11 Respiratory Emergencies
advertisement
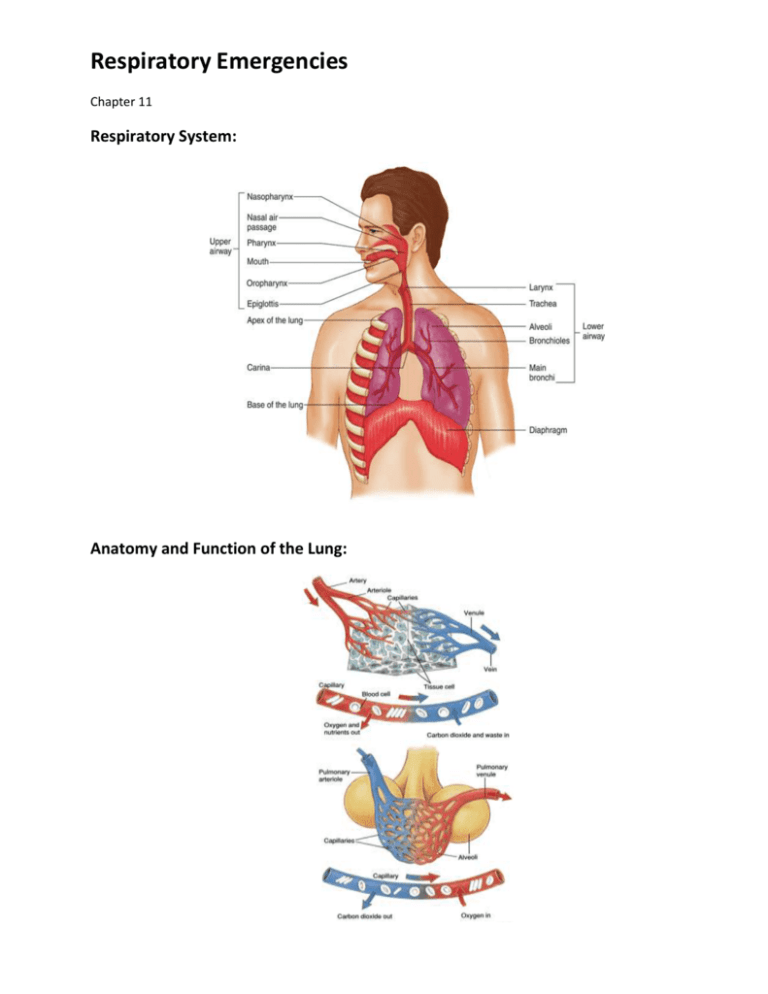
Respiratory Emergencies Chapter 11 Respiratory System: Anatomy and Function of the Lung: Characteristics of Adequate Breathing: • Normal rate and depth • Equal rise and fall of chest • Regular breathing pattern • Pink, warm, dry skin • Good breath sounds on both sides of the chest Causes of Inadequate Breathing: • Pulmonary vessels become obstructed. • Blood flow to the lungs is obstructed. • Alveoli are damaged. • Pleural space is filled. • Air passages are obstructed. • Pale or cyanotic skin • Cool, damp (clammy) skin • Shallow or irregular respirations • Pursed lips • Nasal flaring Signs of Inadequate Breathing: • Slower than 12 breaths/min or faster than 20 breaths/min • Unequal chest expansion • Decreased breath sounds • Muscle retractions Dyspnea: • Shortness of breath or difficulty breathing • Patient may not be alert enough to complain of shortness of breath. Upper or Lower Airway Infection: • Infectious diseases may affect all parts of the airway. • The problem is some form of obstruction to the air flow or the exchange of gases. Upper or Lower Airway Infection (treatment): • Administer warm, humidified oxygen. • Do not attempt to suction the airway or insert an oropharyngeal airway in a patient with suspected epiglottitis. • Transport patient in position of comfort. Acute Pulmonary Edema: • Fluid build-up in the lungs • Signs and symptoms • Dyspnea • Frothy pink sputum • History of chronic congestive heart failure • Recurrence high Acute Pulmonary Edema (treatment): • Administer 100% oxygen. • Suction secretions. • Transport in position of comfort. Chronic Obstructive Pulmonary Disease (COPD): • COPD is the result of direct lung and airway damage from repeated infections or inhalation of toxic agents. • Bronchitis and emphysema are two common types of COPD. • Abnormal breath sounds may be present. • Rhonchi and wheezes COPD Patients: • COPD patients cannot handle pulmonary infections well • Usually age 50 or older • History of recurring lung problems • Long-term smokers • Tightness in chest/constant fatigue Chronic Obstructive Pulmonary Disease(treatment): • Assist with prescribed inhaler if patient has one. • Transport promptly in position of comfort. Asthma: • Common but serious disease • Asthma is an acute spasm of the bronchioles. • Wheezing may be audible without a stethoscope. Asthma (treatment): • Obtain history. • Assess vital signs. • Assist with inhaler if patient has one. • Administer oxygen. • Transport promptly. Spontaneous Pneumothorax: • Accumulation of air in the pleural space • Caused by trauma or some medical conditions • Dyspnea and sharp chest pain on one side • Absent or decreased breath sounds on one side Spontaneous Pneumothorax (treatment): • Administer oxygen. • Transport in position of comfort. • Monitor closely. Anaphylactic Reactions: • An allergen can trigger an asthma attack. • Asthma and anaphylactic (allergic) reactions can be similar. • Hay fever is a seasonal response to allergens. Pleural Effusion: • Collection of fluid outside lung • Causes dyspnea • Caused by irritation, infection, or cancer • Decreased breath sounds over region of the chest where fluid has moved the lung away from the chest wall • Eased if patient is sitting up Pleural Effusion (treatment): • Definitive treatment is performed in a hospital. • Administer oxygen and support measures. • Transport promptly. Mechanical Obstruction of the Airway: • Be prepared to treat quickly. • Obstruction may result from the position of head, the tongue, aspiration of vomitus, or a foreign body. • Opening the airway with the head tilt-chin lift maneuver may solve the problem. Obstruction of the Airway (treatment): • Clear airway. • Administer oxygen. • Transport promptly. Pulmonary Embolism: • A blood clot that breaks off and circulates through the venous system • Signs and symptoms • Dyspnea • Cyanosis • Acute pleuritic pain • Tachypnea • Hemoptysis • Varying degrees of hypoxia Pulmonary Embolism (treatment): • Administer oxygen. • Place patient in comfortable position, usually sitting. • Assist breathing as necessary. • Keep airway clear. • Transport promptly. Hyperventilation: • Overbreathing resulting in a decrease in the level of carbon dioxide • Signs and symptoms • Anxiety • Dizziness • Numbness • Tingling in hands and feet • A sense of dyspnea despite rapid breathing Hyperventilation (treatment): • Complete initial assessment and history of the event. • Assume underlying problems. • Do not have patient breathe into a paper bag. • Give oxygen. • Reassure patient and transport. You are the provider: • You and your EMT-B partner are dispatched to a 33-year-old woman with difficulty breathing. • You arrive at the office building and an upset man identifies himself as the patient’s coworker. • He tells you that the patient has had breathing problems before, but he’s never seen it this bad. • He leads you to a woman who is standing with her arms outstretched on the desk with a metered-dose inhaler in hand. • She acknowledges your presence with a nod. When you ask her what is wrong, she answers with a twoword response, “can’t breathe.” • You hear audible wheezes. Scene size up: • How significant is the person’s response to your question and why? • What should you do next? Should you transport this patient or wait for ALS to arrive on scene? Initial Assessment: • Perform initial assessment. • Place the patient on oxygen. • If patient is in respiratory distress, ventilate. • Check pulse. Signs and Symptoms: • Difficulty breathing • Irregular breathing • Altered mental status • Cyanosis • Anxiety or restlessness • Pale conjunctivae • Increased or decreased respirations • Abnormal breath sounds Increased heart rate • • Difficulty speaking You are the provider: • You arrange to rendezvous with ALS. • You apply high-flow oxygen and obtain the following vital signs: – Respirations: 42 breaths/min – Pulse oximetry: 90% • The patient indicates that she has used the inhaler twice already. • What can you do before you meet ALS? • Another pulse oximetry reading reveals a reading of 72%. • The patient is using accessory muscles to breathe. • What do these signs indicate? • Use of accessory muscles • Coughing • Tripod position • Barrel chest Focused History and Physical Exam: • Abnormal breath sounds are symptomatic of COPD • Long history of dyspnea with sudden increase in shortness of breath • Recent chest cold with fever • Vital signs – Normal blood pressure – Rapid, occasionally irregular pulse – Respirations rapid or very slow Interventions: • Treat immediate life threats • Possible interventions – Oxygen via nonrebreathing mask at 15 L/min – Positive pressure ventilations – Airway adjuncts – Positioning – Respiratory medications Detailed Physical Exam: • Performed only once life threats are addressed. • May not be able to do if busy treating airway or breathing problems. Ongoing assessment: • Carefully watch patients for shortness of breath. • Reassess vital signs. • Ask patient if treatment has made a difference. • Check for accessory muscle use. Emergency Medical Care: • Give supplemental oxygen at 10 to 15 L/min via nonrebreathing mask. • Patients with longstanding COPD may be started on low-flow oxygen (2 L/min). • Assist with inhaler if available. • Consult medical control. Medications in MDI: • Trade names • – Proventil – Albuterol – Ventolin – Metaproterenol – Alupent – Terbutaline – Metaprel – Brethine Prescribed Inhalers: • • Generic names Actions – Relax the muscles surrounding the bronchioles – Enlarge the airways leading to easier passage of air Side effects – Increased pulse rate – Nervousness – Muscle tremors Prior to Administration: • Read label carefully. • Verify it has been prescribed by a physician for this patient. • Consult medical control. • Make sure the medication is indicated. • Check for contraindications. Contraindications for MDI: • Patient unable to help coordinate inhalation • Inhaler not prescribed for patient • No permission from medical control • Maximum dose prescribed has been taken. Administration of MDI: • Obtain order from medical control or local protocol. • Check for right medication, right patient, right route. • Make sure the patient is alert. • Check the expiration date. • Check how many doses have been taken. • Make sure inhaler is at room temperature or warmer. • Shake inhaler. • Stop administration of oxygen. • Ask the patient to exhale deeply and put lips around opening. • If the inhaler has a spacer, use it. • Have the patient depress the inhaler and inhale deeply. • Instruct the patient to hold his or her breath. • Continue administration of oxygen. • Allow the patient to breathe a few times then repeat dose according to protocol. Reassessment: • Carefully watch for shortness of breath. • 5 minutes after administration: – Obtain vital signs again. – Perform focused reassessment. – Transport and continue to assess breathing