Week 13 - papademas.net
advertisement

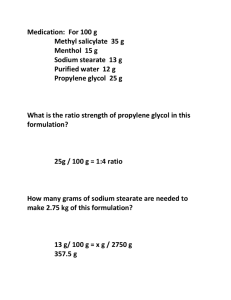
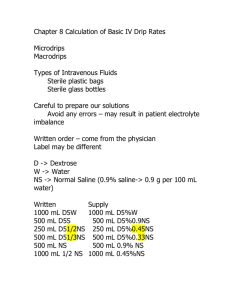
MATH 102 WEEK 04 SESSION 01 AGENDA SU 09 Professor Luke Papademas papademas@aol.com ● ● ● ● ● ● ● ● ● Welcome to MATH 102 Medical Mathematics Meet: Mondays - Thursdays 6 PM Room 2109 Meet: Wednesdays 6 PM Room 1836 ( Professor James ) Sometimes in the PC Lab Room ( Wednesday ) Avoir Du Pois Extra Credit ( consider cereal boxes and balance weights ) Online Web site: http://www.papademas.net/occ/MATH102 Final Exam on Thursday Covers up to Chapter 1 - 10 Lab Projects Wednesday ( MS Excel – calculations, MS Internet Explorer – interactive Web applications ) Review Chapter 8 ( Calculations of Basic IV Drip Rates ) Cover Chapter 9 ( Special Types of Intravenous Calculations ) Graded work tonight / tomorrow ( webcourses@aol.com ) Monday’s Deliverables include: Homework 6 and 7 Tuesday Homework 8 Thursday Homework 9 / 10 Page 210 Chapter 8 Example – Determining Hours an IV will Run ( time calculations ) Order: 500 mL NS IV ; infuse at 75 mL / hr Rule: Number of mL 500 mL ___________ = _______ Number of mL / hr 75 mL / hr = The IV will last approximately 6.7 hours. 2 / 3 hr = (2 /3) ( 60 ) = 40 minutes We could have used 6.6666 but … we use the traditional rules of rounding 6.7 hrs 6.7 = 6 + 0.7 = 6 hours + 0.7 hours = 6 hours + 0.7 * 60 minutes Page 211 Example: Order: Aminophylline 500 mg in 250 mL D5W IV at 50 mL / hr Rule: Number of mL ___________ Number of mL / hr = 250 mL ___________ 50 mL / hr = 5 hr Self – Test 2 IV Infusions - Hour 9. hr (Page 212) Calculate the hours that the IV orders will run. Order: 1000 mL NS IV 12 NOON – 6 PM Rule: we know that between 12 NOON – 6 PM = 6 hours Theoretically we would have: 1000 mL ___________ 166.67 of mL / hr = 6 hr Choosing the Infusion Set Use Microdrip when …. - IV administered over a long period a small amount of fluid is to be infused Use Macrodrip when …. - the order specifies a large amount of fluid over a short time - the microdrips per minute are too many and counting the drip rate becomes to difficult Continuous observation is necessary Adding Medications to IVs Example ( Page 213 ) Order: Available: 1000 mL D5W with 20 mEq KCL IV 10 AM – 10 PM vial of KCL 40 mEq /20 mL, microdrip ( 60 gtt / min ), macrodrip ( 20 gtt / min ) x =(D/H )*S = Formula Method x =(D/H )*S = / * ( ) x = ( 20 mEq / 40 mEq ) * 20 mL x = 10 mL Hence, we add 10 mL of KCL to the IV bag. Step 2 : Choose the tubing We know that the IV will run in 12 hours ( 10 AM – 10 PM ). 12 * 60 = 720 minutes Number of mL to infuse * TF ______________________ Number of minutes to infuse For macrodrip: 1000 mL to infuse * 20 gtt / min ______________________ 720 minutes For microdrip: = 28 gtt / min 1000 mL to infuse * 60 gtt / min ______________________ 720 minutes = 83 gtt / min Page 214 Self - Test 3 IV Infusion Rates Calculate how much medication is needed ( if applicable ) and the infusion rate. 1. Order: 500 mL D5W IV with vitamin C 500 mg of 60 mL / hr Available: ampule of vitamin C labeled 500 mg / 2 Ml ; microdrip tubing at the 60 gtt / mL Rule: 500 mL ___________ 60 mL / hr = 8.3 hr 8.3 = 498 minutes For microdrip: 500 mL to infuse * 60 gtt / min ______________________ 498 minutes = 60 gtt / min Run at: 60mL / hr which is the same as a microdrip rate; 3. Order: Aminophylline 250 mg in 250 mL D5W IV; run 50 mL / hr Available: infusion pump; vial of aminophylline labeled 500 mg / 10 mL Rule: 250 mL ___________ 50 mL / hr = 5 hr Since we have an infusion pump – the work is done for you! Page 217 Example: Order: Vancomycin 1 g IVPB 7am Supply: 500mg powder Package insert directions: 250mL (1g)/D5W Run over 2 hours (1g). Refrigerate for 7 days. Use a reconstitution device to add 1g vancomycin (two vials of 500mg) to 250mL D5W. Label the IV. Set the rate at 21 gtt/min. The IVPB will run 2 hours. mL x TF -------- = gtt/min Min 250x10 --------- = 250 20.8 = 21 gtt/min 120 12 )250.0 Use Macrodrip when …. - the order specifies a large amount of fluid over a short time - the microdrips per minute are too many and counting the drip rate becomes to difficult Self-Test #4 2. Order: Ceptaz (ceftazidime) 1g IVPB q12h Supply: 1 g powder Package directions: 50mL (1g)/D5W. Infuse in 15-30 minutes/store for 7 days (REFRIGATED) Available: macrodrip tubing at 10gtt/mL RULE: mL X TF = gtt/min min 50mL X 10 = 50 = 16.6 = 17 gtt/min 30mins 3 Example pg 219 Administer ½ strength Isocal at 60mL/hr. The total volume will equal 250 mL. For this problem, begin by taking ½ of the total volume to infuse: ½ × 250 mL = 125 mL This number tells you how much formula to add to the tube feeding bag. Next, subtract that number from the total volume. 250 mL – 125 mL = 125 mL This new number tells you how much water to add to the tube feeding bag. Now that you have diluted the formula to ½ strength, infuse it at 60mL/hr. Self Test # 5 pg 220 1. 25 % Renalcal must be prepared. 400mL is the total volume. How much Renalcal is to be mixed with how much water? .25 * 400mL = 100 mL 400 mL – 100 mL = 300 mL 100mL Renalcal. 300 mL water Self Test # 6 pg 221 6. A patient is receiving an antibiotic IVPB in 50 mL q8h to run over 1 hour plus a maintenance IV of 100 mL/hr. What is the 24 hr intake parenterally? 50 mL * 3 = 150 mL 100 mL * 21 hr = 2100 mL 2100mL + 150 mL = 2250 mL Self Test # 7 page 222 6. Order: Amikin (amikacin) 0.4 g IVPB q8h Supply: 2-mL vial labeled 250 mg/mL Package directions: 100 mL/D5W 30 minutes Available: macrodrip tubing 10 gtt/mL a. How many mL of amikacin should be added to the IV? 1 mL 250mg = x 400mg X = 1.6 mL of amikacin b. What are the gtt/min? Add 1.6 mL Amikin to 100 mL D5W TF = 10 gtt/mL for IVPB, total min: 30 mL × TF = gtt/min min 100mL × 10 = 33.3 = 33 gtt/min 30 min Label the IV. Set the rate at 33 gtt/min. Example pg 237-238 Heparin is mixed 25,000 units in 500 mL D5W. How much heparin is in 1 mL of fluid? 25000 units 500 mL = x 1 mL X= 50 units Example pg 238-239 Order: heparin, infuse 800 units/hr Available: heparin 40,000 units in 1000 mL D5W infusion pump 800 units/4000 units * (1000 mL) = 20 mL/hr How many hrs will the IV run? 1000 mL / 20 mL/hr = 50 hrs Mg/ hr Rule and Calculation Pg 240 Order: calcium gluconate 2 g in 100 mL D5W; run 0.25 g/hr IV via infusion pump. 100 mL 2g = x 0.25 g/hr X= 13 mL/hr Number of mL mL/hr 100 mL 13 mL/hr = 7.6 or approximately 8 hrs Pg 243 Order: lidocaine 2 mg/min in IV Supply: infusion pump, standard solution of 2 g in 500 mL D5W (2000 mg in500 mL) Multiply 2 mg/min × 60 = 120 mg/hr 500 mL 2000 mg = x 120 mg X= 30 mL/hr Number of mL mL/hr 500 mL 30 mL/hr = 16.6 or approximately 17 hrs m2 Rule and Calculation Page 251 Example Patient: Height 6 feet 0 inches Patient: Weight 175 lb, BSA 2.0 m2 Order: Platinol (cisplatin ) 160 mg ( 80 mg / m2 ) IV in 1 L NS with 2 mg magnesium sulfate over 2 hours The rate of infusion is 1000 mL _______ = 500 mL / hr 2 hr Self – Test 4 Use of the Nomogram 2. a) b) height 165 cm, wt: 70 kg BSA = 1.77 m 2 Order for Lomustine (CCNU) 230 mg po ( 130 mg / m 2 ) ONCE Q6 WEEKS Is this dosage correct? 1.77 * 130 mg = 230.1 mg ( which is correct) Lomustine comes in tabs of 100 mg and 10 mg. What is the dose? Administer 2 * 100 mg + 3 * 10 mg Chapter 10 pg 280 Dosage Problems for Infants and Children Dosage Based on mg/kg and Body Surface Area EX: An infant weighs 20 lbs 12 oz. Convert the ounces to pounds. Step 1. Because there are 16 oz in 1 lb, divide the 12 oz by 16. 12/16 = 0.75 Step 2. Add the answer to the pounds to get the total number of pounds. 20 + 0.75 = 20.75 lbs Self Test 1 pg 283 8. 12 lb 3 oz = 12 + (3/16) =12.19 lbs 12.19 lbs / 2.2 = 5.5 kg Example pg 283 Mg/kg Body Weight Augmentin (amoxicillin) 150 mg po q8h is ordered for a child weighing 33 lbs. Accompanying prescribing information states that children 40 40 kg receive 6.7-13.3 mg/kg q8h. We need to convert 33 lb to kg Step 1. 33 lb / 2.2 kg = 15 kg Step 2. Determine safe dose range in mg per kg. Low Dose High Dose 6.7 mg×15 kg =100.5 mg/kg 13.3 mg × 15 kg =200 mg/kg Step 3. Is the dosage safe? Yes Step 4. Calculate the dose. Label states 90 mL water should be added gradually to make a concentration of 125 mg/ 5 mL. X mL _____ 150 mg = 5 mL _____ 125 mg X= 6 mL Example pg 288 A child weighing 50 lb is ordered Phenergan (promethazine) IM 20 mg for nausea and vomiting. Is the dose safe? What amount should be given? Step 1. Convert pounds to kg 50 lb / 2.2 kg = 22.727 kg The child weighs 22.73 kg Step 2. Determine the safe dosage range. The Nursing Drug Guide states 1 mg/kg IM q4-6h prn. The safe dosage range is 10-25 mg. Step 3. The ordered dose is 20 mg. 22.73 kg * 1 mg/kg = 22.73 mg Hence, the dosage is safe! Step 4. Calculate the dose. X mL 1 mL _____ = _____ 20 mg 25 mg X= 0.8 mL (use 1 mL precision syringe) Self Test 2 pg 290 2. Order: ferrous sulfate 200 mg po tid Patient: child is 9 yrs old and weighs 30 kg Supply: bottle of 125 mg/5 mL Literature states: children 6 to 12 years old, 600 mg divided doses tid Step 1. Observe patient’s weight in kg Step 2. Check age range of child 6-12 yrs? Yes Step 3. Proper range in present Step 4. X mL 5 mL _____ = _____ 200 mg 125 mg X= 8 mL po tid 8. Order: Cloxapen (cloxacillin) 250 mg po q6h Patient: weighs 48 lbs Supply: liquid labeled 125 mg/ 5 mL Literature states for children more than 20 kg, the dose should be 250 to 500 mg q6h. Dosage is correct. X mL _____ 250mg = 5 mL _____ 125 mg X= 10 mL Steps and rule- m2 medication orders Step 1. Find the BSA in m2 Step 2. Determine the safe dose using a reference. Step 3. Decide whether the ordered dose is safe. Step 4. Calculate the dose needed. Self Test 4 pg 295 4. Child: 10 yrs; height 50 in; weight 35 kg Order: Marinol (dronabinol) po 5 mg × 1 Literature: dose 5 mg / m2 1 to 3 hours before chemotherapy Supply: 2.5 mg capsules Step 1. Find the BSA in m2 = 1.1 m2 BSA= (127 cm * 35 kg / 3600) = 1.1 m2 Step 2. Determine the safe dose using a reference. 5 mg / m2 1 to 3 hours before chemotherapy Step 3. Decide whether the ordered dose is safe. 5 mg/ 1.1 m2 = 4.55 Step 4. Calculate the dose needed. 2 capsules Steps to solving parenteral pediatric medications IVP pg 297 Step 1. Convert lb to kg. Step 2. Determine the safe dose range in mg/kg using a drug reference. Step 3. Decide whether the ordered dose is safe by comparing the order with the safe dosage range listed in the reference. Step 4. Calculate the dose needed. Step 5. Check the reference for diluent and duration for administration. Example pg 297 Child: 5 yrs, 44 lb Order: Tagamet (famotidine) 5 mg IV bid Literature: 0.25 mg/kg q12h IV up to 40 mg/day Dilute with 5 or 10 mL with 5% dextrose or 0.9% sodium chloride and injected over at least 2 minutes. Step 1. 44lb /2.2kg = 20 kg Step 2. 20 kg × 0.25 mg/kg = 5 mg Step 3. Decide whether the ordered dose is safe by comparing the order with the safe dosage range listed in the reference. Step 4. Calculate the dose needed. Step 5. Check the reference for diluent and duration for administration