The puerperium
advertisement

The puerperium
بتول عبد الواحد هاشم0د
Term which refer to 6 weeks period after child birth during which the pelvic organs
return to non pregnant state,metabolic changes of pregnancy reversed and lactation
starts, it's also time of psychological adjustment to cope with additional
responsibilities and anxiety about child welfare.so the role of obstetrician and
midwife are to 1-monitor the physiological changes of puerperium
2-to diagnose and treat any postnatal complications
3-give the mother emotional support
4-advice about contraception
5-other measures which will contribute to continuing health.
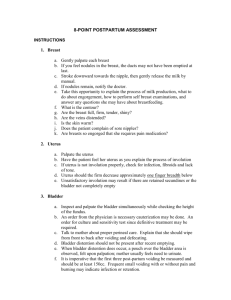
The uterus:
The crude weight of pregnant uterus at term is approximately 1000 gm and the
weight of non pregnant uterus is between50-1.00gm. By 6weeks postpartum,the
uterus has returned to it's normal size, clinically immediately after birth the uterine
fundus lies 4 cm below the umbilicus or more accurately 12 cm above the symphysis
pubis, within 2 week postpartum it is no longer palpable. The cervix itself is very
flaccid after delivery but within few days returns to it's original state uterine
involution occurs by process of autolysis ,in which muscle size diminishesas aresult of
enzymetic digestionof cytoplasm.this has no effect on the number of muscle cells,
and the excess protein produced from autolysis is absorbed into blood stream and
excreted in urine. Involution is inhanced by oxytocine release in women who breast
feed causes of delayed uterine involution
1-full bladder
2-loaded rectum
3-uterine infection
4-retained products of conception
5-fibroid
6-broad ligament haematoma
1
Genital tract changes:
Following delivery of the placenta, the lower segment of the uterus and cervix
appear flabby and there maybe small cervical lacerations. In the 1st few days , the
cervix can readily admit two fingers , but by the end of the 1st week it should become
increasingly difficult to pass more than one finger , and certainly by the end of the
2nd weekthe internal os should be closed. However , the external os can remain open
permanently , giving a characteristic appearance to the parous cervix. In the 1 st few
days , the stretched vagina is smooth and edematous , but by the 3rd week rugae
begin to appear.
Lochia:
It's the blood stained uterine discharge that's comprised of blood and necrotic
decidua. Only the superficial layer of decidua becomes necrotic and is sloughed off.
The basal layer adjacent to the myometrium is involved in the regeneration of new
endometrium and this regeneration is complete by 3rd week. During the 1st few days
fter delivery, the lochia is red; this gradually change to pink as the endometrium is
formed , and then ultimately become serous by the 2nd week. Persistant red lochia
suggests delayed involution . offensive lochia which may be accompanied by pyrexia
and a tender uterus, suggest infection and should be treated with broad spectrum
antibiotics.
Retained placental tissue is associated with increased blood loss and clots, and this
may be suspected if the placenta and membranes were incomplete at delivery
management includes the use of antibiotics and evacuation of retained product
under anaesthesia
Puerperal disorders:
Perineal complications:
Perineal discomfort is the single major problem for mothers, discomfort is greatest
in women who sustain spontaneous tears ,have episiotomy ,and those underwent
instrumental delivery various pharmacological and non pharmacological therapies
have been used including local cooling,topical anaesthetic,paracetamol, diclofenac
suppositories given at delivery followed by another12 hr laterare significantly more
effective. Codeine derivatives are not preferable, as they have tendency to cause
constipation
Perineal infection present with redness, pain, swelling and heatsometimes with
raised body tempreture, these must be taken seriously. Swabs for microbiological
culture and broad spectrum antibioticsshould be started ,pus collection requires
drainage with removal of skin suture; otherwise infection spread, with increasing
2
morbidity and poor anatomical results.surgical repair should never be attempted in
presence of infectionthe wound is irrigated twice daily and healing should be
allowed to occur by secondary intention, if wound is widely gapped secondary repair
is only done after the infection has cleared.
Bladder function:
Voiding difficulty and over distension of the bladder are not uncommon after
childbirth the bladder may take up to 8 hr to regain normal sensation, after epidural
/spinal anesthesia during this time 1 L of urine may be produced ,over stretching of
the detrusor muscle can dampen bladder sensation and make the bladder
hypocontractile ,traumatic delivery ,multiple extended perineal wounds,
vulvovaginal haematoma prolapsed haemorrhoids, anal fissures, may further
exacerbate retention, the midwife need to be careful to avoid bladder
distension(clinically evident by palpable suprapubic cystic mass and lateral or
upward displacement of the uterus. Urinary catheter may be left 12-24
hrafterCSdone under regional anesthesia, any women who did not pass urine >4 hr
of delivery should be encouraged to do so before attempting catheterization , if post
voiding residual urine is >300 ml a catheter is left in situ to allow free drainage for 48
hr.
Urinary incontinence is rare problem in early Peurperium and it requires
investigation to exclude vesicovaginal ,or rarely uretrovaginal fistula, pressure
necrosis may occur following prolonged obstructed labour , incontinence usually
occur in the 2nd week when the slough separates. Small fistulae may close
spontaneously after few weeks of free bladder drainage., large fistulae require
surgical repair.
Bowel function :
Constipation is common problem in the puerperium. This may be due to interruption
in the normal diet and possible dehydration during labour. Advice on adequate fluid
intake may be all that's necessary. Constipation may also be the result of fear of
evacuation due to pain from sutured perineum, prolapsed haemorrhoids or anal
fissures. Avoidance of constipation and straining is more important in labours
complicated by 3rd or 4th degree perineal tear. As this may disrupt the repaired anal
sphincterand lactulose or methylcellulose is given for a period of 2 weeks. Anal
endosonography has identified evidence of occult anal sphincter trauma in 1/3 of
primiparous women, but only 13% have symptoms by 6 weeks postpartum.
Anal incontinence following primary repair of 3rd or 4th degree tear occur in 5% of
women/ and anovaginal /rectovaginal fistulae occur in 2-4% of these women .it's
therefore important to consider a fistula as a cause of anal incontinence in the
3
postpartum period, particularly if the women complain of passing wind or stool per
vagina. Approxmately50% of small anovaginal fistulae will close spontaneously over
period of 6 months, but larger fistulae will require formal repair, frequently with a
covering colostomy.
Secondary postpartum haemorrhage:
It's defined as fresh bleeding from the genital tract between24 hr to 6 weeks after
delivery. The most common time for secondary PPH is between day 7-14, the most
common cause is retained placental tissue. Other less common possible causes of
secondary PPH include endometritis,hormonal contraception, bleeding disorders e.g.
von Willebrands disease and choriocarcinoma treatment include, IV infusion, cross
match, syntocinon, an examination under anaesthsia and evacuation of the uterus.
Antibiotic should be given if placental tissue is found, even without evidence of overt
infection.
Obstetric palsy:
Or tuamatic neuritis, is a condition in which one or both lower limbs may develop
signs of a motor and /or sensory neuropathy following delivery. Presenting features
include sciatic pain, footdrop, parasthesia, hyposthesia and muscle wasting.the
mechanism of injury is unknown and it was previously attributed to compression or
stretching of the lumbosacral trunkas it cross the sacroiliac joint during descent of
fetal head. It's now believed that herniation of lumbosacral disc can occur in
exaggerated lithotomy position and during instrumental delivery. Orthopedic
opinion should be sought.
Symphysis pubis diastasis
This occur spontaneously in at least1/800 vaginal delivery, surgical symphysiotomy
performed to increase the pelvic diameter treatment include bed rest, antiinflammatory agents, physiotherapy, and a pelvic corset to provide support and
stability.
Thrumboembolism :
Thrumboembolism risk rises 5-fold during pregnancy and the puerperium. The
majority of death occur in the puerperium. And are more common after CS, if DVTor
pulmonary embolism is suspected full anticoagulant therapy should be commenced
and a bilateral venogram and or lung scan should be carried out within 24-48hr.
4
Puerperal pyrexia: it s defined as a temperature of 38C(100.4 F) or higher on any
2 of the first 10 days postpartum, exclusive of the 1st 24 hours('measured orally by a
standard technique), common sites associated with puerperal pyrexia include chest,
throat, breasts, urinary tract, pelvic organs, Caeserian or perineal wounds, and legs.
Chest complications:
This are most likely to appear in the 1st 24 hr after delivery, particularly after general
anesthesia, atalectasis may be associated with fever and can be prevented by early
and regular chest physiotherapy.
Aspiration pneumonia(Mendelson's syndrome) must be suspected if theres
wheezing, dyspnoea, a spiking temperature and evidence of hypoxia.
Genital tract infection(puerperal sepsis):
Incidence(3%), account for 7% of all direct maternal death.
Aetiology of genital tract infection
, perineum and lower genital tract.
The most frequently isolated micro organism include
Group BStreptococci
Mycoplasma
Haemolytic streptococcus Lancefield group A
Staphylococcus aureus
Chlamydia trachomatis
Risk factors for puerperal infection
Antenatal intrauterine infection, CS, cervical cerculage or cervical incompetence,
prolonged rupture of membrane, prolong labour, multiple vaginal exam,
internalfetal monitoring, instrumental delivery manual removal of placenta, retained
product of conception, obesity ,DM, HIV.
Symptoms/signs:
Malaise,headache, fever,rigors, abdominal discomfort, vomiting and diarrhea,
offensive lochia, secondaryPPH, o/E pyrexia, tachycardia, boggy tender enlarged
uterus, perineal Caeserian wound infection peritonism paralytic ileus, parametritis.
Investigations
5
FBC,urea &electrolytes,HVS (c&s), blood culture, pelvic ultrasound, clotting screen,
arterial blood gases.
Treatment:
Mild-moderate infection treated with a broad spectrum antibioticamoxiclav or
cefalexin plus metronidazole, first few doses shold be given intravenously.
Severe infection, theres release of inflammatory and vasoactive mediators in
response to the endotoxine produced during bacteriolysis.the resultant local
vasodilatation causes circulatory embarrassment and hence poor tissue
perfusion(septic, endotoxic shock) and delayed management could be fatal.
Necrotizing fasciitis is rare but frequently fatal infection of skin, fascia and
muscle.can originate in perineal tears, episiotomies, and CS wounds.CL perfringens is
usually identified.beside measures taken to manage septic shock , wide deridment
of necrotic tissue under anaesthsia is absolutely essential to avoid mortality, split
thickness skin graft may be needed.
Prevention of puerperal sepsis;
Increased awareness of general hygiene,
Good surgical approach
Use aseptic technique
Prophylactic antibiotic during emergency CS.
6