Kidney
advertisement

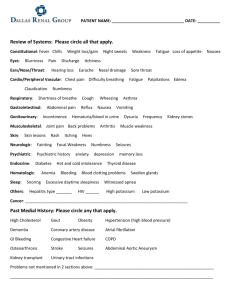
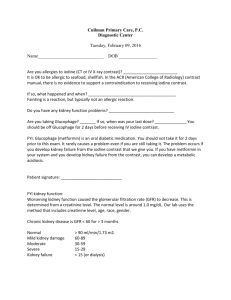
The kidney The kidney is a very important organ and is highly involved in homeostasis. The kidney processes the plasma portion of the blood and ensure that substances that need to be excreted are (e.g. urea) and also , it reabsorbs substances which are needed by the body(e.g. glucose). The kidney lies at the back of the abdominal wall-but not in the abdominal cavity. It is often described as being retroperitoneal. This means that it lies at the peritoneum, the lining of the abdominal cavity. A normal person normally has two kidney but it is also possible to just live with one kidney. A person often doesn’t know that they live with one kidney for their entire life unless a kidney disease occurs. The functions of the kidney There are many functions of the kidney. These include:1. The excretion of nitrogenous waste e.g. urea, uric acid, creatinine, even ammonia. These are called nitrogenous wastes because they contain the element nitrogen 2. The control of pH 3. The control of ionic concentration( sometimes called the electrolyte concentration) 4. The control of blood pressure( Hydrostatic pressure) 5. Gluconeogenesis 6. The water potential of the blood 7. Has an endocrine function- secretes hormones into the blood. The anatomy of the kidney The kidney lies embedded in fat. This acts to insulate the kidney. It also has a fibrous capsule – made out collagen. This fibrous capsule protects the kidney from damage. This image below shows a longitudinal section of the kidney. Pelvis: this is where the (medullary) collecting duct collect with the urine. Ureter Branch the renal artery Branch of the renal by vein Cortex: this contains the glomerulus , bowman’s( renal capsule) , the PCT and DCT. The pyramids of the kidney: this is the medulla of the kidney and contains the loops of henle and the collecting duct The nephron The nephron is the smallest unit of the kidney. It’s often described as being the functional unit of the kidney as this is the structure that performs the entire functions of the kidney. The nephron is also sometimes referred to as a kidney tubule. The majority of the kidney tubules are cortical. This means that their loops of henle doesn’t plunge down deep into the medulla. The minority of the kidney tubules are juxtamedullary. This means that their loops of henle do plunge deep down into the medulla. This is responsible for the dilution of H2o( so it can be reabsorbed in the collecting duct) . Also ion reabsorption in the medulla of the kidney. This places an important role in creation of a hypertonic(hyperosmotic) region in the medulla. This hence allows water reabsorption via an osmotic gradient, down its water potential. The image shown below shows an image of a simplified kidney tubule. Glomerulus( a Afferent (vessel/ arteriole)knot of this isn’t an artery but an interconnected arteriole capillary loops) Bowman’s (renal) capsule Proximal convoluted tubule(PCT) Distal convoluted tubule( DCT) Efferent (vessel/arteriole) Collecting duct Capillaries( where substances being reabsorbed enter) Loop of henle( Henle is a person’s name and the e has an accent mark. Kidney processes The kidney performs these tasks many times during each days ensuring homeostasis is met accordingly:1. 2. 3. 4. 5. 6. Ultrafiltration/ glomerular filtration/ filtration Selective reabsorption/ reabsorption Secretion Creation of a hypertonic region in the medulla of the kidney Control of pH in the DCT Water reabsorption in the descending limb and collecting ducts. Ultrafiltration This occurs in the renal corpuscle( glomerulus and the bowman’s capsule) of the kidney tubule. This is where the plasma portion of the blood enters the kidney tubule. This process is effectively inefficient as 20% of the plasma enters the kidney tubule at any point. However, this is backed up by secretion. There are many reasons why ultrafiltration occurs for. These are collectively known as starling forces. These are: 1. The water potential of the fluid in the bowman’s capsule (glomerular filtrate)-actually zero 2. The water potential of the blood in the glomerulus. 3. The hydrostatic pressure ( blood pressure) in the glomerulus 4. The hydrostatic pressure in the bowman’s capsule In summary, the plasma is able to pass through to the bowman’s capsule because of the net glomerular filtration pressure. This is always positive under normal physiological control, however is due to change at any point- mainly due to a fall in blood pressure. Explanation:The hydrostatic pressure in the afferent vessel is higher than the pressure of the bowman’s capsule. Also, the efferent vessel diameter is smaller than the afferent vessel, increasing the pressure inside the glomerulus even more. So ,effectively the bowman’s capsule would be filled with plasma, down a pressure gradient. However, this doesn’t happen. This is because of the water potential of the glomerulus is low. This is because of the basement membrane acting as a filter and preventing plasma proteins, blood cells out. This lowers the water potential drastically and so is favouring back water by an osmotic gradient, so letting ions follow on down their concentration gradient. But the hydrostatic pressure , as nearly always, in capillaries is the greater force and so facilitating the filtration. Other factors which enhance this filtration is the leakiness of the capillaries. These capillaries have large fenestrations (gaps) which means that it allows substances out from the blood easily. Also the podocytes( the lining of the inside of the bowman’s capsule- epithelial tissue) reduces the resistance to flow by it long foot processes- often called the foot process. The fluid that enters the bowman’s capsule is now known as glomerular filtrate/ filtrate. Selective reabsorption The main role of the PCT is to reabsorb substances which are needed by the body e.g. glucose. The cells lining the PCT, cuboidal epithelial cells, are highly adapted to the reabsorption by using a mixture of facilitated diffusion and active transport. The initial problem is that the concentrations of substances are the same as in the opposite side of the cuboidal epithelium. But this problem is solved the (primary) active transport of sodium ions and potassium ions in the basolateral membranes of these cells. The sodium ions are pumped into the cell and potassium ions are pumped outside the cell coupling this to the ATP hydrolysis. So this pumps are called Na+ and k+ ATPase/ Na+ and k+ pumps. So reabsorption is an active process. This image shows the cells lining the PCT Process These cells are highly adaptable at removing substances from the glomerular filtrate. This is because the luminal membrane( the one facing the tubular lumen) has many microvilli. This increases the surface area so that more proteins can become embedded onto the membranes and facilitate in the reabsorption process. The sodium ion /potassium ion pump in the basolateral membranes set up a concentration gradient where the Na+ concentration is relatively higher inside the cell rather than in the lumen of the tubule. This, therefore allows reabsorption of Na+ by facilitated diffusion. However, this can be only made possible if Na+ is attached to another molecule e.g. glucose. So there is no way of reabsorbing Na+ without attaching the ion to another molecule. The proteins which allow this transport are co-transporter proteins ( also called symporters- transport substances in the same direction). So , the energy released when Na+ is reabsorbed is used to reabsorb other substances against a concentration gradient so no ATP is needed as energy is released by Na+ reabsorption. This is essentially the way in which all molecules are reabsorbed like amino acids and other organic molecules. So the other molecules are absorbed by indirect/ secondary active transport.From all of this reabsorption , you will get an osmotic gradient- so water is reabsorbed by osmosis down a water potential gradient through water channel proteins called aquaporins. So, this increases the urea concentration as water isn’t dissolving it- so urea is reabsorbed by simple/ passive diffusion through the tight junctions between the cells. After this has all occurred, about 65% of water and all the glucose, amino acids etc that are important to the body are reabsorbed and most of the sodium ions will have been reabsorbed. The concept of renal threshold Sometimes, all substances cannot be reabsorbed. This is due that are many molecules present that can be reabsorbed. This means that the substances will start to enter in the urine. This normally isn’t the case. For example, glucose isn’t normally present in the urine, however, if glucose starts to appear in the urine, it has gone above It’s renal threshold as it can’t be reabsorbed. The protein carriers are filled completely. This normally happens in uncontrolled diabetes mellitus . The role of the loop of henle in the reabsorption of water The loop of henle lies deep in the medulla in most cases. This is responsible for reabsorbing ions( sodium and chloride ions) into the medulla. This creates a hypertonic region in the medulla of the kidney ( the interstitial fluid – essentially tissue fluid). This then allows water to be reabsorbed in the collecting duct. That is if the duct is permeable under the influence of a peptide hormone called anti-diuretic hormone (ADH). Sometimes known as vasopressin. The way in which the loop of henle creates the hypertonic region is called the counter-current system/ hairpin counter-current multiplier. The process Vasa recta: capillary Harpin bit The glomerular filtrate is at normal isotonicity when it enters the descending limb- i.e. the solution is isotonic with blood and so enters at 300 milliOsmolar( mOsm). mOsm is a unit that measures the ionic concentration of a particular substance – the higher the value, the more ions it contains. The ascending limb pumps sodium, potassium ions against a concentration gradient using ATP. This lowers the water potential in the interstitial fluid but water can’t follow out as it is impermeable to it. However, the descending limb is permeable to water but not ions, and so water will leave into the medulla down its osmotic gradient. As glomerular filtrate is going down the descending limb, it continues to lose water until the hairpin bit. This is because as you go down deep into the medulla, it becomes even more hypertonic so water continues to go into the medulla as it is equalising osmotic imbalances. As the glomerular filtrate is going into the ascending limb- it will lose ions but not the water and so the water potential becomes higher. This is good because water can be reabsorbed in the collecting duct if water if permeable down a water potential gradient. So the loop of henle acts to firstly lower the water potential of the glomerular filtrate and then increase the water potential drastically so that water can eventually can be reabsorbed in the collecting duct. This couldn’t be achieved if there wasn’t an active transport process going on in the ascending limb and secondly if the loop of henle wasn’t associated in a “loopy” way- the glomerular filtrate flows in opposite directions( counter-current system) to maintain hypertonicity in the medulla and make the glomerular filtrate hypotonic. Furthermore, the function of the water leaving the descending limb isn’t really for reabsorption purposes but to increase the water potential back to normal as it goes back to the normal blood circulation (illustrated by the image above). The capillaries it reabsorbs it into is known as the vasa recta. This only acts to maintain the hypertonic region in the medulla of the kidney. So it is a way of ensuring that the medulla is hypertonic. Water reabsorption in the collecting duct(CD) Under normal physiological conditions, the amount of water reabsorbed and the concentration of the peptide hormone, ADH are at normal concentrations. And so not so much water is reabsorbed. However, as the water potential of the blood starts to decrease- if this isn’t detected, a lot of water will be excreted in the urine as water follows its water potential gradient. So – to prevent this from occurring, osmoreceptors in the hypothalamus will detect this change. Blood flows past these cells and a lowered water potential is thought to cause these cells to shrink and so these sensory receptors activate the neurosecretory cells. These motor neurones will carry an action potential to the synaptic bulb and cause the secretion of ADH into the blood where it will go in the systemic circulation away from the posterior pituitary gland- so the pituitary gland functions as an endocrine gland. ADH will bind to G-protein coupled receptor on the collecting duct cells (target cells) , where it will activate adenyl cyclase, so converting ATP to cyclic AMP etc. to the point you get to the insertion of aquaporins in the luminal membrane of these cells. So , therefore now you can get water reabsorption through these channel proteins, in to the medulla ,down a water potential gradient ,so resulting in smaller volume of concentrated urine. If the water potential of the blood increases, the complete reverse will occur. Physiological conditions associated with reabsorption in the CD Sometimes, reabsorption of water in the collecting duct might not go how it is supposed to. This can lead to a condition known as diabetes insipidus. This is when you are producing a lot of dilute urine as you cannot reabsorb it in the collecting duct. This is termed diuresis. The one associated in the collecting duct is called water diuresis. The causes of this vary and are usually for two reasons. One of the reasons is because of the posterior pituitary gland isn’t secreting ADH- termed central diabetes insipidus. And the other reason is because of the CD cells being unable to respond to the ADH- termed nephrogenic diabetes insipidus. Diuresis can also be caused be uncontrolled diabetes mellitus. This is because glucose becomes above its renal threshold and since glucose cannot be reabsorbed anywhere else than the PCT- it will effectively mean that the hypertonic region created in the medulla will be useless as not much water will become reabsorbed in the CD , even though if it is under the influence of ADH. But this is not water diuresis- it is caused by the solutes rather than the ADH being involved. Final result: urine has been made now after this and now collects in the pelvis of the kidney. Now the urine will go through the ureter and collect in the urinary bladder- and when ready the urine goes through the urethra and is excreted. Kidney failure Kidney failure exists when the body can no longer produce urine. This means that metabolic waste can build up in your body e.g. urea .Also, the person can no longer control the levels of water and electrolytes in the body and therefore, this can generally makes a person feel very ill as well. Kidney failure types The two types of kidney failure and they are:1. Acute kidney failure This is where the body experiences kidney failure as result of other illness already present in a person. Furthermore, this can be caused by the inflammation of the glomeruli. This is because of the damage of the basement membrane. This means that there will be a lack of ultrafiltration. This means that blood cells (like erythrocytes and leucocytes) and plasma proteins (like albumin and fibrinogen) can appear in the urine. Also because of this, the water potential of the blood plasma increases, and therefore a person can have a lot of water retention as oedema occurs (this is the swelling of tissues). Another reason why acute kidney failure may happen is because of sepsis (inflammation of blood and body tissues by bacteria) 2. Chronic Kidney failure. This is when the body develops kidney failure over a period of time. The reasons why kidney failure can be caused is because of hypertension (damage of the basement membrane), diabetes mellitus (as the PCT can‘t reabsorb all the glucose, it’s above its renal threshold), Inflammation of the glomeruli, viral infection and low blood pressure. Dialysis is the separation of molecules by means of a partially permeable membrane. There are two types:Peritoneal dialysis: This is when the peritoneal membrane is used as the partially permeable membrane. The peritoneal membrane is the tissue that lines the peritoneal cavity. The peritoneal cavity is where all the organs lie and there is a fluid which bathes these organs How it is done:A catheter (tube) is inserted into the peritoneal cavity. The dialysis fluid (dialysate) is a fluid which has the correct concentrations of urea, glucose, a.a and so on. Anything in low conc. will diffuse into the body and anything in higher conc. will diffuse into the dialysate. At the end, this dialysate will be drained. The peritoneal membrane acts like the dialysis membrane in renal dialysis machine i.e. partially permeable. It allows simple diffusion to occur and also osmosis Advantages:1) More mobile, that means that the patient doesn’t have to sit around. 2) Less expensive 3) Less of a controlled diet ( so less swings in blood volume and concentrations) as it is more often 4) Feel better as urea not allowed to accumulate so much 5) Psychologically better as patient not perceived as being seriously ill Disadvantages:1) More chances of infection as a result of a pathogen entering the catheter. 2) Less efficient so it has to be done a number of times a day. Haemodialysis:In this process, we need the use of a kidney machine.The artery and vein are sewn together to create a fistula. The blood is taken into the machine and pumped to increase pressure so it can be forced through the machine and it’s warmed to prevent any symptoms of hypothermia (because the blood will cool significantly as it goes through the machine. When it goes back into the body it will lower the core temperature. There is a partially permeable membrane which separates the blood from the dialysate. Any excess electrolytes (e.g. Na+, Cl-) are removed by simple diffusion. Any excess water is removed by osmosis. Plasma proteins and erythrocytes stay in as they are too large. The dialysate and blood moving in different directions is referred as the counter-current system. This increases the concentration gradient and prevent equilibrium to be reached. Heparin added to prevent blood from clotting. There is air detection and filter before return. Advantages of haemodialysis:1) More efficient Disadvantages of haemodialysis:1) 2) 3) 4) 5) More of a controlled diet as it is done more often More expensive More time-consuming Large swings in blood composition and volume Less free as you are stuck in a machine. Kidney transplants It’s the best way to treat kidney failure. The old kidneys are left in place unless they are likely to cause infection or are cancerous. If they are cancerous i.e. contain a malignant tumour, metastasis could occur. This means cancerous cells can break free from the tumour and spread round the body via the blood. Tumours will then develop elsewhere. There is a great importance in the donor to be of a close relative or someone that has a close tissue type. This is because the tissue type have to be otherwise there maybe organ rejection as a result of an immune response. Sometimes, there is a shortage of kidneys as result of not many people having the correct tissue type. This has led to “organs for sale” .This is because not many people in the LEDC’s have money and therefore if they patient and that particular donor are of the same tissue type, then they are likely to sell it. However, a way of solving this is by xenotransplants- that is getting an organ from an animal. This is mostly from pigs. On the other hand, there are many problems with this such as the moral or religious views. Also, the organ of a pig may carry a virus which can cause a new disease in humans.