Chapter 8 Calculation of Basic IV Drip Rates -...Set
advertisement

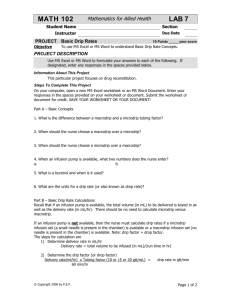
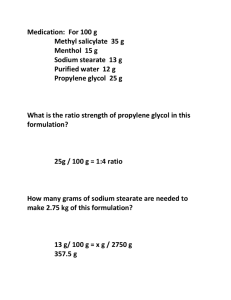
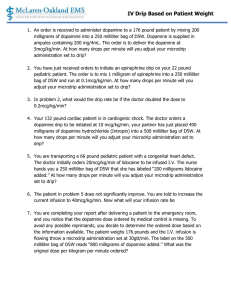
Chapter 8 Calculation of Basic IV Drip Rates Microdrips Macrodrips Types of Intravenous Fluids Sterile plastic bags Sterile glass bottles Careful to prepare our solutions Avoid any errors – may result in patient electrolyte imbalance Written order – come from the physician Label may be different D -> Dextrose W -> Water NS -> Normal Saline (0.9% saline-> 0.9 g per 100 mL water) Written Supply 1000 mL D5W 1000 mL D5%W 500 mL D5S 500 mL D5%0.9NS 250 mL D51/2NS 250 mL D5%0.45NS 500 mL D51/3NS 500 mL D5%0.33NS 500 mL NS 500 mL 0.9% NS 1000 mL 1/2 NS 1000 mL 0.45%NS Kinds of IV Drip Factors Check Infusion Set: See needle in the chamber: microdrip Deliver to the patient 1mL fluid 60 drops = 60 gtt = 1mL Infusion sets with no needle in the chamber – macrodrip Baxter-Travenol macrodrip set to deliver 10gtt/mL Abbott macrodrip set to deliver 15 gtt/mL Tubing for the above sets can be clamped (opened or closed to set the drip rate) Infusion pumps – need only two pieces of info 1) total number of milliliters 2) number of milliliters per hour (infusion rate) Can also do IVPB Order: 500 mL D5W IV Run: 50 mL/hour Primary versus Secondary IVPB Ampicillin 2 g IVPB in 100mL NS over 1 hour Labeling IVs Label such that what drip rate is and what is being infused into the patient Patient Date, Time Order Time Room Rate Run Initials Katherine Papademas 10/02, 1300 1000 mL D5W1/2NS 1300 to 0100 436B 50gtt/min 50 mL/hr DD Note: 1000 mL Run time: Finish time – start time = total hours IV runs Calculating Basic IV Drip Rates mL/hour Step 1: Total number of mLs ordered = no. mL/hr Number of hours to run Step 2: Number of mLs/hr x Tubing Drip Factor (TF) = drops per minute (gtt/min) Number of minutes Order: 1000 mL Ringer’s Lactate IV 8am-8pm Available: an infusion pump Logic: Run time: 12 hours Step 1: 1000 mL/12 hours = 83.33 (round to nearest whole number) Enter: total volume: 1000 mL mL/hr: 83 Order: 500 mL D5NS IV 12noon-4pm Available: microdrip at 60 gtt/mL; Macrodrip at 20 gtt/mL Logic Run time: 4 hr Step 1: #mL/hr = 500 mL/4hr = 125 mL/hr Step 2: Macrodrip calculation #mL/hr x TF #min = 125mL/hr x 20 gtt/mL = 41.6 gtt/min 60 min = 42 gtt/min 1 hr = 60 min Step 2: Microdrip calculation #mL/hr x TF #min = 125mL/hr x 60 gtt/mL = 125 gtt/min 60 min Which one should you choose? Use Microdrip when … IV administered over a long period of time Small amount of fluid to be infused Macrodrops per minute are too few Use Macrodrip when … Large amount of fluid is ordered in a short time Microdrips per minute are too many and counting the drip rate might be difficult for the nurse Need for continuous observation Check IV frequently Gravity Patient’s movements : kink the tube Watch the flow of the fluid with respect to where the needle has been inserted – check for infiltration Swelling Pain Coolness Pallor at the insertion site Eg. Order: 500 mL D51/3NS IV KVO for 24◦ Available: microdrip at 60 gtt/mL; macrodrip 10gtt/mL Will have to choose the IV set (as no infusion pump) Step 1: # mL/#hr = 500 mL/24 hr = 20.83 mL/hr = 21 mL/hr Step 2: Macrodrip #mL/#hr x TF = 21 mL/hr x 10 gtt/mL = 3.5 gtt/min 60 min 60 min = 4 gtt/min Step 2: Microdrip #mL/#hr x TF = 60 min 21 mL/hr x 60gtt/mL = 60 min 21 gtt/min Which do we choose????? Macrodrip 4gtt/min too slow Select microdrip infusion set Set drip rate at 21 gtt/min No. 4 on p. 203 Order: 180 mL D5 1/3NS 12 noon – 6pm Available: macrodrip (10gtt/mL); microdrip (60 gtt/mL) Step 1 180 mL/6 hr = 30 mL/hr Step 2 Macrodrip 30mL/hr x 10gtt/ml = 5 gtt/min 60 min Step 2 Microdrip 30 mL/hr x 60 gtt/mL = 60 min 30 gtt/min Choose microdrip Determining hours an IV runs Number of mLs ordered = run time (#hrs to run) Number of mLs/hr Order: 500 mL NS IV; run 75 mL/hr 500 mL = 6.66hr -> 6.7 hr 75 mL/hr Order: aminophylline 500 mg in 250 mL D5W IV at 50mL/hr 250mL = 5 hr 50 mL/hr Adding Medications to IV When continuous IV order includes medication; add medication to IV and determine rate of flow Either pharmacist or nurse will add medication Buretrol: IV delivery system with tubing and chamber (can hold 150 mL delivered as microdrip) Medications ordered over several Hours Order: 1000 mL D5W with 20 mEq KCl IV 10am-10pm Available: vial of KCl 40 mEq/20 mL, microdrip (60gtt/min), macrodrip (20 gtt/min) D xS=A H Desire: 20mEq Have: 40mEq Supply: 20 mL a) 20mEq x 20mL = 10 mL (dosage amount) 40mEq b) Calculate drip factor Step 1: #mL/#hr = 1000 mL/12 hr = 83 mL/hr Step2: Macrodrip 83 mL/hr x 20 gtt/mL = 28 gtt/min 60 min Step 2: microdrip 83 mL/hr x 60 gtt/mL = 83 gtt/min 60 min Class chose macrodrip Add 10 mL KCl to the IV bag Order: 5 milliunits penicillin G in 1000 mL D5W IV q8hr Available: macrodrip (10 gtt/mL), microdrip (60gtt/mL) Logic: Milliunit -> million units 5 milliunits -> 5000000 units of Penicillin G potassium Supply: 5-milliunits vial of powder Directions: reconstitute with 100 mL Order is safe Use a 10-mL syringe to remove fluid aseptically from 1000mL bag D5W Inject 10mL into vial containing powder – make sure all liquid!!!!!!! Inject the new supply into the bag (990 mL + 10 mL) Now that medication has been added – calc the drip factors and choose!!!! Step 1: 1000mL/8hr = 125 mL/hr Step 2: Macro 125mL/hr x 10 gtt/mL = 20.83 gtt/min =21gtt/min 60 min Micro 125mL/hr x 60gtt/mL = 125 gtt/min 60 min p. 207-208 buretrol = microdrip Order: aminophylline 250 mg in 250 mL D5W; run at 50 mL/hr Available: ampule of aminophylline 1g in 10mL; Buretrol that delivers 60 gtt/mL Logic: Ampule – 1g /1000 mL = 1000 mg/1000 mL (1) Use Formula Rule 250 mg x 10 mL =2.5 mL want to administer 1000 mg (2) Preparation: draw up 2.5 mL of drug and inject it into 250 mL D5W. Label the bag. Buretrol: microdrip 60 gtt/mL (3) Determine drip rate mL/hr x TF = 50 mL/hr x 60 gtt/min = 50 gtt/min 60 min 60 min (4) Label IV Bag: Rate, 50 mL/hr Eg. Self Test 3 – No. 3 Order: 250 mg hydrocortisone sodium succinate in 1000 mL 8AM – 12 midnight Available: vial of hydrocortisone sodium succinate labeled 250 mg with a 2mL diluent; microdrip tubing 1) determined total time 8am – 12 midnight = 16 hours 2) determine #mL/hr = run time 1000 mL/16 hours = 62.5 mL/hr -> round to 63 mL/hr 3) #mL/hr x TF = 63 mL/hr x 60 gtt/min = 63 gtt/min 60 min 60 min 4) Label IV: Medications for Intermittent Intravenous Administration IVPB q4h, q6h, or q8h = time intervals most in powder form check dr’s order (drug, route, time interval) nurse must research manufacturer’s directions for amount and type of diluent and time for infusion to run Rule to solve IVPB same as rule to solve IV #mL x TF = gtt/min #min # mL = type and amount of diluent stated on label/insert TF: tubing for IVPB-> called secondary administration set and has a macrodrip factor. Shorter than main line IV tubing – check label for Tubing drip factor #min -> if number of min not given for IVPB, then general rule: 30 minutes for every 50 mL solution for adults Eg. Order: cefazolin 1 g IVPB q6h Supply: package insert for IVPB dilution of cefazolin sodium: Reconstitute with 50 to 100 mL sodium chloride injection or other solution listed (D5W, D10W, D5LR, D5NS) Use 50 mL D5W As no time given: use 30 min for 50mL #mL x TF = gtt/min #min 50mL x 10 gtt/min = 16.6 = 17 gtt/min 30 min Use reconstitution device (sterile implement containing 2 needles that connects vial and 50 mL bag) Admixture IVs If health care pharmacy reconstitutes and prepares IVPB in a sterile environment using laminar flow hood – you as nurse still need to check for proper labeling etc. Check dose, check expiration date, etc. Changing the Intravenous drip Rate If kinking of tube, movement of patient, placement of needle/catheter, gravity affect flow – then might have to recalculate IV drip Eg. Label on IV: 1000 mL D5W IV to run 8am – 4pm Tubing is macrodrip (10gtt/mL); rate set at 20gtt/min Time now: 1pm Amount of fluid you observe left in IV bag: 600 mL Change drip? Logic Step 1: calculate #ml/hr 1000ml/8hr =125 mL/hr = delivery rate Step 2: calculate how many hours have elapsed 5 hours have elapsed 125 mL/hr x 5 hr = 625 mL should have been delivered Step 3: Make an educated decision Step 3: As 600 mL left in IV, only 400 mL were delivered (rather than the 625mL) 625 mL – 400 mL = 225 mL behind Conclude: make judgment to increase IV drip rate – call the doctor Recording intake : keep accurate account of parenteral intake as well as liquids taken orally/enterally (tube feedings)! Ex. #8. p 213 IV of D5W 1000 mL infusing at 125 mL/hr 1000mL/125 mL/hr = 8 hr #4 Order: 500 mL aminophylline 0.5g to infuse at 50 mL/hr. How mg patient receive per hour 0.5 g = 500 mg 500 mg in 500 mL -> 1mg/mL (concentration of drug) 1mg/mL x 50 mL/hr - 50 mg per hour