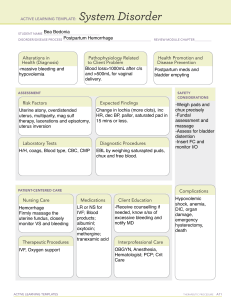
z NURSING CARE OF A POSTPARTUM CLIENT z POSTPARTUM ASSESSMENT: "BUBBLES“ Breast, Uterus, Bowels, Bladder, Lochia, Emotional Status, Section/Episiotomy z COMPLICATIONS IN POSPARTUM CLIENT POSTPARTUM HEMORRHAGE (PPH) Postpartum hemorrhage is one of the leading causes of death among postpartum women. PPH refers to a blood loss of at least 500 mL after a vaginal birth and at least 1000 mL after a C-section. There are a number of reasons that a PPH may occur and are related to the four T’s: Tone Atony Trauma Lacerations, hematoma, inversion, rupture Tissue Retained placenta, invasive placenta Thromin Coagulopathies z Early hemorrhage occurs within the first 24 hours after birth and can be caused by uterine atony, lacerations, and hematomas. Manly caused by Uterine Atony and Laceration Late hemorrhage is classified as more than 24-hours post-delivery but less than 6-weeks after birth. Typically, late hemorrhage is associated with subinvolution and the failure of the uterus to return to a normal size. This may be due to a retained placenta/membranes or an infection. UTERUS z UTERINE ATONY RISK FACTORS • Retained placenta • Chorioamnionitis (infection) • Uterine fatigue INTERVENTIONS • Full bladder • Fundal massage SYMPTOMS • Assist to void or use in-and-out catheter • Enlarged • Soft • Boggy • Poorly contracted uterus • Not midline Administer uterine-toning medications, such as oxytocin. Encourage the mother to breastfeed, as nipple stimulation can enhance uterine contractions. If bleeding persists, additional interventions like medications (e.g., misoprostol), uterine artery embolization, or surgical measures may be z b. Lacerations - tear in the perineum or vulva, bleeding persists despite firm uterus Sites: a. Cervical - usually found on the sides of the cervix near the branches of the uterine artery. b. Vaginal - Although they are rare, lacerations can also occur in the vagina. They are easier to assess than cervical lacerations, because they are easier to view. z b. Perineal- Occurs when a woman is placed in a lithotomy position for birth, because this position increases tension on the perineum. Degree of perineal lacerations: z z c. Retained placental fragments - part of placental tissue is left in the uterus interfering with uterine contractions. Signs and symptoms: 1. Vaginal bleeding 2. Soft or non-palpable uterus 3. Signs and symptoms of shock Management: 1. Dilatation and curettage -to remove the placental fragment 2. Monitor vital signs and I and O 3. Massage fundus until firm 4. Ice cap on the fundus 5. Estimate and monitor blood loss 6. Fluid replacement and administration of oxytocin 7. Facilitate frequent bladder emptying z d. Sub-involution - failure of the uterus to return to its prepregnant state Causes: 1. Retained placental fragments 2. Infection 3. Uterine tumors Signs and symptoms: 1. Enlarged boggy uterus 2. Prolonged lochia discharge 3. Backache Management: 1. Administration of methergine 2. Antibiotics 3. Dilatation and Curettage 4. Client instruction for signs and symptoms to report z e. Hematoma - collection of blood in the subcutaneous layer of tissue of the perineum Causes: 1. Vulvar varicosities 2. Precipitate labor 3. Injury to the blood vessels in the perineum during birth 4. Inadequate suturing of lacerations 5. Rupture of vein during episiorrhaphy Signs and symptoms: 1. Perineal pain 2. Swelling 3. Skin discoloration 4. Tenderness 5. Feeling of pressure over the vagina Management: 1. Ligation of bleeders 2. Analgesics 3. Ice packs 4. Antibiotics Postpartal/Puerperal Infection z a. Puerperal infection - Any infection of the reproductive organs that occurs within the first 6 weeks after childbirth or 4 weeks after abortion; usually localized in the endometrium. Postpartum infections are the leading cause of nosocomial infections and maternal morbidity and mortality. Predisposing factors: 1. Strongest predictors of developing a puerperal infection: a. Duration of labor > 18 hours b. Route of delivery: The single most significant risk for postpartum infections - 20 times greater than in the vaginal birth is cesarean section c. Colonization of amniotic fluid 2. Rupture of membrane over 24h before birth 3. Retained placental fragments 4. Postpartal hemorrhage 5. Pre-existing anemia and malnutrition; obesity 6. Instrumental birth 7. Internal fetal monitoring 8. Local vaginal infection at the time of birth - UTI, STDs 9. Invasive procedures in prolonged labor with frequent vaginal examinations z Signs and symptoms: 1. Fever, chills and tachycardia 2. Change in the color, amount, odor (foul) and consistency of lochia 3. Painful/tender uterine fundus, delayed uterine involution 4. Body malaise, anorexia, headache 5. Dysuria, burning sensation on urination, costovertebral tenderness Complications: 1. Pelvic inflammatory disease 2. Pelvic cellulites 3. Generalized peritonitis 4. Puerperal sepsis one of the leading causes of maternal mortality z Management: 1. Maintain bed rest 2. Start with ordered antibiotics stat (after appropriate specimen is obtained); a broad-spectrum antibiotic directed at multiple organisms often are administered prophylactically for cesarean sections and prolonged rupture of membranes 3. Observe standard precautions and careful handwashing. 4. Monitor vital signs and I &0; force fluids - 3,000 to 4,000 ml if not contraindicated and encourage frequent voiding 5. Promote drainage of secretions 6. Teach regarding perineal hygiene 7. Provide nutritious, high calorie, high protein, high iron diet 8. Promote client's comfort z b. Infection of the perineum, vulva, and cervix Signs and Symptoms: 1.Pain/pressure on the affected area 2. (+) pus 3. Fever 4. Redness and swelling 5. Dysuria Management: 1. Proper perineal hygiene 2. Sitz bath, and warm compress 3. Establish drainage 4. Analgesics 5. Antibiotics z c. Endometritis - infection of the endometrium Risk factors: 1. Cesarean Section 2. PROM 3. Prolonged labor Signs and symptoms: 1. Fever/chills 2. Foul smelling lochia 3. Boggy and enlarged uterus 4. Uterine tenderness 5. Body malaise 6. Lack of appetite 7. Backache Management: 1. Antibiotic therapy 2. Analgesic 3. Oxytocin 4. Increase fluid intake 5. Frequent changing of perineal pad 6. Nutritious diet 7. Monitor V/S