January 2014 First year doctor tweets
advertisement

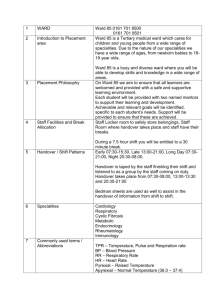
A week in the life of a first year doctor Monday 6th January Hello and Fàilte gu NHS Highlands Who We Are! My name is Thom (@fakethom ) and I'm a doctor at Raigmore. @nhshighland It's my first year as a doctor (called FY1) & I'm currently working on the gastrointestinal medicine ward. This week I will try to give a glimpse of life a junior doctor in The Highlands. Each day will have a theme. I want to point out that it is a 'typical' week. I am not tweeting live from work. Any patient stories or details are fictional amalgamations of truer stories. If you have any questions or feedback please feel free to tweet me on my personal account @fakethom at any time! Today I will give some background to how someone becomes a doctor and how I ended up moving to Inverness from Brighton! From tomorrow through to Sunday, tweets with snippets of my working days will hopefully show the range of this fantastic job. Each day will focus on a different aspect of the day-to-day job. I'll #storify each day and then again for the whole week. If I get time I will try to blog a summary and tie everything together at the end of the week, and elaborate on any highlights. So a little bit about me. I'm from that London they have now and trained in the fantastic city of Brighton. My nickname is @fakethom as there was another Tom O'Neill in the year above at school (the 'real' one!). The name stuck! I have an interest in medical school admissions, and have worked for Brighton's Widening Access To Medicine Scheme. If you have questions about applying to medical school feel free tweet me @fakethom and I'll try point you in the right direction! I'm a @BSMSalumni & moved from Brighton to Inverness after being allocated a job at Raigmore out of all the jobs in Scotland! Somehow I managed to for my life into my wee Renault Clio (called Cleopatra, of course) and drive Brighton to Inverness over 2 days! 1 When I'm not being a doctor, or trying to be The Doctor, I volunteer for a charity called @OverTheWallCamp OTW provides therapeutic camps for sick kids and has shaped the person I am today, and the kind of doctor I (try) to be! I'm aiming to become a paediatrician. Not sure what brand yet, but plenty of time to mull that one over! But first I'll need to get through foundation years, the start of my professional training after medical school. As a Foundation Year doctor, I change jobs every 4 months to give me a wide range of training before I specialise. My first job was in Medicine for the Elderly. It was a superb job to start my career with, as it's very holistic and patient focused. After time on the acute medical receiving unit, (I'll tweet about it at the weekend) I'm now on GI medicine. As I want to be a medic (surgery is beyond my abilities!) I'm quite lucky having two medical jobs back to back. I'm learning and developing my clinical skills all the time, and being given more responsibility as I progress. As an FY1, I am yet to gain full registration to practice. It means the hospital has overall responsibility for me. Technically there is always someone to supervise clinical decision making: always someone to ask! I asked a lot of questions when I first started. I'm starting to ask fewer simple questions now as I gained experience. I have also loaded useful guidelines and protocols onto my phone to quickly look things up. On my phone: Highland Formulary (for drugs and guidelines), quick protocols for replacing some vital salts in the body... Flow charts for various heart problems, resuscitation protocols and also an array of apps such as medical calculators. Reference apps are always up to date, more so than books, and are instantly accessible. A vital key for doctors today. My most used app however is the NHS Highland Telephone Directory!! The other amazing resource on my phone is actually twitter itself! Lots of medical professionals who inspire and teach! 2 For those of you not familiar with NHS Highland or Raigmore Hospital, here are some stats... NHS Highland covers the largest catchment area of any health authority in Scotland, around 40% an area the size of Belgium. It caters for a population of nearly 310,000 people, as well as the large numbers of tourists who visit each year. There are a number of community hospitals across The Highlands. Raigmore is the receiving hospital and provides tertiary level care. Raigmore has approx 450 beds and includes a Children's Ward, Obs&Gynae/Delivery Suite, ENT surgery and ITU. It has a cath lab and is a centre for interventional radiology. A heli-pad receives patients from all over the North of Scotland. I'm lucky enough to be one of the 25 or so FY1s to work at Raigmore this year. Over the week, hopefully you'll get a glimpse of this! So stick around, and ask anything you fancy @fakethom - see you at 8.45 tomorrow for handover! Tuesday At 8.30-08.45 it's morning handover from the Hospital At Night team. I have to stop by on the way to my ward to get updates. They let us know if anything happened on our ward during the night and if so what was done. This handover is for the junior doctor/nurse practitioner from each ward and helps us prepare and prioritise for the morning. Today I'm told about a new patient who came in yesterday evening with an exacerbation of his Crohn's disease. This is important information as I'll make him a priority to see early on in the ward round. But first... Ward safety brief & mini-MDT: quick run through of all patients & what the current plans are. Physio & OT also present. Also look at barriers to discharge. (An MDT is a multi-disciplinary team meeting, with nurses, physio- & occupational therapists, social workers & doctors) Will look more at the MDT later in the week. They're key to providing patients with as seamless care as possible. Daily ward round: Today the consultant is with us. The ward round team ideally is the consultant, registrar, pharmacist, charge nurse & me. The aim of the ward round is to decide/update management plans for each patient and to see if any new issues have arisen. 3 My job on this consultant ward round is to generate a list of jobs required for each patient, and manage the checklist. Jobs include filling out any request forms or referrals to other teams, and update the blood results for each patient. We use a simple ward round checklist to make sure important things that apply to every patient aren't missed. These include reviewing drugs, checking the basic observations, and removing any unnecessary drips etc. They are simple tick boxes but mean the important things don't get missed. The current checklist is focused on patient safety. I want to add two points to it to make it even more patient focused. 1) Has everyone on the ward round been introduced to the patient? (Wards have many members of staff come & go between patients & it can be difficult to know who's who at the best of times.) 2) Has the management plan been explained to the patient? (Seems simple but it can be easy to think you've explained a plan when actually it's just been discussed in front of the patient) I'll be suggesting these to the quality development lead once I have tried out the new checklist on my ward. Today we have 22 patients to see, most of whom have a gastrointestinal problem. We commonly see liver disease, which can sometimes just occur out of the blue, but can also be related to alcohol consumption. We also see bowel conditions such as Crohn's disease. This is where the bowel lining is damaged and has a range of symptoms. Patients with Crohn's disease can be looked after by medical teams, such as the patients on my ward, or by surgeons. Part of my job on this ward involves liaising with surgical teams if a patient might require surgery. Thanks to the handover from Hospital At Night, we see the person with worsening Crohn's disease first this morning. We are seeing them first because they are new to the ward and probably the most acutely unwell, and may also require surgery imminently. 4 As a team we decide we can monitor them over the next few days, and support them with fluids and steroids through a drip. Young people with serious conditions such as Crohn's can appear very well but may 'drop off' & become very unwell very quickly. We use a number of indicators to assess how unwell somebody is. Their basic observations, such as heart rate & blood pressure are key. Most importantly though is the patient's story. Every detective knows the clues lie in the story. Asking the right questions and listening carefully to the patient tell their story can tell you a great deal. I think the 'perfect' doctor would be a combination of Sherlock Holmes, Obi-Wan Kenobi, and of course, The Doctor. As the junior, I often find patients relax and talk more freely than they sometimes do with consultants. Occasionally vital clues to a patient’s condition can be picked up by a junior, which are key to how we progress with their care. And of course, a good chat is always a benefit to a patient, and to me too I find. It can be hard to find time to chat to patients at length, but it is important. The ward can be a really busy place with lots of people coming and going. Discussions can be tricky. Communication is vital to good patient care. If there are barriers to this, we need to find ways to effectively communicate. This could be as simple as asking for the vacuum cleaner to be turned off whilst talking to a patient who is hard of hearing. Or it could involve getting other people or services to help with communication for a patient. This morning I found it harder than usual to talk to an elderly person on my ward. I think their hearing aid might have broken. Whilst the consultant is writing in the patient's notes, I use the ward mobile to call audiology and ask for someone to look at the hearing aid. There are lots of little jobs involved in patient care, and often the juniors are the best people for the job. My pager has bleeped. Everyone carries their own bleep, so you can be contacted by other people involved in a patient's care. I phoned the number on my pager and it's the labs to inform me a blood sample taken this morning has clotted and needs repeating. 5 Whilst sometimes annoying, the bleep system is a pretty good way of directly contacting the right person when needed. Once the ward round finished, the registrar and I compiled a list of jobs to do for the afternoon. We divide these up and crack on. They included making referrals for specialist reviews and requesting imaging. Phoning GPs and speaking to relatives to keep everyone up to date is another crucial part of good patient care. The afternoon is unusually quiet for the GI ward, which has some of the most unwell patients in the hospital. It's a good chance to update some of the computer records, write in the latest lab results, and update patient relatives during visiting hours. Before the end of the day, I prepare things for the morning such as who needs bloods taken. This includes filling out the blood forms to help out the phlebotomists (the vampires!) tomorrow morning. The phlebotomist on my ward is wonderful and I wouldn't be able to do my job without her! Before going home, I go to handover to update the evening team and alert them of any things that need doing tonight. I let them know about the new patient with Crohn's and that if they deteriorate they will need an urgent surgical review. Good handovers mean that patients get better continuity of care between day and night teams, therefore improving safety. Time for home. Tomorrow I am on a 'long day'. This means I carry the crash bleep, and cover all the medical wards in the evening. Actually I quite like responding to the challenges of arrests. As an FY1, there are (usually!) many more senior people present at arrests! If anything they are really good learning experience. So we will see what tomorrow brings! Feel free to tweet me questions/feedback to @fakethom and I will be happy to (try and) answer! Wednesday Morning all! And hello to any new followers to the account. @fakethom here for another glimpse of FY1 life. I'd come in a little early this morning (8am) to get a discharge letter finished and printed for a patient who left hospital last night. 6 Discharge letters are really important as they let both the patient and their GP know all about their time in hospital and the current plan. Unfortunately the computer system had a fault yesterday evening meaning it had to wait until today. The patient was able to get away on time as they were given a hand-written prescription and I wrote them a discharge letter to keep. Now the system is back up and running, a formal copy of the letter can be sent to the GP and I can also get a copy sent posted to the patient. Sometimes if the ideal isn't possible, an FY1 has to adapt and find the next best solution. And yes, I did try turning it off and on again. Before morning handover, I pick up the on-call pager from the night team on the medical receiving unit as I'm on a 'long-day'. This means I spend the day on my ward, but the evening covering all the medical wards until the night team arrive. A senior doctor is on-call too. If there is a cardiac arrest or similar emergency in the hospital during the day, however, the on-call pager will go off. For now, I clip it inside my pocket and hope it stays as inanimate as it is now. Nothing is handed over. It's been a quiet night. Today the ward round is just the registrar (senior doctor) and me. It takes is a little longer to see each patient, but we make our way round steadily. There are a few patients who require some investigations to help us diagnose the underlying causes of their symptoms. One patient is having difficulty passing urine and had to have a catheter inserted earlier this morning by one of the nurses. We look at the whole picture and use a number of different things to give us clues as to what might be causing this. These include looking at the person's blood pressure, as changes in this can affect the kidneys, and also the medication they are on. These bedside observations give us instant information to help paint a picture of what is happening. But some clues need to be hunted for... Another easy one is to test the urine that's come from the catheter to see if there are any clues, such as an infection. This can be quickly done with a dipstick, and also in the laboratory for more detailed analysis after the initial dip. 7 I'll also need to arrange an ultrasound scan of the patient's abdomen, which will also include the kidneys and bladder. I have to fill out a request form for the scan, with all the relevant information on it, and take that to the radiology department. Some scans, such as CT and MRI scans need to be discussed with a radiologist first. The more information the better, so it's important to know the patient well before heading off to radiology. On occasion I've taken a scan request down on behalf of another doctor, where I haven't known much more than was written on the form. It's harder to have an effective discussion instances & shows why it's important to know what you're on about! I can set the wheels in motion for all of this and gradually the puzzle pieces will present themselves. It's my job to collect the puzzles pieces and try and fit them together, whilst discussing the results with my registrar too. Some mixed analogies with wheels and puzzles there. Run with us. After the ward round, we realise it's gone lunch time and decide we should probably try and get a coffee to keep us going. The hospital can be very busy, especially at this time of year, and often we miss the canteen opening times. Thankfully Raigmore has an excellent Cafe, with all the coffee we could possibly need! Re-caffeinated, the registrar and I (wouldn't that make a terrible musical?) head back to the ward. BEEP BEEP BEEP BEEP BEEP "CARDIAC ARREST, ONE OF THE WARDS, CARDIAC ARREST." It would go off just as I reach the top of the 7th flight of stairs, only to turn back and head quickly to the other side of the hospital. (My new year's resolution is to take the stairs up to the 7th floor, rather than the lift. I'm regretting it today!!) The middle-grade on-call with me today catches up with my descending the stairs, followed by the acute medicine consultant for the day. At Raigmore, the arrest bleep alerts the on-call FY1 and middle-grade, the consultant on-call and also the anaesthetist. 8 When we arrive, there is already a team of nurses and two doctors from that ward attending to the patient. One doctor is managing the patient's airway, using a bag that can squeeze oxygen in via a mask. The other doctor is finding a vein on the patient's arm to out in a cannula (a tube that sits in a vein to deliver drugs/fluids). Two nurses are alternating cycles of chest compressions and another is preparing emergency drugs & placing ECG leads onto the patient. The on-call consultant takes the lead and help direct the team with their individual tasks, taking charge of the cockpit, as it were. The middle-grade starts reviewing the patient's notes and asking the ward staff about relevant information. That leaves me free to help gain further intravenous access for the patient, and to give any emergency drugs required. The anaesthetic team arrive too, and a full resuscitation plays out. Have a look at the resus council website for flow charts of the different types of resuscitation. http://www.resus.org.uk There are many reasons a cardiac arrest call is put out. It may not actually be an arrest but it is better to err on the side of caution. This time it is a cardiac arrest and the patient required some emergency drugs before their output returned. Following the resuscitation, the patient needs to be stabilised and transferred to the intensive care unit for close monitoring. Back to the 7th floor. New year's resolution broken already, and I take the lift. It's a chance to catch breath and briefly reflect. Back on the GI ward and it's time to start looking up results. As well as the ultrasound scan, I had also requested... A CT head scan for someone who we think had a minor stroke, a scan to see if a patient's blood supply to their liver had worsened... An echocardiogram and lung function tests to see how well another patient was doing, to help the physiotherapist's assessment. The person who had difficulty passing urine earlier had a normal renal ultrasound but had signs of a urine infection, so needs antibiotics. I write up the antibiotics after double-checking them in the hospital's guidelines (on my phone). 9 A few drug charts have run out of space so need re-writing. The ward pharmacist checks out our prescriptions too, for extra safety. We run through the list of jobs from today and make sure we haven't missed anything, then go to handover. As I'm on long-day ward cover, I take the handover from each ward today, making a list of jobs. Pretty quiet tonight actually! The middle-grades hand over anyone who is very unwell, including the patients in high-dependency. Making the evening team aware of very unwell patients, even if nothing specific needs doing, ensures continuity of care. After handover I head to the WRVS shop to grab a thin coke and monster munch, the staple diet of junior doctors. Where Raigmore triumphs over all other hospitals is that it sells Harry Gow's legendary cakes. Vital on long days. Dream ring anyone? My bleep goes off just as I finish the last bit of cream from the dream ring. Thankful for the sustenance, I head to the phone. A patient on the oncology ward, who is being treated for a blood cancer, has got a high temperature, so I need to review them. The nurse has recorded the patients SEWS (Scottish Early Warning Score) as 2, as they have a high temperature. The SEWS alerts us to acute changes which could signify new problems such as infection, and also show trends. Due to this patient's chemotherapy, their white blood cells are very low (neutropenia). White cells fight infection, so having very few makes someone very susceptible to overwhelming infection. We have a specific protocol for treating infection in people with neutropenia. It makes life easier for me as I can just follow the guideline! I do a full assessment & examination of the patient & review their notes to get a fuller picture, & note current plan. The patient feels fine, which is good. We know from evidence the sooner a patient gets antibiotics, the better they do. I explain that even though they feel fine now, they may have an infection brewing that could develop into a sepsis & become very sick. Whilst I'm putting a cannula in their arm, we discover we both have a love for the music of Sibelius after it comes on the radio. 10 After that we fall into a discussion about the symphony, Scandinavia, & swans! (Guess the piece, music buffs?) Although we're cut short by my bleep going off again. Another ward, another cannula. FY1s on medicine at Raigmore usually do one long day on-call each week. They can be quiet, sometimes boring, or really, really busy. Some have been really tough, either because of how busy I've been, or due to complex cases. There is always support though. On occasion, they can be sad. I've been called to a couple of patients who have died in the evenings. I have to confirm the patient is dead by examining them for signs of life, and record this in their notes. I then usually talk to the relatives. This can be quite upsetting at times, but I have learnt from observing the very best. On one evening shift, I had to tell a lady her husband was very likely to die that night. I'd observed a similar conversation the week before. The patient died later that evening, but a week later I received a thank you card from his wife for helping her though that time. Death and dying isn't always sad. I wrote a short story about a death on my previous ward. It was shared a lot online. It's called The Old Lovers, and shows that compassion is very much alive in our NHS. http://the5thleg.wordpress.com/2013/08/30/the-old-lovers/ That's all for tonight folks, thanks for following again today! Tomorrow will be full of guts, gore and bodily fluids!! @nhshighland Thursday Morning all! @fakethom here again. Hope nobody's been blown off in any storms this week. It's getting windy again this week! Thanks for all the superb feedback so far, I'm glad my twittery-thumbs have produced some interesting things so far. So this morning the consultant and registrar will do the ward round with our new medical student. Our student is in their final year, and so is essentially learning how to do the job now that the knowledge basis is there. They are going to have a go at being me on the ward round today, as I'm going to be getting my (gloved) hands mucky with procedures. 11 This morning I need to drain a build-up of fluid from a patient's abdomen. On the gastro ward, we commonly see patients with a condition called ascites. This is where the abdomen fills with fluid that shouldn't be there. The biology/physics behind ascites is pretty interesting, and fairly straightforward to grasp. Wikipedia it! Patients with liver or pancreatic disease are fairly susceptible to developing ascites. As fluid builds up in the belly, it becomes uncomfortable and can start impacting upon organ functions too. One of the ways we keep track of how ascites is building up is by regularly recording weight. 1kg weight ~= 1L of fluid. On yesterday's ward round, we predicted that one patient would need fluid drained this morning by looking at the trend in their weight. I pop into the patient's room to check they are still happy to have the procedure done. This patient has had to have quite a few drains like this before due to liver disease caused by excess alcohol consumption. Unfortunately the damage done to the liver is pretty irreparable so we can only manage this fluid build-up as best we can. As well as draining the fluid externally, we can try different tablets that affect storage of water and salts in the body to try shift fluid. I collect all the bits and pieces required for the procedure. There's lots to get out, but I think I've remembered everything! Working on the GI ward, I've lost count of how many drains I've inserted. My registrar taught me on my second day, then observed until I was competent. I gather the equipment required for the drain, plus stuff for a cannula in the arm, plus what I need for local anaesthetic. Everything is laid out on a metal trolley I can take to the patient's bedside. Everything on the trolley is sterile and mustn't be contaminated by touch. I used to work for the ambulance service so thankfully I'm used to working with a sterile field and using 'aseptic technique'. Even so I occasionally drop something or touch something sterile with a non-sterile hand and have then to get everything out from scratch! With the patient now and ready to start. First I put a small cannula into a vein in the patient's arm. 12 Thankfully the patient is in no way needlephobic, as the guide needle for the drain itself is huge. A good 12 inches. This is why I use an injection of local anaesthetic (using a MUCH smaller needle!) under the skin first. After examining the patient's abdomen, I clean the area thorough and visualise where I want to insert the drain. I inject local anaesthetic to the skin, and then to each layer of the abdominal wall beneath, along the path the drain will take. Once it takes effect, a very small incision in the outermost layer of abdominal wall with a scalpel will help the drain go in. Now we're ready for the big one. I've put the guide needle in to the drain, which is a plastic tube that will sit inside the abdomen. Smooth and quick is the best approach, I find. Once the guide needle takes the tube through the abdominal wall, I advance the drain & remove the needle. The one thing I forgot was to pre-clamp the attachment on the end of the drain. I quickly clamp it but not before getting gunk on my shoes! Some padded dressing to secure the drain and make it comfortable against the skin, and a 2L bag attached and we're all done. I take sample fluid to send to the labs for analysis, which is important to chase the results of in case there is any infection present too. One problem that can occur when draining fluid quickly from the body is the kidneys don't always have time to adjust. To protect against this, we can give infusions of albumin through the cannula I inserted before the procedure. The mechanism here is related to the reasons ascites develops in the first place. Again, Wikipedia it if interested. Remember osmotic gradients and semi-permeable membranes from school? All done, and the patient can get back to reading their book: The Thurber Carnival. An excellent collection of short stories, I highly recommend it! I tidy up the mess of used bits and pieces, plus wrappers and rubbish, then label and send off the samples to the labs. All in all it probably took about 30 minutes. The drain can stay in for up to 6 hours. Longer than that becomes an infection risk. 13 For this person we're aiming to drain 10L. Sometimes we aim for more, but here we want to be careful because of their kidney function. Afterwards, the patient may be able to return home if all else is well, and monitor their weight until they feel they need a further drain. I had two more of these drains to do this morning. This afternoon my registrar is going to teach me how to do a chest drain. The procedure is similar but for fluid surrounding the lungs. The reasons for build up of chest fluid are similar too. A chest drain is a tad more complicated due to the pressures in the chest affecting breathing, and requires some clever three ways drains. As a junior doctor, there's always something new learn. It's impossible to know everything in medicine! Whilst I'm being taught new skills, I'm also starting to teach the skills I have ready started developing. After the ward round has finished, our medical student assists me with another ascitic drain. The Aberdonian students are an excellent bunch! *Almost* as good as the ones from Brighton of course...not that I'm biased of course. As a medical student and as a junior doctor, you will develop a high tolerance to gross-ness. Blood, vomit, diarrhoea, and other miscellaneous squirts of bodily fluids. It all comes flying your way. I say embrace it. Perhaps ascitic-fluid speckled shoes could be the next big thing... I'm also a great lover of a good mess. I don't think there anything more fun than making a mess actually. It's one of the reasons I love being involved with @overthewallcamp - mess is always encouraged! Here's a little adventure story I wrote about a wonderful example of how mess can be therapeutic for kids. http://the5thleg.wordpress.com/2013/10/28/harri-and-his-food-fight/ That's pretty much all for today's tweets folks. Amongst other things, I'll try touch upon a few bits & bobs for those considering doctor'ness. I'll leave you with this: I think there can be a common misconception about the type of person, or background, needed to be a doctor. Anyone can be a doctor if they really want to be: http://the5thleg.wordpress.com/2013/07/08/theim-a-doctor-first-time/ Thanks for reading. Tweet me @fakethom with any questions/comments. Goodnight! 14 Friday Hello all! I trust you've all had fantastic weeks, and if not, then at least it's the weekend! We share a ward with the renal team. I've stuck this to their jobs book as a present for Friday. pic.twitter.com/uoZz8adTVV So far this week we've had a peek at a consultant ward round, a junior round, organising bits & bobs, some emergencies, & some procedures. Today I thought I'd fill in the gaps with the other things required of junior doctors in training, and our place in the grand scheme of things. One thing I haven't touched on much, but is an inevitable part of the job is the subject a bad news, death & dying. Not the cheeriest topic for a Friday morning... But thinking about death & dying meaningfully, & approaching it sensitively is key to providing good care. @Palliative_Scot @LifeDeathGrief When a patient dies, they are still your patient, & you still have a duty of care towards them, which extends to the patient's family/friends. On my ward, we have some very unwell patients. Many have a good chance of recovery, even if it will take time. But of course, we have patients who are not going to survive, despite the best efforts of all involved. In the 6 months I've been at Raigmore, I've had a lot of teaching about death & dying, & experienced a lot of excellent end of life care. There is an excellent palliative care team who are experts in everything to do with end of life care. They are on hand to help make the last weeks/days/hours of somebody's life as comfortable as possible. There are lots of things to consider regarding end of life care for a patient. The basic physical needs of the patient need to be considered, and there are some effective drugs to combat some 'side effects' of dying. There is a wealth of advice about end of life care in our book of drugs and guidelines, The Highland Formulary. The real saviours when it comes to death and dying are the palliative care nurses. They never cease to amaze me at how much comfort they can bring to a patient. The palliative care team, especially, show just how important the psychological and spiritual side of care is in such circumstances. 15 When one of the palliative care nurses arrives on the ward, it's as if a layer of calm descends and I know all will be well. The other thing an FY1 often has to do is confirm death when a patient dies. It involves checking thoroughly for signs of life. We have a shadowing week before starting FY1 at Raigmore. The doctor I was shadowing had to confirm a death on the first day. As she went through the examination, she spoke to the patient as she would if he were alive. It was very touching. I've since emulated this in my own practice. Once confirmed, the death needs to be recorded in the patient's notes and a certificate filled out with cause(s) of death. When writing in the patient's notes, I end the entry with "May they rest in peace". Unless there are other issues, it's the last line to be recorded in the notes. I think it's kinder than just writing "time of death..." I picked that tip up from the ever-excellent @themattmak and stuck with it ever since. Discussions on the subject with relatives, and breaking bad news, is something I think pretty much all FY1s fear. It's good to observe people breaking bad news and having such discussions as much as possible to learn the best ways of doing it. I've been placed with some really incredible people in this respect and I'm starting to get a feel for what I imagine is something that takes a lifetime to master. I could tweet for hours about death and dying (I won't!). I find it really interesting. I think, to me, it forces perspective, reflection and contemplation, which are all good things. I've met many doctors and nurses at Raigmore who I aspire to be more like in the way they approach end of life care. I mention this all today as one of our patients who has been with us a while died during the night. They died peacefully after gradual deterioration from effects of chronic liver disease. Start the morning by completing a death certificate. As it was during the night, the phenomenal night nurse practitioners were on-hand to make sure the patient was as comfortable as possible. Raigmore's Night Nurse Practitioners are one of its greatest assets, and an invaluable source of support & guidance for junior doctors. 16 Teaching is a big part of life as an FY1, whether formal teaching, or (more commonly) learning through experience & discussion. In the afternoon, I observe a couple of medical students practice their clinical examinations of the chest and abdomen. I was always a bottom-of-barrel kind of medical student, so it can feel a bit strange teaching final year medical students. The tips I try and impart to the medical students are based more on coping with the day-to-day job... Tips about how to take blood from patients with tricksy veins, or the best way to look up information. I suppose I can't go through a 'week in my life' without mentioning the dreaded ePortfolio that all doctors have to do in some form. It essentially an online log of achievements and development, with space to reflect on various events. I know a lot of people who shudder at the word 'reflection' (and not all of them are vampires). Thanks to my experiences with the wonderful @overthewallcamp I find reflection a really interesting concept. At camp, we use reflection as a key tool to help children affected by serious illness break away from barriers cause by illness. Facilitating reflection in kids has given me an appreciation for how I myself reflect on things and the value it can bring. It's one of the many reasons the charity has shaped the person I try to be today. I wrote this about Reflection For Kids: http://the5thleg.wordpress.com/2013/11/06/reflection-forkids/ To be honest, the themes I've covered with tweets each day this week actually mostly all occur on a daily basis. Whilst life as a junior doctor is hectic and non-stop, it's largely immensely enjoyable. You never know what's coming at you next! The compassion and kindness I see around me on a daily basis at work is incredible and is a large part of why I enjoy the job so much. That and the view! pic.twitter.com/jNBEaa8jTY For anyone considering a life in healthcare, whatever job that may be, I think there are two key things required: one is empathy... 17 ...and the other, in the words of J.M. Barrie, is the ability to always be a little kinder than is necessary. For anyone interested, I wrote this about how empathy can't be taught, but can be inspired. http://the5thleg.wordpress.com/2013/11/10/the-standing-ovation/ And that's about it for the week! I haven't managed to write enough tweets to cover Saturday and Sunday as I've run out of hours in the day! But I'm hoping I'm invited back to tweet about what doctors do when they work at weekends! Thank you all for showing such an interest! It's been an absolute pleasure to tweet for @NHSHighland - any comments/questions to @fakethom Here are the #storify collations for each day: Monday: http://storify.com/fakethom/nhs-highland-who-we-are-fakethom-monday Tuesday: http://storify.com/fakethom/nhs-highland-who-we-are-fakethom-tuesday Wednesday: http://storify.com/fakethom/nhs-highland-who-we-are-fakethom-wednesday Thursday: http://storify.com/fakethom/nhs-highland-who-we-are-fakethom-thursday Friday : http://storify.com/fakethom/nhs-highland-who-we-are-fakethom-friday 18