Ahmet_Rencuzogullari_LGB_ACS_OHIO
advertisement

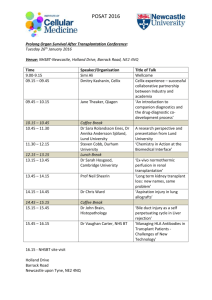
Incidence, Management and Risk Factors for Lower Gastrointestinal Bleed in Renal Transplant Recipients Ahmet Rencuzogullari1, Sinan Binboga1, Erman Aytac1, John Rabets2, Luca Stocchi1, Gokhan Ozuner 1 Department of Colorectal Surgery, Digestive Disease Institute1, Cleveland Clinic, Ohio Department of Urology, Transplantation Center2, Cleveland Clinic, Ohio Introduction: There is very limited data regarding management and outcomes of lower gastrointestinal bleed (LGB) in renal transplant recipients (RTR). The aim of this study is to evaluate incidence, management strategies and risk factors associated with LGB in RTR. Methods: Between 01/2004 and 12/2013, patients who were admitted to the hospital with LGB after renal transplantation were analyzed. LGB was defined as having clinical evidence of hemorrhage after upper gastrointestinal etiology was ruled out by bilious output via nasogastric tube or esophagogastroduodenoscopy. The comparison with respect to time to bleed after transplantation and recurrent bleed was performed by using a log-rank test with the KaplanMeier method. A p-value less than 0.05 was considered significant. Results: There were 1578 [n=987 (62.5 %) males] RTR with a mean age of 50 ± 14 years at the time of transplantation. Mean follow-up time after transplantation was 57 ± 45 months. 35 (2.9 %) patients had a documented site of LGB and in 10 patients the exact site could not be localized. The most common causes of bleed were colitis and angiodysplasia (38%, n=17). Mean time to LGB after transplantation was 43 ± 36 months. 12 (26 %) patients with LGB required intervention. 3 (6 %) underwent colectomy, endoscopic treatment was utilized in 8 (17%) and 1 (2 %) patient had angiographic embolization to control bleeding. Recurrent LGB developed in 11 (26 %) within a mean time of 9 ± 8 months, out of 42 patients who did not have surgery at the time of index bleed. Surgical (1) or endoscopic intervention (4) was required in 45% of recurrent bleeders. LGB was more commonly seen in RTR’s who developed a nonfunctioning kidney (p<.0001). RTR who developed a LGB had an increased overall mortality rate (not directly related to the bleeding episode) compared to those who did not experience a LGB (p=0.001). No increased risk of LGB was observed among patients who were on antiplatelet, antiaggregant or anticoagulant agents (p=0.76) Associations of risk factors and LGB in RTR are listed in the table. Conclusion: Non-functioning kidney after transplant is a risk factor for LGB. Overall mortality increases after LGB in RTR. There is no increased risk of lower gastrointestinal bleed in RTR who are on anticoagulanat or antiaggregan treatment. Table. Association of potential risk factors and Lower Gastrointestinal bleed. LGIB ( + ) LGIB ( -) P value Age>50 19/45 (42.2%) 754/1499 (50.3%) 0.65 Male gender 32/45 (71.1%) 929/1498 (62%) 0.12 BMI≥30 10/45 (22.2%) 526/1480 (35.5%) 0.14 African-American race 8/45 (17.7%) 332/1499 (22.1%) 0.23 Tobacco use 24/44 (54.5%) 692/1454 (47.5%) 0.31 Donor type (deceased) 29/45 (64.4%) 847/1491 (56.8%) 0.12 Non-functioning kidney 9/45 (20%) 43/1498 (2.8%) <.0001 Combined transplant* 6/45 (13.3%) 197/1499 (13.1%) 0.95 Blood-thinner usage** 35/44 (79.5%) 1259/1498 (84%) 0.76 BMI: Body Mass Index *Pancreas, liver or heart transplantation combined with kidney transplant. **Antiplatelet, antiaggregant or anticoagulant agents.