presenters` profiles
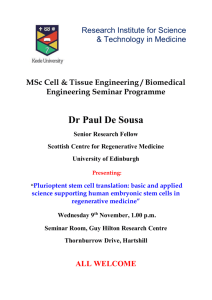
advertisement

PRESENTERS’ PROFILES Juan Carlos Izpisua Belmonte graduated from the University of Valencia, Spain and received his Ph.D. from the University of Bologna, Italy and the University of Valencia, Spain in 1987. After postdoctoral stages at the EMBL in Heidelberg, Germany, and UCLA, Los Angeles, USA, in 1993 he moved to the Salk Institute for Biological Studies in La Jolla, California where he is currently a professor in the Gene Expression Laboratories. Since 2004 he is also the Director of the Center of Regenerative Medicine in Barcelona. His key scientific interests include the establishment of organ left-right asymmetry, limb and heart development, and stem cell biology and regeneration. He has received several notable honors and awards, including the William Clinton Presidential Award, the Pew Scholar Award, the National Science Foundation Creativity Award, the American Heart Association Established Investigator Award, and the Roger Guillemin Nobel Chair for his endeavors in these fields. Dr. Izpisua Belmonte has been at the forefront of developmental biology research. He has published over 300 articles in high profile, internationally recognized, peer reviewed journals and book chapters. Through the years he has produced novel, groundbreaking results, such as uncovering the role of some homeobox genes in limb patterning and specification, as well as the identification of the molecular mechanisms that determine how the different cell type precursors of internal organs are organized spatially along the embryonic left right axis. Furthermore, his work has started to give us a glimpse into the molecular basis implicated during organ regeneration in higher vertebrates, the differentiation of human stem cells into various tissues, and the molecular basis underlying aging and somatic cell reprogramming. Dr. Gustavo Mostoslavsky received his M.D. from the University of Tucuman in Argentina and his Ph.D. from the Hebrew University in Jerusalem, Israel. His longstanding interest in basic science and regenerative medicine brought him to Harvard Medical School to pursue postdoctoral studies with stem cells and gene therapy. Dr. Mostoslavsky is currently Assistant Professor of Medicine in the Section of Gastroenterology in the Department of Medicine at Boston University School of Medicine. His main research interests are stem cells, disease modeling, regenerative medicine, gene correction and lentiviral vectors as tools for gene transfer. Dr. Mostoslavsky is a founder and Co-Director of the BU Center for Regenerative Medicine (CReM). The Mostoslavskyr lab has a major interest in the study of induced Pluripotent Stem cells or iPS cells and the development of tools for their generation and characterization. Pioneering work by the laboratory of Dr. Yamanaka showed that fibroblasts transduced with retroviral vectors expressing four transcription factors, Oct4, Klf4, Sox2 and cMyc can be reprogrammed to become pluripotent stem cells that appear almost indistinguishable from ESC. In contrast to ESC, iPS cells are genetically identical to the individual from whom they are derived, raising the prospect of utilizing iPS cells for autologous cell based therapies without risk of rejection. We have previously developed a single lentiviral vector expressing a stem cell cassette, named STEMCCA, capable of generating iPS cells from post-natal fibroblasts with the highest efficiency reported to date. We have recently modified it to make it excisable and have used it to generate mouse and human iPS cells free of exogenous transgenes. We aimed at using iPS cells in parallel to ESC for the study of endoderm/intestinal lineage specification, as well as for disease modeling and their potential for regenerative medicine. We are currently establishing and characterizing iPSC lines from several GI tract related diseases, including Familial Adenomatous Polyposis (FAP), Crohn’s disease and Hemochromatosis. Dr Sebastian Carotta Dr Sebastian Carotta 2011 – Current: Group Leader at The Walter & Eliza Hall Institute Email: carotta@wehi.edu.au 2007 – 2010: Senior Post-doctoral fellow at The Walter and Eliza Hall Institute for Medical Research, Melbourne, Australia 2004 – 2007: Post-doctoral fellow at The Walter and Eliza Hall Institute for Medical Research, Melbourne, Erwin Schroedinger long term fellowship 2003 – 2004: Post-doctoral fellow at the Research Institute of Molecular Pathology, IMP, Vienna 2000 – 2003: PhD thesis on “Characterization of ES cell derived Erythroid Progenitor Cells” in the group of Dr. Hartmut Beug at the Research Institute of Molecular Pathology, IMP, Vienna, Final Exam: September, 2003, (passed with distinction; “Auszeichnung”) Research Overview Common cancer therapies are often non-specific and ineffective in eradicating the cancer. To understand the mechanisms of how cancers arise and design more effective targeted therapies, a better understanding of how normal cell development is regulated is required. The haematopoietic (blood) system due to its hierarchical organisation is an ideal system to study tissue development from normal stem cells and the formation of neoplasms such as leukaemias and lymphomas. Differentiation of haematopoietic stem cells (HSC) and progenitors is under the strict control of a regulatory network orchestrated by the activity of key transcription factors. Detailed knowledge of these transcriptional networks is essential for a better understanding how blood homeostasis is regulated and how alterations in these networks lead to diseases such as cancer. The main focus of our group is to understand how haematopoietic stem cell self-renewal versus lineage commitment is regulated on the molecular level and which pathways are critically dysregulated in the formation of leukaemias. To address these questions we are employing a range of different model systems such as mouse models, mouse and human embryonic stem cells. Research Interests Transcriptional regulation of haematopoietic stem cell development Natural killer cell development Red blood cell development Epigenics – a different direction A UNSW-affiliated researcher is one of six young people awarded grants to find new ways to help prevent and treat cancer. Dr Phillippa Taberlay, who is a conjoint senior lecturer in UNSW Medicine based at the Garvan Institute of Medical Research, has been given an Early Career Development Fellowship through the Cancer Institute NSW. The three-year $587,877 fellowship will allow Dr Taberlay to pursue her work in epigenetics, the study of heritable biochemical marks that are placed along the DNA without altering the underlying sequence. The work will initially look at prostate cancer cells. While epigenetic defects are involved in cancer development, they are also potentially reversible and Dr Taberlay says her work could ultimately expand the benefit of existing drugs that have proved to be very successful in treating leukaemia patients. By unlocking any hidden potential of an already existing therapy, this could mean that patients may have access to a different treatment, that is already known to be safe, relatively quickly. Dr Taberlay says her team will be one of the first to try to understand how epigenetic changes impact on the 3D structure of DNA and vice versa. The researchers will specifically map the 3D structure of DNA and ask whether this is different between normal and prostate cancer cells. We are just beginning to understand how important the 3D structure of our DNA actually is. One reason is that it ensures that genes are expressed as they should be by physically bringing critical gene control centres together inside cells so that they can interact," she says. "We are using sophisticated techniques to map these 3D loops to determine whether there is a difference between normal and prostate cancer cells, and how it may drive disease.” The team will also test whether a next-generation epigenetic therapy can be used to treat the prostate cancer cells, restoring a more normal 3D structure. The work could be an important step forward to the goal of personalised medicine. “Genetic and epigenetic cancer research has enabled us to see that not all cancers are the same," she says. "We hope to use the new types of knowledge from this study in the future to determine whether a patient has a certain sub-type of a particular cancer, which may allow us to tailor their reatment and give them the best chance of survival.” Associate Professor Ernst Wolvetang is a stem cell researcher who leads the Stem Cell Engineering Group at the Australian Institute for Bioengineering and Nanotechnology. His team of researchers uses novel cutting-edge inter-disciplinary approaches to understand the complex molecular mechanisms that govern human pluripotent stem cells. This knowledge is then used to develop novel methods to generate and expand pluripotent stem cells and direct their differentiation into cell types that can be used in regenerative medicine and drug screening Research The major obstacles that currently inhibit the application of patient specific stem cell based regenerative therapies are a) the low efficiency of reprogramming somatic cells, b) the effect of modifying the genome and epigenome during reprogramming in relation to the long term safety of stem cell grafts, c) the costs associated with generating iPS cells and differentiating such stem cells to the relevant progenitor cells and d) the lack of a cost effective platform for expansion of stem cells and progenitors . Combining advanced cell biology, nanotechnology and microfluidics approaches will be able overcome many, if not all, of these hurdles. Associate Professor Wolvetang’s Stem Cell Engineering Group (SCEG) is presently focusing on four major areas: Unravelling the processes that control the genetic and epigenetic stability of induced pluripotent stem cells, so as to ensure their long-term safety. The development of micro-fluidic screening platforms for small molecule-based differentiation of pluripotent stem cells into neuronal and cardiac cell lineages and for drug screening purposes. Understanding the fundamental processes that control pluripotency and lineage-specific differentiation, including the micro-environment. To achieve these aims the SCEG combines cutting-edge molecular biology techniques, high content screening tools, transcriptome and Chromatin immuno-precipitation (CHIP) analyses and cell biology. The research program in the SCEG closely interfaces with other disciplines within the AIBN such as smart-surface chemistry, microfluidics, bioinformatics and nano-particle development. The efficient and cost-effective generation of patient and disease specific induced pluripotent stem (iPS) cells. Research Projects Developing novel cell reprogramming technologies; Generating Down Syndrome iPS cells to understand Alzheimer’s disease; Understanding epigenetic control over differentiation and genetic stability; Elucidating BMP-SMAD signalling in human stem cells; Metabolic analysis of human embryonic stem cells; Developing smart surfaces for stem cell expansion and differentiation. Dr Andrew Laslett is a Research Group Leader at CSIRO Materials Science and Engineering , where he leads a human pluripotent stem cell biology research group. He also holds an Adjunct Associate Professor position with the Department of Anatomy and Developmental Biology at Monash University and is an Honorary Senior Fellow with the Department of Zoology at Melbourne University. Since 2001, he has focused on elucidating the complex biology of human embryonic stem cells (hESC), examined methods for the differentiation of hESC to renal progenitor cells and more recently begun comparing hESC to reprogrammed human cells termed induced pluripotent stem (iPS) cells. His laboratory is currently focused on exploiting the basic biology of these cell types to create novel cell lines and tools that enhance human pluripotent cell research translation within CSIRO, Australia and internationally Dr Sharon Ricardo is Group Leader, Kidney Stem Cell and Regeneration Laboratory and Director, MBio Graduate School, Monash University Research interests The Kidney Regeneration and Stem Cell Laboratory at MISCL, Monash University focuses on the development of stem cell-based therapies and/or growth factors that may repair damaged kidney tissues and reverse the development of scarring, thereby reducing the need for kidney dialysis or organ transplantation Ongoing projects include: Pluripotent stem cells from patients with kidney disease We have recently derived iPS cells from human kidneys (Song et al, JASN 2011) and are currently generating iPS cells from patients with genetic kidney disease including polycystic kidney disease and Alports Syndrome. These iPS lines that maintain the disease genotype and phenotype, will be used for disease modeling and screening new and existing drug compounds that will offer alternatives to the limited framework of prevailing clinical options. The long-term objective is to developiPS cells as a method to produce differentiated human kidney cell types in sufficient quantities that can be used in high-throughput in vitro toxicity screens and ultimately cell therapies for patients with chronic kidney disease. Immune modulation and bone marrow-derived cells in kidney repair This research is focused on the development of strategies to promote kidney ‘self-repair’ and the monocyte/macrophage phenotypesthat are important in this process. As we have recently reported (Alikhan et al. Am J Pathol 2011)macrophages are critical regulators of tissue homeostasis, providing an essential role during organogenesis and adult tissue repair. We are interested in the processes underlying inflammation and repair that are driven by macrophages/monocytes. Understanding the heterogeneous nature of myeloid cells and the supporting stromal cells during inflammation and tissue repair provides the means to identify, recruit and polarise desirable populations, and raises new and exciting therapeutic possibilities to attenuate or conceivably reverse progressive renal disease. Dr Jose Polo is Group Leader of the Reprogramming and Epigentics Laboratory at Monash University. Jose Maria Polo was born in Buenos Aires, Argentina where he graduated from Buenos Aires University as a Biochemist. In 2002, Jose began his graduate studies at Albert Einstein College of Medicine, New York under the UniversityUIniUniversityUniversityand Stem Cell Laboratories (MISCL), Monash University supervision of Dr. Ari Melnick where he worked on the transcriptional mechanism of the BCL6 repression complex in lymphomagenesis and B-cell maturation. In 2008 he obtained his PhD and moved to Boston to the laboratory of Dr. Konrad Hochedlinger at the Harvard Stem Cell Institute to work on reprogramming of adult cells into induced pluripotent stem (iPS) cells. In particular, his work focused in the acquisition of immortality and the existence of epigenetic memory during reprogramming. In June 2011 as a Larkins Fellow, Jose established his independent research group at Monash University. In 2012, Jose was awarded a NHMRC Career Development Fellowship to continue his work in reprogramming and epigenetics. As of 2013, Jose holds appointments to the departments of Anatomy and Developmental Biology and to the Australian Regenerative Medicine Institute. Lab interest The laboratory is interested in the transcriptional and epigenetic mechanisms that govern cell identity, in particular pluripotency and the reprogramming of somatic cells into induced pluripotent stem (iPS) cells. We are particularly interested in the following aspects: 1) The kinetics and universality of the epigenetic and genomic changes occurring during reprogramming. 2) The composition and assembly kinetics of transcriptional regulation complexes at pluripotency genes. 3) How the cell of origin influences the in vitro and in vivo plasticity potential of cells generated during the reprogramming process. 4) The epigenetics changes occurring in adult stem cells as a consequence of changes in their environment. Polo et al, “A molecular roadmap of reprogramming somatic cells into iPS cells.” Cell. 2012 Dec 21;151(7):1617-32. Dr Melissa Little is Group Leader, IMB Kidney Research Laboratory, Institute for Molecular Bioscience, The University of Queensland; and NHMRC Principal Research Fellow Hansson et al., “Highly coordinated proteome dynamics during reprogramming of somatic cells to pluripotency” Cell interests Reports. 2012 Dec 27;2(6):1579-92. Research The prevalence of Chronic Kidney Disease is climbing at 6-8% per annum with diabetic nephropathy now the leading cause of chronic kidney disease in most developed nations and some developing nations. Despite this, treatment Arnold et al., “Sox2(+) adult stem and to progenitor cells important tissue regeneration options remain restricted transplantation and are dialysis. Professor for Little'sresearch laboratory focuses on the development of alternative therapeutic through advanced understanding of the normal processes of kidney and survival of mice. Cell Stem Cell. 2011 Octoptions 4;9(4):317-29. development, injury and repair.. The kidney not regarded as a highly regenerative organ. Indeed, the functional filtration units of the kidney are all formed by time you reach Ohi etisal., “Incomplete DNA methylation underlies a transcriptional memory ofthesomatic birth. Hence, research is focussed on a number of approaches. The first is to investigate adult kidney mesenchymal stem cell populations so as to cells inwhat human cells. Nat Cell 2011 investigate role theseiPS cells play in regulating normalBiology. responses to injury andMay;13(5):541-9 how they might be able to improve repair. The other approach is Polo to look atet directed ES/iPS cells or reprogramming adult cells to the nephron stemfunctional cell state of the properties developing kidney, al., differentiation “Cell typeof of origin influencesofthe molecular and offrom where the hope is to be able to generate new nephrons mouse induced pluripotent stem cells. ” Nature Biotechnology. 2010 Aug;28(8):84855. Utika and Polo et al., “Immortalization eliminates a roadblock during cellular