides Increased secretion of xanthine and hypoxanthine, Decreased in end product: Uric acid May lead to Xanthine Lithiasis Kidney Stones 12) SCID – Severe Combined Immunodeficiency Syndrome 1. Due to Adenosine Deaminase Deficiency Causes deficit of BOTH B and T cells Get decreased salvaging of Adenine, and thus increased production of PRPP and increased nucleotide synthesis (normally Deoxyadenosinedexoyinosine via ADA) In ADA Def.--> Deoxyadenosine is phosphorylated by kinases to form dATP o see build up of dATP which causes SCID Excess dATP inhibits Ribonucleotide Reductase (at activity site) an inhibits DNA synthesis in developing immune cells 2. Due to Purine Nucleoside Phosphorylase deficiency (part of Purine catabolism pathway) Causes deficit of T Cells, B cells are normal May be due to build up of dGTP dGTP can inhibit reduction of pyrimidine ribonucleotides via ribonucleoside reducatse, thereby blocking DNA synthesis dGTP works at substrate specificity site of ribonucleoside reductase