Low-Cost Transitional Care with Nurse Managers
advertisement

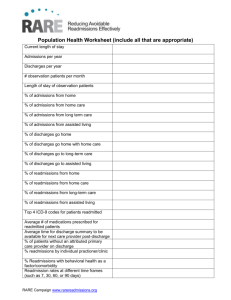
Low-Cost Transitional Care with Nurse Managers Making Mostly Phone Contact with Patients Cut Rehospitalization at a VA Hospital Point of Contact: Mr. James Butera, james.e.butera.civ@mail.mil Group Involved with the Project: William S. Middleton Memorial Veterans Hospital, in Madison, Wisconsin Submitted by James Butera 13 May 2014 Executive Summary: The Coordinated-Transitional Care (C-TraC) Program is structured to improve care coordination as the patient transitions from the inpatient to the outpatient setting. The implementation occurred at the William S. Middleton Memorial Veterans Hospital, in Madison, Wisconsin. The foundation of the program focuses on nurse case managers proactively working with patients starting in the inpatient setting and continuing after discharge, primarily through telephonic communication. A total of 708 patients enrolled in the programs which resulted in correcting 639 medication discrepancies, reduced 30 day rehospitalization rates by 11% producing an estimated cost of care savings of $1,225 per patient net of programmatic costs (Kind, et al., 2012). This model requires a relatively small amount of resources to operate and may represent a viable alternative for hospitals seeking to offer improved transitional care as encouraged by the Affordable Care Act. 1|Page Objective of the Best Practice: Proper transitional care from the inpatient setting to the community setting improves patient outcomes, reduces readmissions and corrects potentially fatal medication discrepancies. Additionally, the C-TraC program strengthens the patientcentered medical home model. Based on Coleman’s Four Pillars of transitional care, C-TraC aims to educate and empower the veteran/caregiver related to medication management; ensure proper follow-up; educate veteran/caregiver about pertinent “red flags”; and the proper person to contact for concerns during the transitional care period (Kind, et al., 2012). Background: The Department of Veterans Affairs (VA) restructured the delivery of primary care through the development of Patient Aligned Care Teams (PACT) based on the patientcentered medical home model. While the enrolled C-TraC population primarily consists of veterans with high-risk conditions that would benefit from home health assistance, the PACT workflow prevents home visits. To address this issue, as well as the challenges associated with serving a large geographic region, the Madison VA created C-TraC as a clinical quality improvement program. Section 3025 of the Affordable Care Act established the Hospital Readmissions Reduction Program, requiring CMS payment reductions to IPPS hospitals with excess readmissions, effective for discharges beginning on October 1, 2012 (Centers for Medicare & Medicaid Services, 2013) which served as another impetus for the C-TraC program. Literature Review: There exists an abundance of current literature that addresses the ramifications associated with hospital readmissions. It is proven that they are not only costly from the business operations perspective; they also have a correlation between increased morbidity and mortality (Parker & Griffith, 2013). According to Benbassat and Taragin, approximately 9% to 48% of all readmissions are associated with poor quality care indicators and, therefore, are preventable (2000). Primary indicators included “poor resolution of the main problem, unstable therapy at discharge, and inadequate post-discharge care” (Benbassat & Taragin, 2000). While current literature addresses numerous processes and interventions aimed at improving the transition of care and decreasing readmissions, there exists no consensus as to which modalities are universally successful. Multiple articles cite a multidisciplinary, multifaceted approach to obtaining improvement in these areas. Three studies in the January 2013 Journal of American Medicine depict the trials of navigating through the health care delivery system while transitioning among hospitals, emergency departments and homes especially for patients with chronic conditions. “Too often the ED serves as a source of outpatient follow-up (40% of all hospital-based, acute care use during the post-discharge period according to their findings), compounding the problems of ED overcrowding” (Williams, 2013). Failure to provide optimal transition from the hospital setting to the home environment often results in adverse medical outcomes, readmissions, and sometimes death. Discharge from the hospital after acute care intervention does not necessarily equate to resolution of the reason for admission nor does it prevent medication errors. Approximately 20% of medical patients discharged from the hospital setting sustain a preventable adverse event (AE) within 3 weeks of discharge. Several factors negatively impact care transition: 1) inadequate communication between inpatient and outpatient providers; 2) medication discrepancies; 3) insufficient patient education related to diagnosis, medications, warning signs, and follow-up requirements; and 4) premature discharge form the hospital to identify a few (Rennke, et al., 2013). In 2012, Hesselink et al. conducted a literature review over 1162 citations related to interventions aimed 2|Page at improving patient discharge from hospital to primary care. Twenty of the 27 studies specifically focused on care coordination efforts which show statistically relevant improvement in appropriate primary care use, patient health status, hospital use for care, and continuity of care. The studies recognized organized post-discharge follow-up services; structured discharge planning processes; and early assessment of follow-up requirements as key components of successful transition of care (Hesselink, et al., 2012). Coordinated care efforts and early primary care involvement optimize patient post-discharge outcomes and reduce the amount of readmissions within 30 days of the acute care hospitalization. Implementation Methods: Launched in April 2010, the C-TraC program focused on veterans who were considered high risk for negative post-hospital outcomes and who were discharged to non-institutional community settings. Requirements for participation included a diagnosis of 1) dementia, delirium, or other cognitive impairment or 2) being 65 years or older, living alone, with a hospitalization within the last year. Figure 1 below graphically depicts the protocol CTraC implemented. Figure 1. 3|Page Results: A total of 708 veterans enrolled in the program from the April 1, 2010 start through March 31, 2012. Of the 605 intervention-period enrollees 47% had a medication discrepancy (639 total) identified and corrected and a 11% average reduction in readmissions (see Figure 2). This reduction corresponds to 408.7 prevented hospital days equating to a cost avoidance of $966,167 over the 18 month period or $1,225 per enrollee (Kind, et al., 2012). Thirty Day Rehospitalization Rates 50% Baseline 43% 45% Intervention 40% 35% 31% 30% 25% 24% 24% Q3 Q4 25% 22% 22% 22% Q5 Q6 Q7 20% 15% 10% 5% 0% Q1 Q2 Q8 Figure 2. Conclusion: The C-TraC program provides an adaptable framework for the MHS to use to reduce medication discrepancies, reduce hospital readmissions, and improve the patient care experience and health outcomes. Through the Army’s Patient Centered/Solider Centered/Community Based Medical Home current staffing model, the nurse case manager (NCM) could perform the duties required in the same manner as NCMs at the Madison VA. Adoption of this model or a similar protocol-driven model will result in significant cost savings through reduced hospital readmissions and will improve patient outcomes through medication discrepancy corrections and improved transitional health care delivery. 4|Page References Benbassat, J., & Taragin, M. (2000). Hospital Readmissions as a Measure of Quality of Health Care: Advantages and limitation. Archives of Internal Medicine, 160(8), 1074-1081. doi:10.1001/archinte.160.8.1074 Centers for Medicare & Medicaid Services. (2013, August 2nd). Readmission Reduction Program. Retrieved November 13th, 2013, from cms.gov: Centers for Medicare & Medicaid Services: http://www.cms.gov/Medicare/Medicare-Fee-for-ServicePayment/AcuteInpatientPPS/Readmissions-Reduction-Program.html Hesselink, G., Schoonhoven, L., Barach, P., Spijker, A., Gademan, P., Kalkman, C., . . . Wollersheim, H. (2012, September 18). Improving Patient Handovers From Hospital to Primary Care: A systematic review. Annals of Internal Medicine, 157(6), 417-428. Kind, A., Jensen, L., Barczi, S., Bridges, A., Kordahl, R., Smith, M., & Asthna, S. (2012). Lowcost Transitional Care With Nurse Managers Making Mostly Phone Contact With Patients Cut Rehospitalization At a VA Hospital. Health Affairs, 31(12), 2659-2668. doi:10.1377/hltaff.2012.0366 Parker, C., & Griffith, D. (2013, April). Reducing Hospital Readmissions of Postoperative Patients With the Martin Postoperative Discharge Screening Tool. JONA: The Journal of Nursing Administration, 43(4), 184-186. doi:10.1097/NNA.0b013e3182895902 Rennke, S., Nguyen, O., Shoeb, M., Magan, Y., Wachter, R., & Ranji, S. (2013). Supplement, Making Health Care Safer: A critical review of evidence supporting strategies to improve patient safety. Annals of Internal Medicine, 158, 433-440. Williams, M. (2013, January). A Requirement to Reduce Readmissions: Take care of the patient, not just the disease. Journal of American Medical Association, 160(8), 394-396. doi:10.1001/archinte.160.8.1074 5|Page