Partnering to Avoid Hospital Readmissions
advertisement

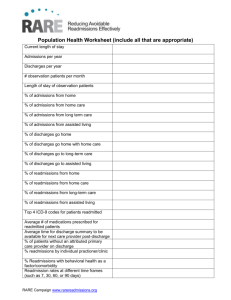
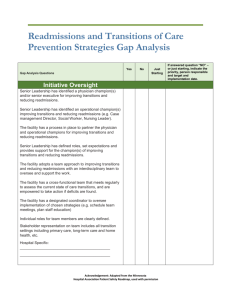
Kathy Cummings, RN, BSN, MA Institute for Clinical Systems Improvement Janelle Shearer, RN, BSN, MA Stratis Health George and Martha What is happening? What is the Impact? • Almost 20% of Medicare patients in Minnesota are readmitted within 30 days of discharge • Huge opportunity to fix gaps in fragmented system • Reduce unnecessary burden on patients, families • Preventable readmissions are contributing to unsustainable climb in health care costs • CMS penalties for low-performing hospitals – “clock” begins ticking Oct. 1, 2011 The RARE Campaign • A campaign across the continuum of care to reduce avoidable hospital readmissions across Minnesota and surrounding areas • Regional approach, supported by hospitals, providers, health plans, other key stakeholders • Campaign is engaging other care providers, acknowledging that readmissions are the result of a fragmented health care system Triple Aim Goals • Population health – Prevent 4,000 avoidable readmissions within 30 days of discharge OR in other words, • Care experience – Recapture 16,000 nights of patients’ sleep in their own beds instead of in the hospital – Improve by 5% on HCAHPS survey questions on discharge • Affordability of care – Save an estimated $30 million for commercially insured patients; additional savings for Medicare patients Broad Community Support • Operating Partners: • Institute for Clinical Systems Improvement (ICSI) • Minnesota Hospital Association (MHA) • Stratis Health • Supporting Partners: • Minnesota Medical Association • MN Community Measurement Broad Community Support • Community Partners: – Endorse and actively support the campaign • A growing list of providers, health plans, state health agencies, home health agencies, nursing homes, patient advocacy groups and other community organizations Five Focus Areas • Comprehensive discharge plan • Effective communication for transitions of care • Engagement of patient and family in discharge process • Medication management • Transition care Support for Organizations • • • • • • • Best practice toolkits Face-to-face sessions Webinars Conference calls Peer coaching Data reporting “Innovator” approach: intensive, rapid process improvement work Analysis and Measurement • MHA Potentially Preventable Readmissions (PPR) data used to establish each hospital’s goal • Progress monitored with quarterly PPR results • Hospitals collect data on variety of process measures; report their progress Long Term Care Monitoring and Measuring Readmissions: Developed by the Long Term Care Committee of the RARE Campaign as a tool to help nursing facilities calculate two types of rehospitalization measures: • The Minnesota Department of Human Services Re-Hospitalization Measures • Other Re-Hospitalization Measure Why Track to Reduce Readmissions? • Reduce the burden on patient, family and staff • Reduce costs • Improve quality and target improvement activities • Accountability For more on long-term care, vist the RARE Campaign website What can long term care do? • Collect your data • Analyze your data • Analyze each readmission for opportunities for improvement – which of the five focus areas contributed to the readmission? • Analyze your care for each of the five focus areas • Begin quality improvement projects to reduce readmissions and include your community partners – hospital, pharmacy, etc. What can long term care do? • • • • • Medication Management Comprehensive Discharge Plan Patient and Family Engagement Care Transition Support Care Transition Communication www.RAREreadmissions.org 16,000 Nights At Home Will Make Our Day. Thank You For Helping Everyone Sleep More Peacefully. Questions? www.RAREreadmissions.org Thank you. kathy.cummings@icsi.org jshearer@stratishealth.org