File - Jody Dawson:Nursing Portfolio
advertisement

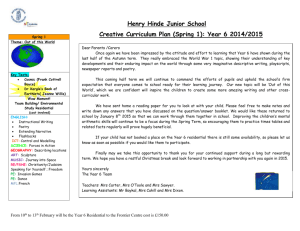
Running head: CLINICAL CASE SCENARIO Clinical Case Scenario: Expansion on Key Components of Concept Map Jody Dawson October 26, 2014 1 CLINICAL CASE SCENARIO 2 Clinical Case Scenario: Expansion on Key Components of Concept Map In order to ensure safe, competent, and ethical nursing practice, it is essential that entry-level Registered Nurses (RNs) demonstrate critical inquiry and evidence informed decision-making (College of Nurses of Ontario [CNO], 2014). Creating a concept map is an excellent way to facilitate critical thinking through complex health-care situations. Concept maps allow nurses to synthesize information from diverse sources of knowledge and use this information to prioritize their nursing interventions. The following is an expansion of the key components of the concept map created for the care of Mrs. S.B, which can be found in the Appendix. Patient Profile Mrs. S.B. is an 89-year-old woman who was admitted to the hospital with endstage osteoarthritis of her right hip. She was scheduled for the surgical intervention of total hip arthroplasty [THA]. Mrs. S.B. had two secondary diagnoses of hypertension and hyperlipidemia, which were controlled by medications. She lived in a two-story home with her husband, and their children and grandchildren all lived nearby. Pre-operative Nursing Interventions Prior to her surgery, it is essential to ensure that Mrs. S. B. has made an informed decision regarding her plan of care. Mrs. S.B. had a pleasant discussion with her physician where she was fully informed about the risks and benefits of the surgery, and she made an informed decision about her resuscitation care plan where she elected to have the health care providers allow natural death in the event that her heart stopped beating. CLINICAL CASE SCENARIO 3 Along with completing an assessment of Mrs. S.B’s functional capacity and allergies prior to her surgical intervention, it is important to address any socio-economic issues that may affect Mrs. S.B. in her recovery. For example, patients with low income and low education have been shown to be at increased risk for post-operative complications such as infection and poorer functional outcomes (Santaguida et al., 2008; Matar et al., 2010). Using a social determinants approach allowed us to address issues such as financial concerns Mrs. S.B. had regarding her plan of care, and also allowed us to ensure she had access to resources and information that would support her in her recovery. In our pre-operative assessment with Mrs. S.B. we also took the opportunity to integrate any preferences that were important to her physical, emotional, and spiritual health into her plan of care. Culture care preservation is an effective approach to promoting client centered and culturally sensitive care, and promotes positive health outcomes (College of Nurses of Ontario, 2009). Post-operative Nursing Interventions While THA is well known as being a highly effective intervention for patients suffering from severe arthritis of the hip, it is still associated with general risks. Older women as well as individuals with comorbidities are associated with having worse functional outcomes and increased risks of complications (Santaguida et al., 2008; Basilico et al., 2008). Mrs. S.B.’s age, gender, comorbidities and procedure in general pre-disposed her to various potential post-operative complications. The following is a discussion of these complications in order of priority for nursing interventions. Ineffective Tissue Perfusion CLINICAL CASE SCENARIO 4 Joint replacement surgery is associated with significant blood loss, and elderly patients presenting for THA tend to already have disorders in hematopoiesis associated with ageing (Conlon, Bale, Herbison, & McCarroll, 2008). On the day following her surgical procedure, Mrs. S.B. began presenting with symptoms of anemia. These symptoms included low serum levels of hemoglobin [Hg] (83g/L), low serum levels of hematocrit [Hct] (26%), pallor, increased fatigue, and shortness of breath on exertion. In treating Mrs. S.B. for symptomatic anemia, the physician ordered two units of a red blood cell IV transfusion, as well as 300mg of ferrous gluconate to be taken orally, twice daily. Prior to administering the blood transfusion, we explained the procedure to Mrs. S. B. and obtained her informed consent. We then monitored her throughout the entire transfusion for signs and symptoms of adverse reactions. Mrs. S.B.’s transfusion was effective with no adverse reactions. Her Hg and Hct returned to normal levels, her skin colour returned to normal and she was soon able to carry out appropriate activities without shortness of breath. Risk for Delayed Recovery Higher levels of post-operative pain following THA are associated with increased length of stay, delayed ambulation and long-term functional impairment (Morrison et al., 2003). Adequate pain management for elderly individuals is complicated by comorbid diseases, increased risks of adverse drug reactions, and physician reluctance to prescribe opioid analgesics (Mercadante, 2010). Patient controlled analgesia [PCA] has been demonstrated to be effective for older patients, and the use of PCA greatly reduces the risk of overdose (Mercadante, 2010). Mrs. S.B.’s pain relief was complicated by a knowledge deficit regarding the use of PCA. Once Mrs. S.B. received sufficient CLINICAL CASE SCENARIO 5 education regarding the use of her PCA device that infused 0.4mg of morphine every 15 minutes if she pressed her button, she was able to receive adequate pain relief by this intervention. Risk of Increased Sedation and Respiratory Depression Knowing Mrs. S.B.’s increased risk of sedation and respiratory depression when taking morphine, I monitored Mrs. S.B.’s respirations and oxygen saturation closely and provided continuous oxygen therapy while she received the opioid analgesic. I also completed frequent checks with my preceptor of the parameters of the PCA to ensure that the device was not infusing at a basal rate and that the lock-out interval and demand dose were consistent with the physician’s order. Risk of Neurovascular Dysfunction Orthopedic surgeries in general predispose patients to risks of neurovascular dysfunction, for example, pulmonary embolus, thrombophlebitis, and vascular complications (Jain, Guller, Pietrobon, Bond, & Higgins, 2005). The risk of postoperative neurovascular complications is increased when patients possess preoperative cardiovascular risk factors such as hypertension and hyperlipidemia (Dy, Wilkinson, Tamariz, and Scully, 2011). Due to her surgical operation, edema, immobility and comorbidities, Mrs. S.B. was at increased risk for neurovascular dysfunction. In order to address this risk, I continuously monitored Mrs. S. B. by assessing the circulation, sensation, and movement in her affected right extremity compared with her left. I assessed for deep venous thrombosis by assessing Homans’ sign, and I assessed for pulmonary embolisms by looking for signs of respiratory distress. Mrs. S.B.’s physician ordered 24-hour telemetry monitoring for her so that we could be quickly made aware of CLINICAL CASE SCENARIO 6 any issues such as ischemia, arrhythmias, and infarction. I educated Mrs. S.B. about the importance of foot pumping and mobilization, and assisted her in ambulating multiple times throughout the day in order to prevent vascular complications. Also, I administered her prescribed anticoagulant as prophylactic treatment for potential vascular complications. Risk for Infection Wound infection is a devastating complication and a leading cause of morbidity following THA (Matar et al., 2010). The risk of infection is increased for patients who are older than 75 years, who have received an allogenic blood transfusion, and who are administered a low-molecular-weight heparin, which can result in hematoma formation, reoperation, and subsequent infection (Matar et al., 2010). Having required an allogenic transfusion of two units of blood, being prescribed dalteparin for prophylactic control of deep vein thrombosis, and because she is 89 years old, Mrs. S.B. was at increased risk for infection. The provision of prophylactic antibiotics has been shown to be an effective method of reducing the incidence of post-operative wound infection (Matar et al., 2010). Mrs. S.B. was prescribed with 3 doses of cefazolin IV. We completed dressing changes with aseptic techniques, and educated Mrs. S.B. about monitoring for signs and symptoms of infection. Role Performance Altered There are many aspects of a patient’s experience that cannot fully be captured by standardized assessment tools and screening instruments, and can only be uncovered through shared moments of intentional relations that enable deeper connections. There was a moment where Mrs. S.B. began to express to me her worries about her husband CLINICAL CASE SCENARIO 7 and sadness for being apart from him. Through relational inquiry, I discovered that feelings of guilt were causing Mrs. S.B. significant spiritual distress. She was concerned about her ability to take care of herself when she returned home let alone continue cooking for and taking care of her husband. In identifying these concerns, we were able to assist Mrs. S. B. and her family by connecting them with appropriate resources such as the Community Care Access Center, meals-on-wheels, physiotherapy and assistive devices. Conclusion Using evidence gathered from multiple sources of knowledge, nurses can promote safe, competent, and ethical nursing care that reflects the principles of relational practice and critical thinking. A concept map is a useful tool to illustrate the integration of evidence-based knowledge into holistic nursing processes and interventions based on prioritized nursing care. By creating a concept map for the case of Mrs. S.B., the complex individual components of her experience were linked in a comprehensive, effective, and clarifying visualization. CLINICAL CASE SCENARIO 8 References Basilico, F., Sweeney, G., Losina, E., Gaydos, J., Skoniecki, D., Wright, E., & Katz, J. (2008). Risk factors for cardiovascular complications following total joint replacement surgery. Arthritis & Rheumatism, 58(7), 1915-1920. doi: 10.1002/art.23607 College of Nurses of Ontario. (2014). Competencies for entry-level Registered Nurse practice. Retrieved from http://www.cno.org/Global/docs/reg/41037_EntryToPracitic_final.pdf College of Nurses of Ontario. (2009). Culturally sensitive care. Retrieved from http://www.cno.org/Global/docs/prac/41040_CulturallySens.pdf Conlon, N., Bale, E., Herbison, G., McCarroll, M. (2008). Postoperative anemia and quality of life after primary hip arthroplasty in patients over 65 years old. Anesthesia & Analgesia, 106(4), 1056-1061. doi: 10.1213/ane.0b013e318164f114. Dy, C., Wilkinson, J., Tamariz, L,. & Scully, S. (2011). Influence of Preoperative Cardiovascular Risk Factor Clusters on Complications of Total Joint Arthroplasty. The American Journal of Orthopedics, 40(11), 560-565. Retrieved from http://hosp.gcnpublishing.com/fileadmin/qhi_archive/ArticlePDF/AJO/0401105 60.pdf Jain, N., Guller, U., Pietrobon, R., Bond, T., Higgins, L. (2005). Comorbidities increase complication rates in patients having arthroplasty. Clinical orthopedics and related research, 435, 232-238. doi: 10.1097/01.blo.0000156479.97488.a2 CLINICAL CASE SCENARIO Matar, W., Jafari, S., Restrepo, C., Austin, M., Putrill, J., & Parvizi, J. (2010). Preventing infection in total joint arthroplasty. Journal of Bone & Joint Surgery, 92, 36-46. doi:10.2106/JBJS.J.01046 Mercadante, S. (2010). Intravenous patient-controlled analgesia and management of pain in post-surgical elderly with cancer. Surgical Oncology, 19, 173-177. doi: 10.1016/j.suronc.2009.11.013 Morrison, R., Magaziner, J., McLaughlin, M., Orosz, G., Silberzweig, S., Koval, K, & Sui, A. (2003). The impact of post-operative pain on outcomes following hip fracture. Pain, 103(3), 303-311. doi: 10.1016/S0304-3959(02)00458-X Santaguida, P., Hawker, G., Hudak, P., Glazier, R., Mahomed, N., Kreder, H., Coyte, P, & Wright, J. (2008). Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: A systematic review. Canadian Journal of Surgery, 51(6), 428-436. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2592576/ 9 Running head: CLINICAL CASE SCENARIO 10 Appendix esent Illnesses Ferrous Gluconate 300 mg PO BID Amlodipine: 5mg bedtime Acetylsalicytic Acid: 81mg PO QD Hydrochlorothiazide: 18.75mg PO q morning Ramipril: 15 mg PO q morning Atorvastatin: 20mg PO bedtime Pt Hg 83 g/L, Pt Hct 26%, pallor, increased fatigue, SOBOE 1. Ineffective Tissue Perfusion r/t blood loss during surgery and complicated by disorders in hematopoiesis associated with aging Obtain consent, administer blood products, Pt teaching re: administration of blood products, promote adequate rest and nutrition Ferrous Gluconate 300mg BID Hypertension Hyperlipidemia Anemia Two Units Packed RBCS Pt demonstrates no S/S adverse reaction to transfusion Pt’s Hgb returns to normal level (120-156 g/L), , Pt’s Hct returns to normal level (35-46%), pt’s skin returns to normal colour, pt able to carry out goals with minimal fatigue/SOB Pre-op assessment: ?Allergies ? Functional Capacity ? Socioeconomic concerns Pt teaching re: foot pumping, & extremity mobilization 2. Risk for Delayed Recovery r/t ineffective pain management Convey empathetic understanding of patient’s incisional and arthritic joint pain; educate patient re: PCA; maintain affected joint in aligned position, and maintain extremity mobilization Morphine, PCA, SC Basal Rate = 0 Demand dose = 0.4mg Lock-out interval = 15 min Boluses/hr = 4 Volume: 15 ml bag Pt demonstrates understanding of PCA, Pt rates pain < 4/10 Present Illnesses Pt’s PPP, pt denies numbness/tingling, pt completes > 4 walks/day, -ve Homans’ sign ★ End –Stage Osteoarthritis Right Hip Acute Pain Elective Surgery: Total Hip Arthroplasty 5. Risk for Infection r/t invasive procedure and disruption of skin integrity WBCs elevated (12), T 36.5°C Respirations 10, SpOs = 89% 3. Risk of Increased Sedation and Respiratory Depression r/t adverse effect of opioid narcotic Apply 2 L O2 ; monitor RR and SpO2, monitor PCA parameters Pt maintains adequate resps, SpOs > 92% Nursing Assessment Dalteparin 5000 units, SC, QD ? Adequate circulation, ? Adequate sensation, ? Adequate movement ? Homans’ sign Telemetry monitoring for ? Ischemia, ? Arrhythmias, ? Infarction Admitting Diagnosis: Pt rating pain 6/10, facial grimacing Patient teaching re: healthy lifestyle modifications 4. Risk of Neurovascular Dysfunction r/t immobilization, potential vascular obstruction in surgery, edema, comorbidities Mrs. S. B. ★ Age: 89 ★ Gender: Female Allergies: NKA Resuscitation Status: Allow Natural Death Social: Lives with husband in 2-story home HR = 82, BP = 134/89 Nursing Diagnoses Pt is concerned because she is care provider for husband. Promote good hand hygiene; use aseptic techniques when changing dressings; Pt teaching re: S/S infection 6. Role Performance Altered r/t compromised mobility Address concerns of patient by connecting with appropriate resources ie. CCAC, meals on wheels, physiotherapy, and assistive devices. Pt denies any concerns re: discharge. Pt has support systems in place to assist she and her husband during her recovery. Pt shows confidence and increased selfefficacy with discharge plan Nursing Interventions Pharmacological Therapy Cefazolin 2g, IV, q8H, 3 doses Pt’s WBC count returns to normal (510x109 /L), wound site shows no redness, swelling, purulent drainage, odor, pt remains afebrile Expected outcomes ★ Known Risk Factors