Reporting of Quarterly Outpatient Activity Information: Data

Reporting of Quarterly Outpatient
Activity Information
Data Definitions and Guidance
Document
Version 12 (July 2015)
2
Contents
Page No.
1 Background 4
2 Definitions 5
3 Collection of data 8
- Outpatient Activity
8
- Peripheral Outpatient Services
9
- Reasons for Cancellation: Regional and
Sub-Regional Codes
10
4 Reporting of data 11
- Section 1.1 - Outpatient Activity
11
- Section 1.2 - Reasons for Cancellation of 12
Appointments
- Schedule 12
5 Data Validation 13
6 Data Use 14
7 Contact details 15
8 Appendices 16
3
1 BACKGROUND
The Quarterly Outpatient Activity Return, the present methodology for the collection of consultant-led outpatient activity, was introduced as a direct result of a comprehensive review undertaken in 2007/08. Primarily the methodology changed from a count of clinics to a count of appointments, and was subject to a National Statistics public consultation. The recommended changes in the methodology were endorsed and the QOAR was introduced from the beginning of 2008/09.
The QOAR relates to total face to face consultant led outpatient activity at each Health and
Social Care hospital in Northern Ireland.
A new version of the QOAR was introduced at the beginning of 2014/15, with the main change being that ward attendances seen by a consultant are now reported in the return separately and are not included in the main outpatient activity, as was the case in previous years.
Virtual activity (see definitions) was also previously included within the QOAR. However, following the issuing of virtual activity guidance by the Health and Social Care Board (HSCB) at the beginning of 2015/16, HIB introduced a separate return, the V-QOAR, to allow the monitoring of virtual activity. All terminology in the following guidance should therefore be taken to refer to face to face appointments only, unless otherwise specified.
Section 1.1 relates to outpatient attendances, patient cancellations of outpatient appointments
(CNA), outpatient appointments which the patient did not attend (DNA), hospital cancellations of outpatient appointments, ward attendances seen by a consultant and outpatient appointments cancelled as the result of a patient’s death. Section 1.2 relates to hospital and patient cancellations of outpatient appointments split by the reason for cancellation.
The variable ‘reason for cancellation’ was introduced in 2008/09 as experimental statistics and was only made mandatory for completion from March 2013. Following this decision, an audit of the reasons for cancellation was undertaken and an updated methodology was put in place. All
HSC Trust implemented this methodology from 1 st
July 2013.
The return is populated by activity data extracted from the Outpatients Universe universe of the
HSC Data Warehouse using Business Objects queries developed by the Department and HSC
Trusts. This data is supplemented by any activity not currently recorded on HSC Trust’s Patient
Administration System (PAS).
Data on attendances at accident and emergency departments in Northern Ireland should be reported on the KH09 (Part 2) data return.
4
2 DEFINITIONS
OUTPATIENT SERVICES – An outpatient service is a consultant led service provided by
Health and Social Care Trusts to allow patients to see a consultant, their staff and associated health professionals for assessment in relation to a specific condition. Patients are not admitted into hospital for this assessment. Outpatient services are usually provided during a clinic session providing an opportunity for consultation, investigation and minor treatment. Patients normally attend by prior arrangement. Although a consultant is in overall charge, they may not be present on all occasions the clinic is held. They must, however, be represented by a member of their team.
OUTPATIENT APPOINTMENTS – An outpatient appointment is an administrative arrangement enabling patients to see a consultant, their staff and associated health professionals, following an outpatient referral. Outpatient appointments relate to all appointments with a consultant led service, irrespective of the location in which the service is performed.
NEW ATTENDANCES - A new attendance is the first of a series or the only attendance at an outpatient service with a consultant or their representative following an outpatient referral. In practice, most referrals will be seen as a consequence of a GP referral request; however, referrals may also be received from a range of other sources (see Appendix 1). First attendances at an outpatient clinic that are initiated by the consultant, who has already seen the patient, are classified as review attendances i.e. following an attendance at an Accident & Emergency unit or following an inpatient admission.
NEW ATTENDANCE SEEN - This is the number of patients who attended a new outpatient appointment.
NEW ATTENDANCES DID NOT ATTEND (DNA’d) - This is the number of patients who did not attend, and failed to give advance warning to the hospital, for a new outpatient appointment. This includes patients who cancelled their new outpatient appointment on the same day on which the appointment was scheduled. These should not be confused with those who could not attend and who did warn the hospital in advance (before the day on which the appointment was scheduled).
NEW ATTENDANCE COULD NOT ATTEND (CNA’d) -
This is the number of patients who did not attend, and gave advance warning to the hospital, for a new outpatient appointment before the day of the scheduled appointment. These should not be confused with those who either did not attend without prior warning or those who could not attend and informed the hospital on the day on which the appointment was scheduled. This does not include new appointments cancelled as a result of the hospital being notified of the patient’s death.
REVIEW ATTENDANCES - A review attendance is an attendance at an outpatient service following; a new outpatient attendance, a previous review attendance, an attendance at an
Accident & Emergency unit, a domiciliary visit, or following an inpatient admission, for the same condition. Essentially review appointments are all appointments that are not a first appointment. (See Appendix 8 for further information on the categorising of attendance sequence for face to face and virtual appointments.)
REVIEW ATTENDANCE SEEN - This is the number of patients who attended a review outpatient appointment.
5
REVIEW ATTENDANCES DID NOT ATTEND (DNA’d) - This is the number of patients who did not attend, and failed to give advance warning to the hospital, for a review outpatient appointment. This includes patients who cancelled a review outpatient appointment on the same day on which the appointment was scheduled. These should not be confused with those who could not attend and who did warn the hospital in advance (before the day on which the appointment was scheduled).
REVIEW ATTENDANCE COULD NOT ATTEND (CNA’d) -
This is the number of patients who did not attend, and gave advance warning to the hospital, for a review outpatient appointment before the day of the scheduled appointment. These should not be confused with those who either did not attend without prior warning or those who could not attend and informed the hospital on the day on which the appointment was scheduled. This does not include review appointments cancelled as a result of the hospital being notified of the patient’s death.
NEW OUTPATIENT APPOINTMENTS CANCELLED BY HOSPITAL - This is the number of new outpatient appointments that have been cancelled by the provider Health and
Social Care Trust. Such cancellations do not include those cancelled by the patient (Could Not
Attend), appointments the patient did not attend without giving prior notice (DNA) and new appointments cancelled by the hospital as a result of the patient’s death.
REVIEW OUTPATIENT APPOINTMENTS CANCELLED BY HOSPITAL - This is the number of review outpatient appointments that have been cancelled by the provider Health and
Social Care Trust. Such cancellations do not include those cancelled by the patient (Could Not
Attend), appointments the patient did not attend without giving prior notice (DNA) and review appointments cancelled by the hospital as a result of the patient’s death.
WARD ATTENDANCE SEEN BY A CONSULTANT
An attendance at a ward by a patient for the purpose of examination or treatment by a consultant/doctor is an outpatient appointment/attendance. These patients would not currently be admitted to the health care provider. The care is for the prevention, cure, relief or investigation because of a disease, injury, health problem or other factor affecting their health status.
This includes:
disease (physical or mental) confirmed or suspected - inclusive of undiagnosed signs symptoms,
injury - inclusive of poisoning - confirmed or suspected,
health problem e.g. prostheses or graft in situ,
other factors influencing the health status of non-sick persons e.g i.
pregnancy, ii.
family planning, iii.
potential donor (organ or tissue), iv.
potential problem requiring prophylactic (preventative) care, v.
bereavement or other problem requiring health professional counselling, vi.
cosmetic surgery, vii.
other.
6
PRIVATE PATIENT ATTENDANCES - A private patient is one who has opted to have treatment outside the Health Service and has undertaken to pay for all expenses incurred, including treatment and accommodation costs. Private patient attendances relate to private patients who attend an outpatient appointment at a facility provided by a Health and Social Care
Trust. These should not be confused with independent sector attendances, which relate to attendances at a private sector healthcare company that is contracted by HSC Trusts in the provision of healthcare or in the support in the provision of healthcare. Any cost of these independent sector attendances is paid by the Health Service and not the patient.
REASONS FOR CANCELLATION - An outpatient appointment may be cancelled by either the provider Health and Social Care Trust (a hospital cancellation) or the patient (patient could not attend – CNA).
Hospital Cancellations may occur for the following reasons:
Consultant unavailable
Medical staff / Nurse unavailable
Patient treated elsewhere
Consultant cancelled appointment
Appointment rescheduled (brought forward)
Appointment rescheduled (put back)
Cancelled following validation / audit
Administrative Process
Hospital transport not available
Cancelled by hospital in order to rebook as alternative booking method
Patient died
1
Patient Cancellations (CNA) may occur for the following reasons:
Patient cancelled appointment as it is no longer required
Patient cancelled but the appointment is still required
GP cancelled appointment
PATIENT DIED – This is an appointment which has been cancelled due to the hospital being notified of the patient’s death. Cancellations due to the death of a patient are not included within the figures for either Patient Cancellations (CNA) or hospital cancellations.
VIRTUAL ACTIVITY - A virtual appointment is a planned contact by a Healthcare
Professional responsible for the care of a patient for the purposes of clinical consultation, advice and treatment planning. It may take the form of a telephone contact, video-link intervention, an email or a letter.
Virtual contact between a Healthcare Professional and a patient can be regarded as a Virtual
Outpatient Attendance only as long as it replaces what would have been a face to face attendance at an outpatient clinic and that it directly supports the diagnosis and care planning of a patient/client. It is not intended to facilitate the recording of every contact/phone call. Further information on the definition and recording of virtual activity can be found in the V-QOAR guidance and in Appendix 8 of this document.
7
3 COLLECTION OF DATA
OUTPATIENT ACTIVITY
All activity at a consultant led service is counted as an outpatient attendance and should be included on the return (excluding virtual and independent sector activity which is reported on separate returns). The patient does not necessarily have to see the actual consultant at such a visit, but they must be assessed by either the consultant or a member of the consultant’s team.
All activity performed by consultants and health professionals employed by the Health and Social Care Trusts in hospitals in Northern Ireland should be recorded. This includes activity performed as part of ‘in-house’ waiting list initiatives and private patient consultations.
Activity commissioned by the Health and Social Care Trusts, but performed by
Independent Sector providers, irrespective of the location of the service, should not be recorded on this return.
Activity will be reported by specialty. Specialty relates to the specialty of the consultant that performs the activity and is derived from the consultant’s contract of employment. It is recognised, however, that there may be instances where an attendance is recorded under a specialty that reflects the consultant’s contract but does not reflect the specialty that the patient attended under. Hospitals should therefore try to ensure that the consultant’s contract accurately reflects their work.
Activity should be reported irrespective of the location at which the service is delivered but should be attributed to the hospital that holds the contract for the consultant, or member of their team, that provided the service. Examples of the range of locations at which outpatient services are performed are contained in Appendix 6.
Services not controlled by a consultant e.g. those led by a nurse or Allied Health
Professionals should not be included on this return. Integrated Clinical Assessment and
Treatment Services (ICATS) are reported on a separate return.
Attendances at a group session provided by a consultant led service should be recorded as an outpatient attendance. The number of outpatient attendances will relate to the number of patients present who have identifiable patient records, even if the patients are seen together in a group. (Note this is different to a couple/family scenario – see point below.)
At some appointments a family or a couple may be treated together. The number of attendances to be recorded should be the number for whom a separate appointment was made, e.g. if a couple are seen together under the same appointment, this should be counted as one outpatient attendance. If separate appointments were made for them, this should be counted as two outpatient attendances.
Activity of consultants on domiciliary visits for which a fee is payable should not be counted as outpatient attendances. Other home visits and visits to an inpatient of a
8
different specialty, e.g. for assessment, should be counted as outpatient attendances.
Whoever has the contact collects and returns the data.
On no account should consultants visiting their own inpatients on a ward be included as outpatient attendances.
At some appointments, one or more doctors may see a patient together. In such a case only one attendance should be recorded.
If another health professional sees a patient in a consultant outpatient clinic, with a doctor, this should be recorded as a patient on the return for the appropriate discipline, as well as the attendance being recorded for the outpatient clinic, e.g. if a patient sees a consultant and an occupational therapist together, this should be recorded as one outpatient attendance and one face-to-face contact for the occupational therapist.
PERIPHERAL OUTPATIENT SERVICES
For the majority of specialties a patient’s attendance will reflect the HSC Trust to which they have been referred and the location where they attended the appointment. However, not all outpatient services are provided at each of the five HSC Trusts in Northern Ireland. In such circumstances patients from one HSC Trust may attend an appointment for a service provided at another HSC Trust, or, in other cases, a consultant, or a member of their team, from one HSC
Trust may provide a visiting ‘outreach’ service at another HSC Trust. In addition, within a HSC
Trust, a consultant may hold services at various locations within their own Trust.
These ‘peripheral’ outpatient services can therefore be:
regional specialties which are organised centrally but hold outpatient appointments throughout the five Trusts, or
consultants from any specialty from one HSC Trust that provide a ‘visiting’ outreach service at another HSC Trust.
consultants from any specialty who may hold services at various locations within their own Trust.
Data on outpatients attending peripheral services should be recorded and returned by the HSC
Trust which holds the contract for providing the service. Data should be broken down by location. With regional specialties this is likely to be the organising centre/hospital, i.e., in the case of cancer services these are reported by the Cancer Centre, Belfast. For visiting consultants
(either within their own Trust or at another HSC Trust) the contract could be either with the hospital holding the clinic, or with the consultant’s hospital/unit. The same rule applies in both scenarios; whoever has the contract collects and returns the data.
It is recognised that in some cases a patient’s records are held on the PAS box of the HSC Trust to where the patient was referred, and not the HSC Trust who holds the contract of the consultant who provides the service. HSC Trusts should therefore ensure that the HSC Trust whose consultant is providing the service either has access to these patient’s details to allow them to record this activity, or a process is set up to provide the details of this activity to them.
9
REASONS FOR CANCELLATION: REGIONAL AND SUB-REGIONAL CODES
The total number of appointments cancelled by (i) the provider Health and Social Care Trust and
(ii) the patient are reported in Section 1.1 of the QOAR (see Appendix 2).
The reason for cancellation should also be recorded for each cancelled appointment. Total number of cancelled appointments, by reason for cancellation is reported in Section 1.2 of the return (see Appendix 2).
The reason for cancellation has now become mandatory within the Health Service in Northern
Ireland for all hospitals with access to PAS, and an agreed list of regional codes and definitions can be found in Appendix 3.
Contained within each regional code is a list of agreed sub-regional codes reflecting the outcome of the audit of the ‘Short Life’ working group (the key findings of which can be found in
Appendix 4).
This list of regional and sub-regional codes must be utilised in a standardised manner across all
Trusts. If no reason for cancellation has been recorded, Trusts must report this as ‘No reason for cancellation recorded’.
If an incorrect reason for cancellation has been recorded, for example if one of the hospital cancellation reasons are recorded against a patient cancellation, Trusts must report the number of such errors as ‘Incorrect reason for cancellation recorded’.
Health and Social Care Trusts must use one of the above regional codes to record reason for cancellation. If no reason for cancellation has been recorded, Trusts must report this as ‘No reason for cancellation recorded’. Trusts must not use the reason ‘Other’.
Additional Reason for Cancellation Codes to be added to the QOAR
To ensure standardisation of codes, if Trusts require any new codes under the variable ‘reason for cancellation’, the request should be taken through the Hospital Liaison Group (HLG). As this group meets quarterly, the HLG mailing list should be used to ensure a quick reply to the Trusts request.
10
4 REPORTING OF DATA
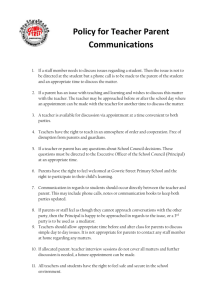
SECTION 1.1 - OUTPATIENT ACTIVITY
The number of attendances for a new (first) outpatient appointment should be reported in
Column B.1 of the return. These include private patient attendances, which are also recorded separately.
The number of patients who did not attend a new outpatient appointment and failed to give advance warning to the hospital (DNA’d) should be recorded in Column C.1 of the return.
Patients who could not attend a new outpatient appointment and informed the hospital on the day of the appointment (CNA on the day) should also be reported in Column C.1 of the return.
The number of patients who could not attend a new outpatient appointment, and informed the hospital before the day of the appointment (CNA’d), should be reported in Column D.1 of the return. This does not include new appointments cancelled as a result of the hospital being notified of the patient’s death.
The number of attendances for a review outpatient appointment should be reported in Column
E.1 of the return. These include private patient attendances, which are also recorded separately.
The number of patients who did not attend a review outpatient appointment and failed to give advance warning to the hospital (DNA’d) should be recorded in Column F.1 of the return.
Patients who could not attend a review outpatient appointment and informed the hospital on the day of the appointment (CNA on the day) should also be reported in Column F.1 of the return.
The number of patients who could not attend a review outpatient appointment, and informed the hospital before the day of the appointment (CNA’d), should be reported in Column G.1 of the return. This does not include review appointments cancelled as a result of the hospital being notified of the patient’s death.
The number of outpatient appointments as a result of a patient attending a ward for examination or treatment by a consultant should be reported in Column H.1. New and review appointments should be combined.
The number of new outpatient appointments cancelled by the hospital should be reported in
Column I.1 of the return.
The number of review outpatient appointments cancelled by the hospital should be reported in
Column J.1 of the return.
The total number of appointments cancelled as the result of the patient’s death, both new and review, should be reported in Column K.1 of the return.
Attendances by private patients are included within the main body of the return but are ALSO separately reported in Column L.1 of the return. The total number of private patient attendances, both new and review, should be reported in Column L.1.
11
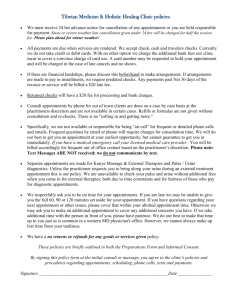
SECTION 1.2 - REASONS FOR CANCELLATION OF APPOINTMENTS
The total number of appointments (i) cancelled by the hospital and (ii) cancelled by the patient
(CNA) is also reported in Section 1.2 of the return, split by the reason for cancellation.
The sum total of cancellations, recorded in Column B.2 in Section 1.2 of the return should equate with the sum total of reasons for appointments cancelled by the hospital and cancelled by the patient, excluding patient deaths, as reported in Columns C.2 to Q.2 in Section 1.2.
The total recorded in Column B.2 of Section 1.2 should also equate with the number of appointments cancelled by either the hospital or the patient as reported in Section 1.1 of the return (Column D.1 + Column G.1 + Column I.1 + Column J.1). This is calculated automatically in column M.1. If the total number of cancellations in Column B.2 does not equate to the number reported in Section 1.1 of the return, a
‘ FALSE’
warning will appear. If this happens, you should revisit the number of cancellations and ensure that the correct number is reported in both Sections 1.1 and 1.2.
Column D.1 (new CNA) and column G.1 (review CNA) should agree in total with or be more than the total of column M.2 to column O.2 (patient cancellation reasons). This total may exceed the total of column M.2 to column O.2 as there may be some patient cancellations which have either been incorrectly recorded or not recorded.
Column I.1 (new cancelled by the hospital) and column J.1 (review cancelled by the hospital) should agree in total with or be more than the total of column C.2 to column L.2 (hospital cancellation reasons). This total may exceed the total of column C.2 to column L.2 as there may be some hospital cancellations which have either been incorrectly recorded or not recorded.
A patient cancellation on the day of the appointment should be reported as a DNA, and are therefore not included in Section 1.2 of the return.
SCHEDULE
HIB issue a timetable each quarter instructing HSC Trusts to run the Business Objects query on a particular date. This is usually three weeks after the end of each quarter, allowing HSC Trust administrative staff sufficient time to ensure their outpatient data are recorded correctly on PAS.
The timetable also includes the date by which HSC Trusts must submit their QOAR return to
HIB each quarter. Sufficient time is given to allow HSC Trusts to run their queries, collect data not recorded on PAS, and then populate the QOAR return for each of their hospital sites.
12
5 DATA VALIDATION
Each quarter, following receipt of the QOAR return from each HSC Trust, HIB validate the data by comparing figures at Hospital and at specialty level for the current quarter and against each of the four quarters of the previous year. Any irregularities are queried with HSC Trusts.
The validations queries are compiled at Hospital level for each of the five HSC Trusts. Trusts are required to provide an explanation for all queries within a week, as well as to confirm figures or provide amendments where necessary. Whilst it is mainly Part 1.1 that will be queried, on occasions queries will be raised regarding Part 1.2.
At the end of each financial year the last quarter’s data is sent out for validation, along with any outstanding queries for the previous quarters of that year, and presented to HSC Trusts for final sign-off. Trusts are given two weeks to respond to this.
13
6 DATA USE
Data submitted by HSC Trusts to the DHSSPS on the QOAR are National Statistics. National
Statistics are produced to high professional standards set out in the UK Statistics Authority Code of Practice for Official Statistics. They are required to comply with the Code’s eight Principles and three supporting Protocols including the Protocol on Release Practices.
Provisional data on the number of new attendances are published quarterly in the Northern
Ireland Waiting Time Statistics: Outpatients Waiting List Bulletin.
Following final sign off from HSC Trusts, data on new and review, attendances, did not attends and cancellations, is then published in the annual Hospital Statistics: Outpatient Activity
Statistics bulletin. The most recent publication, together with previous editions, can be found at the following link: http://www.dhsspsni.gov.uk/index/statistics/hospital/hospital-activity/outpatient-activity.htm
Outpatient activity data split by financial year, hospital, HSC Trust and specialty are also published in Microsoft Excel format at the above link.
Outpatient activity data are also used in:
Ministerial answers to both Written and Oral Assembly questions;
Departmental responses to correspondences received from the NI Assembly Health
Committee, Public Accounts Committee, Northern Ireland Audit Office and other stakeholder bodies such as the Patient Client Council;
Ministerial briefing material;
Health compendium publications, and
Responses to data requests from HSC, politicians, journalists, voluntary / charitable organisations and members of the general public.
14
7 CONTACT DETAILS
This document will be reviewed and updated periodically. Frequently asked questions can be found in Appendix 1.
If you have any issues relating to the contents of the document or the collection of outpatient activity information in general please contact:
Hospital Information Branch
DHSSPS
Annex 2, Castle Buildings
Stormont
Tel: 028 90523264 / 02890522521
E-mail: statistics@dhsspsni.gov.uk
15
APPENDIX 1: FREQUENTLY ASKED QUESTIONS
What are the main sources of referral for a first outpatient appointment?
While the majority of referrals for a first outpatient appointment will be made by a General
Practitioner, referrals may also be received from a range of other sources. A full list of the sources from which a referral for a first outpatient appointment may be received is outlined below (with Patient Administration System internal codes in brackets):
General Practitioner / General Dental Practitioner, including referrals submitted via the
Clinical Communications Gateway (CCG) (3)
ICATS following triage, i.e. where a patient is initially referred by their GP for an
ICATS service, but at the paper triage stage it is decided that the patient is not suitable to be treated by ICATS and needs to be seen by a consultant. The patient will be referred as a GP referral (3).
Accident and Emergency Department (not initiated by same consultant to whom the patient is being referred) (5)
Other consultant (other than A & E Dept) (5)
Self-referral (5)
Prosthetist (5)
Another Health Practitioner (5)
Family Planning Service (5)
Voluntary Agency (5)
Criminal Justice Agency (5)
Screening Service (5)
ICATS following a diagnostic test or treatment (5)
Should nurse led activity be reported on this return?
No. This return relates solely to activity performed in a consultant led outpatient service.
Activity performed in a non consultant led service, such as those led by nurses, allied health professionals etc should not be reported on this return.
Should ICATS activity be reported on this return?
No. ICATS is the term used for a range of outpatient services for patients, which are provided by integrated multi-disciplinary teams of health service professionals, including GPs with a special interest, specialist nurses and allied health professionals. Activity at ICATS services are not regarded as consultant led activity and should not be recorded on the QOAR.
From 1 st April 2010, a number of ICATS were officially introduced within the HSC, and a data return, the Quarterly ICATS Activity Return (QIAR), was introduced by the Department in
2010/11. HSC Trusts should submit data on ICATS activity to HIB on this return on a quarterly basis.
16
Should virtual activity be reported on this return?
No. This return relates solely to activity that takes place in a face to face environment.
However, it should be noted that prior to 2015/16 virtual activity was included on the QOAR. In
April 2015, the HSCB issued technical guidance for the recording of consultant virtual outpatient activity on PAS. Implementation of the virtual activity guidance allowed this virtual activity to be disaggregated from face to face activity. This includes any associated DNAs,
CNAs and hospital cancellations. Subsequently a separate data return for virtual outpatient activity, the V-QOAR, was introduced by the Department in 2015/16.
Any virtual outpatient activity that previously was recorded on the QOAR must now be recorded on the V-QOAR, and HSC Trusts should submit virtual outpatient activity data to HIB on a quarterly basis.
It should be noted that neither the QOAR nor the V-QOAR is intended to facilitate the recording of every contact/phone call made by the consultant, or member of their team.
Can a face to face attendance occur after a virtual attendance, and, if so, how should this be recorded?
Following a new virtual attendance it may be decided that a patient needs a face to face appointment. In this case a patient will be booked in for a review face to face attendance. The initial new virtual attendance will be recorded on the V-QOAR, but the review attendance will be counted as a review attendance on the QOAR. Any subsequent face to face review appointments will also be recorded on the QOAR. If, however, following a face to face review appointment a patient is given a virtual review appointment this should be recorded on the V-
QOAR.
Referrals for a face to face appointment from another consultant following a virtual attendance are treated as a new attendance, and should be recorded on the QOAR.
Should independent sector activity be reported on this return
No. Outpatient activity at Independent Sector providers is recorded on the Departmental Return
IS1 (Part 1), provided by the Health and Social Care Board.
HSC Trusts are provided with guidance, dealing how they should record details of patients transferred to the Independent Sector for assessment, on their PAS system. Following assessment, the Independent Sector provider informs the transferring HSC Trust who records the patient’s outpatient wait as being complete. These records are then validated against financial invoices received by the HSC Trust from the Independent Sector provider for each transferred patient. HSC Trusts then submit this data to the HSC Board.
Where should private patient attendances be recorded?
Private patient attendances relate to patients who pay a fee and attend an assessment with a
Health and Social Care consultant at a Health and Social Care facility. They are included within the main outpatient activity figures (where they should be separated into new and review attendances) and also listed in the Private Patient attendances column. Data in this column relate
17
to total attendances and are not split by appointment type. These columns should therefore not be added together.
Does a patient have to be assessed by a consultant in charge of the team in order for their attendance to be reported on the return?
Not necessarily. A patient does not have to be seen by the actual consultant in charge of the team, however in order for the attendance to be recorded as an outpatient attendance, the patient should be seen by either the consultant or a member of a consultant led service. For example, if a patient is seen by a nurse in a service that is under the overall control of a consultant, this activity should be reported on this return. If on the other hand, the patient is seen by a nurse who is not working as part of a consultant led team, the service is considered to be nurse led and should not be reported on this return.
Any contact between the patient and the consultant or a member of their team, that is not face to face, but is its equivalent, should be counted as virtual activity and recorded on the V-QOAR.
If a patient attends an appointment with a consultant, following an initial attendance at an
Accident and Emergency Department, how should this be reported?
As a result of increasing efforts to improve the quality of care provided by the health service,
Accident and Emergency attendees are increasingly being given appointments for reattendances. This has focused attention on the difference between a follow-up attendance at an
A&E clinic and an attendance at an outpatient clinic of a consultant in the A&E specialty.
The key elements of an outpatient attendance at a clinic of the A&E specialty are that the patient is given an appointment and is seen by a consultant of the A&E specialty or member of their team in a clinic with a recognised clinic purpose (e.g. Fracture Clinic, Trauma Clinic etc). This activity is recorded in the outpatient activity return as a review outpatient attendance against specialty 180. A follow-up attendance at an A&E Department is a re-attendance where the patient sees a nurse, or the patient is seen by an A&E consultant but the attendance is not within a clinic session with a recognised clinic purpose. These attendances should be reported on
KH09 (Part 2) as a follow-up attendance at an A & E Department. Any re-attendance where the patient sees a consultant of a different specialty or their team should be recorded as the appropriate outpatient attendance in that consultant's specialty.
Hence, the fact that a patient is given a specific appointment time for a follow-up A&E attendance does not necessarily mean that this attendance should be automatically counted as an outpatient attendance (rather than an A&E follow-up). The purpose of the clinic and the specialty of the consultant in charge of the clinic are critical factors. The advice contained in this answer, is particular to A&E Departments and should not be applied generally.
Does the patient have to attend a face to face consultation at a hospital in order for the attendance to be reported on the return?
Not necessarily. The face to face consultation may take place at a location outside of the hospital (see Appendix 6).
For activity performed outside of a hospital, the attendance should be attributed to the hospital that holds the contract for the consultant, or member of their team, that provided the service.
18
Should Waiting List Initiative (WLI) activity be included within this return?
Yes. Health Service patients will attend an outpatient appointment at a HSC hospital, at either a routinely provided or core consultant led outpatient service, or at a consultant led service additionally provided by the HSC Trust. These latter services (sometimes referred to as ‘Waiting
List Initiatives’) should be recorded as one would the routinely provided or core outpatient activity.
This WLI activity should not be confused with outpatient activity carried by an Independent
Sector provider.
19
General Surgery
Urology
Trauma & Orthopaedics
ENT
Ophthalmology
Oral Surgery
Restorative Dentistry
Paediatric Dentistry
Orthodontics
Neurosurgery
Plastic Surgery
Cardiac Surgery
Paediatric Surgery
Thoracic Surgery
Accident & Emergency
Anaesthetics
Pain Management
General Medicine
Gastroenterology
Endocrinology
Haematology (Clinical)
Clinical Physiology
Clinical Pharmacology
Audiological Medicine
Clinical Genetics
Clinical Genetics & Mol. Genetics
Clinical Immunology & Allergy
Rehabilitation
Palliative Medicine
Cardiology
Dermatology
Thoracic Medicine
Infectious Diseases
Genito-Urinary Medicine
Nephrology
Medical Oncology
Nuclear Medicine
Neurology
Clinical Neuro-Physiology
Rheumatology
Paediatrics
Paediatric Neurology
Geriatric Medicine
Dental Medicine Specialties
Medical Ophthalmology
Obs & Gyn (Obstetrics)
Obs & Gyn (Gynaecology)
Antenatal Clinic
Postnatal Clinic
Well Babies (Obstetrics)
Well Babies (Paediatrics)
General Practice (Maternity)
General Practice (Non maternity)
Learning Disability
Mental Illness
Child & Adolescent Psychiatry
Forensic Psychiatry
Psychotherapy
Old Age Psychiatry
Clinical Oncology
Radiology
General Pathology
Blood Transfusion
Chemical Pathology
Haematology
Histopathology
Immunopathology
Medical Microbiology
Neuropathology
Community Medicine
Occupational Medicine
Joint Consultant Clinic
TOTAL
371
400
401
410
420
421
330
340
350
360
361
370
302
303
304
305
310
311
312
313
314
315
320
172
180
190
191
300
301
142
143
150
160
170
171
Specialty
Code
(A.1)
100
101
110
120
130
140
141
810
820
821
822
823
824
710
711
712
713
715
800
830
831
832
900
901
990
520
540
550
610
620
700
430
450
460
501
502
510
APPENDIX 2: OUTPATIENT ACTIVITY DATA RETURN
Secti on 1.1 Consul tant Outpati ent Acti vi ty
Main Specialty Function
Se e n
(B.1)
0
Ne w
DNA
1
(incl
CNA on day)
(C.1)
CNA 2
(D.1)
Atte ndance s
Re vie w
Se e n
(E.1)
DNA
1
(incl
CNA on day)
(F.1)
0 0 0 0
Cance lle d Appointme nts
Ne w Re vie w
CNA 2
(G.1)
0
Ward
Attendance seen by
Consultant
(H.1)
Cance lle d by
Cance lle d by
Hos pital 3 Hos pital 3
Cance lle d following de ath of patie nt 4
Private
Patient
Attendances
(I.1) (J.1) (K.1) (L.1)
D.1+G.1
+I.1+J.1
= B.2
(M.1)
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
0 0 0 0
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
TRUE
0 TRUE
1 - Did not attend - includes patients that do not attend and do not give prior notice and patients who inform the hospital on the day of the scheduled appointment that they could not attend the appointment.
2 - Could not attend - includes patients who inform the hospital (before the day of the scheduled appointment) that they cannot attend their appointment.
3 - Ward attendance seen by consultant - includes patients attending a ward for the purpose of examination or treatment by a consultant and are currently not admitted to the hospital
4 - Cancelled appointments - these relate to all appointments cancelled by the hospital.
5 - Cancelled following death of patient - this relates to all appointments cancelled as a result of the death of a patient.
20
Secti on 1.2 Reason for cancel l ati on of outpati ent appoi ntment
Main Specialty Function
General Surgery
Urology
Trauma & Orthopaedics
ENT
Ophthalmology
Oral Surgery
Restorative Dentistry
Paediatric Dentistry
Orthodontics
Neurosurgery
Plastic Surgery
Cardiac Surgery
Paediatric Surgery
Thoracic Surgery
Accident & Emergency
Anaesthetics
Pain Management
General Medicine
Gastroenterology
Endocrinology
Haematology (Clinical)
Clinical Physiology
Clinical Pharmacology
Audiological Medicine
Clinical Genetics
Clinical Genetics & Mol. Genetics
Clinical Immunology & Allergy
Rehabilitation
Palliative Medicine
Cardiology
Dermatology
Thoracic Medicine
Infectious Diseases
Genito-Urinary Medicine
Nephrology
Medical Oncology
Nuclear Medicine
Neurology
Clinical Neuro-Physiology
Rheumatology
Paediatrics
Paediatric Neurology
Geriatric Medicine
Dental Medicine Specialties
Medical Ophthalmology
Obs & Gyn (Obstetrics)
Obs & Gyn (Gynaecology)
Antenatal Clinic
Postnatal Clinic
Well Babies (Obstetrics)
Well Babies (Paediatrics)
General Practice (Maternity)
General Practice (Non maternity)
Learning Disability
Mental Illness
Child & Adolescent Psychiatry
Forensic Psychiatry
Psychotherapy
Old Age Psychiatry
Clinical Oncology
Radiology
General Pathology
Blood Transfusion
Chemical Pathology
Haematology
Histopathology
Immunopathology
Medical Microbiology
Neuropathology
Community Medicine
Occupational Medicine
Joint Consultant Clinic
TOTAL
420
421
430
450
460
501
502
330
340
350
360
361
370
371
400
401
410
510
520
540
550
610
620
700
710
711
830
831
832
900
901
990
712
713
715
800
810
820
821
822
823
824
304
305
310
311
312
313
314
315
320
180
190
191
300
301
302
303
130
140
141
142
143
150
160
170
171
172
Specialty
Code
Number of appointments
Cancelled by either
Hos pital or
Patient
(B .2) (A.2)
100
101
110
120
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
HCON
(C.2)
0
HMED
(D.2)
0
HPTE
(E.2)
0
HCCA
(F.2)
0
HAB F
(G.2)
0
HAPB
(H.2)
Reason for cancellation of appointment
0
HCFV
(I.2)
0
HADE
(J.2)
0
HTNA
(K.2)
0
HRB K
(L.2)
0
PNLN
(M.2)
0
PCSR
(N.2)
0
PGPC
(O.2)
Reas on for cancellation not recorded
Incorrect reas on for cancellation recorded
(P.2) (Q.2)
0 0 0
APPENDIX 3: REASONS FOR CANCELLATION
Since the reason for cancellation has now become mandatory for all Trusts to record, an agreed list of regional codes and definitions can be found below.
Contained within each regional code is a list of agreed sub-regional codes reflecting the outcome of the audit by the ‘Short Life’ working group.
This list of regional and sub-regional codes must be utilised in a standardised manner across all Trusts.
Regional Code QOAR Regional Group Description Sub-Regional Codes
HCON
HMED
HPTE
CONSULTANT UNAVAILABLE
Unique to consultant staff
Used to record any consultant absence related to clinical/personal/admin reasons
MEDICAL STAFF / NURSE UNAVAILABLE
Relates to all Health Professionals (Midwife,
Medical, Nursing and AHP)
Use to record absence related to clinical/personal/admin reasons for staff other than consultants
PATIENT TREATED ELSEWHERE
Use to record an appointment which is cancelled by the hospital as the patient is already being treated in hospital, being treated by another specialty, or referred to another specialty, or appointments needs to be moved to a new location i.e. change of location or
Consultant Absent (Administrative/Management)
Consultant Absent (Clinical/Medical)
Consultant Absent (Personal)
Consultant Ill
Consultant Left Trust/Retired
Other Health Professional Absent (Administrative/Management)
Other Health Professional Absent (Clinical/Medical)
Other Health Professional Absent (Personal)
Other Health Professional Ill
Other Health Professional Left Trust/Retired
Change In Location
Currently Being Referred To Independent Sector
Currently Being Referred Within The HSC
Currently Being Treated In Alternative Care Setting
HCCA
HABF
HAPB discharged back to GP.
Used to record patients funded by the HSC but treated in the independent sector.
CONSULTANT CANCELLED APPOINTMENT
Use to record a patient who has had their appointment cancelled by the consultant as treatment is no longer required, e.g. the result of diagnostics determines that the consultant does not need to review the patient.
APPOINTMENT RESCHEDULED – BROUGHT
FORWARD
Use to record any appointments cancelled by the Hospital where the appointment has been brought forward.
This relates to appointments where the:
· date and time have been changed
· time has changed, but the date remains the same
APPOINTMENT RESCHEDULED – PUT BACK
Use to record any appointments cancelled by the Hospital where the appointment has been put back.
This relates to appointments where the:
· date and time have been changed
· time has changed, but the date remains the same
Appointment No Longer Required At Consultants Request
Earlier Appointment Requested By Health Professional
Management Of Clinic
Waiting List Management
External Incident
Funding Issues
Industrial Action
Internal Incident
Later Appointment Requested By Health Professional
Management Of Clinic
Technical Issues
23
HCFV
HADE
HTNA
HRBK
PNLN
CANCELLED FOLLOWING VALIDATION /
AUDIT
Use if the appointment has been cancelled by the Hospital as a result of validation having taken place.
ADMINISTRATIVE PROCESS
Use to record any appointment which is cancelled by the Hospital as a result of an error in the admin process – this is not exclusively confined to Booking Centre processes.
HOSPITAL TRANSPORT NOT AVAILABLE
Use to record any appointment which is cancelled by the Hospital due to a transport reason.
CANCELLED BY HOSPITAL IN ORDER TO
REBOOK AS ALTERNATIVE BOOKING
METHOD
Use for any appointment which is cancelled by the hospital as part of the implementation of partial booking.
PATIENT CANCELLED APPOINTMENT AS IT
IS NO LONGER REQUIRED
Use to record if the patient has called the hospital to cancel their appointment, and to
Validation
Audit
Administrative Error
Management of Clinic
Management Processes
Ambulance Unavailable
Alternative Rebooking Method
Change in Location
Change In Medical Circumstances
Changed To Private Patient
Patient Moved Away
24
PCSR
PGPC state that no further appointment is required.
Local codes to be removed from this regional code:
· Patient DNA’d
· Patient DNA’d previous appointment
· Problem gone (duplicate)
PATIENT CANCELLED BUT THE
APPOINTMENT IS STILL REQUIRED
Use to record an appointment cancelled by the patient due to personal reasons, where an appointment is still required.
GP CANCELLED APPOINTMENT
Use to record an appointment cancelled by the
GP following consultation with the patient.
Change In Medical Circumstances
External Incident
Patient Ill
Patient Requests Earlier Appointment
Unsuitable
Appointment Cancelled By GP
Cancellations due to the death of a patient (HRIP and PRIP) are reported separately on Section 1.1 of the return and should not be included within the figures for either Patient Cancellations (CNA) or hospital cancellations.
25
APPENDIX 4: KEY OUTCOMES OF SHORT LIFE WORKING GROUP
Impact on Patient
A cancelled hospital appointment which had an impact on the patient is defined as one where contact was required with the patient, either in writing or by telephone to discuss their appointment which would involve a change in the date/time/location of the appointment.
Measuring Impact on Patient
The measurement of the impact of hospital cancellations on the patient will be calculated as followed:
The impact on the patient when there is a ‘Change In Date’ will be measured via the regional query on Microsoft Access.
The impact on the patient when there is a ‘Change in Time but No Change in Date’ will be measured via the regional query on Microsoft Access. (This will not measure the change in hours and minutes but rather that there has been a change in time).
The impact on the patient when there is a ‘Change In Location’ will be measured via the
Sub-regional code: Change in Location, which comes under the Regional code: HPTE. This should include patients who are relocated to another hospital either within a Trust or across
Trusts.
Monitoring Impact on Patient
A monthly statistical return, submitted by HSC Trusts was introduced from July 2013.
This return is known as the Impact on Patients of Hospital Cancelled Appointments return
(IPHCOA), formerly known as the Short Life Working Group (SLWG) return.
An internal brief covering the nine month period July 2013 to March 2014 has been developed, with a further report covering the 2014/15 year planned.
It should be noted that although the figures are produced in line with the QOAR definitions and guidance document, the figures detailed in the IPHCOA are not directly comparable to the figures collected in the QOAR due to the methodological differences in the processing of the data. The QOAR data is based on attendances and cancellations within a given quarter, whereas the IPHCOA data is based on attendances (face to face and virtual) within a given month with a previous cancellation (within three months of the attended appointment) on record.
APPENDIX 5: LIST OF SPECIALTIES AND SPECIALTY CODES, BY PROGRAMME
OF CARE
Programmes of Care are divisions of healthcare, into which activity and finance data are assigned so as to provide a common management framework. They are used to plan and monitor the health service, by allowing performance to be measured, targets set and services managed on a comparative basis. In total, there are nine Programmes of Care. However, only five of these are relevant to hospital activity.
POC 1 - ACUTE SERVICES
100 General Surgery
101 Urology
110 Trauma & Orthopaedics
120 ENT
130 Ophthalmology
140 Oral Surgery
141 Restorative Dentistry
142 Paediatric Dentistry
143 Orthodontics
150 Neurosurgery
160 Plastic Surgery
170 Cardiac Surgery
171 Paediatric Surgery
172 Thoracic Surgery
180 Accident & Emergency
190 Anaesthetics
191 Pain Management
300 General Medicine
301 Gastroenterology
302 Endocrinology
303 Haematology (Clinical)
304 Clinical Physiology
305 Clinical Pharmacology
310 Audiological Medicine
311 Clinical Genetics
312 Clinical Genetics And Molecular Genetics
313 Clinical Immunology And Allergy
314 Rehabilitation
315 Palliative Medicine
320 Cardiology
330 Dermatology
340 Thoracic Medicine
350 Infectious Diseases
360 Genito-Urinary Medicine
361 Nephrology
370 Medical Oncology
371 Nuclear Medicine
400 Neurology
401 Clinical Neurophysiology
27
410 Rheumatology
420 Paediatrics
421 Paediatric Neurology
450 Dental Medicine Specialties
460 Medical Ophthalmology
502 Obs & Gyn (Gynaecology)
620 General Practice (Other)
800 Clinical Oncology (Was Radiotherapy)
810 Radiology
820 General Pathology
821 Blood Transfusion
822 Chemical Pathology
823 Haematology
824 Histopathology
830 Immunopathology
831 Medical Microbiology
832 Neuropathology
900 Community Medicine
901 Occupational Medicine
990 Joint Consultant Clinic
POC 2 - MATERNITY & CHILD HEALTH
501 Obs & Gyn (Obstetrics)
510 Obstetrics - Ante Natal Outpatients
520 Obstetrics - Post Natal Outpatients
540 Well Babies - Obstetrics
550 Well Babies – Paediatrics
610 General Practice (Maternity)
POC 4 - ELDERLY CARE
430 Geriatric Medicine
715 Old Age Psychiatry
POC 5 - MENTAL HEALTH
710 Mental Illness
711 Child & Adolescent Psychiatry
712 Forensic Psychiatry
713 Psychotherapy
POC 6 - LEARNING DISABILITY
700 Learning Disability
28
APPENDIX 6 - LOCATIONS
01 Client's or Patient's Home
The private residence (temporary or permanent) of the client or patient. Includes foster home, hotel, bed & breakfast accommodation, university halls of residence, staff accommodation (e.g. nurses home), sheltered accommodation and any other accommodation which may be used as a client's home provided it is not listed below.
02 Health Centre
A HPSS owned or leased facility for use by local GPs and supporting local related services.
03 Other GMP Premises
Premises mainly used by a GP practice for patient consultations. The distinguishing feature from a HEALTH CENTRE is that no health care services, other than those provided directly by the GP PRACTICE, are based at the premises.
04 Ward on HPSS Hospital Site
All wards on a HPSS managed hospital site inclusive of wards open day-time only.
Includes wards in HPSS Hospices and HPSS GP Hospitals.
-
06 Hospice
Non-HPSS managed residential premises, voluntary or private, registered under Article
35 of the HPSS (NI) Order 1972 for the provision of clinical pain relief and professional nursing care to resident patients who are terminally ill.
07 Other Voluntary or Private Hospital or Nursing Home
Any non-HPSS managed residential premises, voluntary or private, excluding hospices, registered under the Nursing Homes and Agencies Act (NI) 1971. Includes Mental
Nursing Homes.
Group Homes
Residential accommodation provided to cater for a small group of vulnerable persons
(e.g. mentally handicapped, mentally ill) sharing a common household. Such premises are normally unstaffed at night or have no staff on site. In the event of the deterioration of health of one or more residents, 24 hour staff attendance may be provided on a temporary basis without affecting the status of the home. Excludes Sheltered
Accommodation.
29
-
-
-
-
12 Other Residential Care Homes Managed by Voluntary or Private Agents
Any other residential accommodation providing board and personal care to the residents.
Includes homes for children, the elderly or physically disabled. Excludes sheltered accommodation.
Other Residential Care Homes should be sub-divided into:-
HPSS Day Care Facility
See definition of DAY CARE FACILITY. Also includes HPSS managed Adult Training
Centres, Work Related/Training for Work Project Areas, Nursery-type facilities and any other day care facility provided for clients or patients to enable the maintenance of function of vulnerable groups e.g. the elderly, mentally ill, mentally handicapped, physically disabled. Excludes paramedical departments.
Day Centre
Non-Residential premises provided for the day care of vulnerable groups of persons e.g. the elderly, mentally ill, mentally handicapped and physically disabled. Includes Non-
HPSS managed Adult Training Centres, Work Related/Training for Work Project Areas,
Nursery-type facilities and any other day care type facility provided for the support and maintenance of function of vulnerable persons. Excludes premises provided for the general public.
HPSS Consultant Clinic Premises
HPSS managed premises used mainly for patients to attend for consultation, examination, investigation and/or treatment including minor operative procedures. The distinguishing feature is that the main use of the premises is for hospital consultant/consultant firms and diagnostic health professionals employed by a Health
Board, to come into face-to-face contact with their patients. Includes Outpatient
Departments, A&E, Radiotherapy, Radiology and Physiological Measurement
Departments. Excludes wards, premises used primarily for Day Care, Paramedical
Departments and any other premises separately identified. Also excluded are Pathology
Departments or other areas not usually used for face-to-face contacts.
Health Clinic Premises
Non-hospital premises used for clients to attend for consultation, examinations, assessment and/or treatment. The distinguishing feature is that the main use of the premises is for community medical officers (including community paediatricians), community nurses, health visitors, community dentists and other health professionals to come into face-to-face contact with their clients. Includes Child Guidance Centres, Child
Assessment Centres, Family Planning Clinics and other 'client-contact' health premises.
Excludes General Medical Practitioner premises, HPSS Consultant Clinic Premises,
Paramedical departments and Resource Centre premises.
30
- Resource Centre
Non-residential premises for the use of multi-disciplinary or specialist teams to see clients or patients either as referrals or self-referrals for treatment, advice and information. The provision of Resource Centres are usually for the care of those persons with Mental Health or Mental Handicapped problems. Excludes General Medical
Practitioner premises, HPSS Consultant Clinic Premises, or Health Clinic and
Paramedical departments.
- Paramedical Department
Premises provided mainly for the use of paramedical professionals including audiology technicians. Excludes General Practitioner, HPSS Consultant Clinic, Health Clinics and
Resource Centres.
- School Premises
Premises used primarily for primary and secondary education. Includes sixth form colleges, nursery schools and special schools. Excludes nurseries and establishments for higher education (i.e. those providing advanced courses leading to qualifications above
General Certificate of Education 'A' Level).
- Other HPSS Managed Sites
Any other HPSS managed premises (departments or facilities) providing Health or Social
Service type care where face-to-face contacts occur regardless of the main purpose of the premises. Includes Health Education Centres, Nurseries or Crèches (excluding those classifiable to Day Care) Leisure Activity Centres and the offices and staff training premises of health or social service professionals.
35 Prison Department Establishments
Includes detention centres, youth custody centres and prisons.
36 Public Place or Street
Includes Police Station.
37 Other
Other locations not classified elsewhere. Includes first aid rooms in factories, health facilities in universities and the private homes of health or social service professionals.
31
- HPSS Nursing and Residential Care Homes
HPSS Nursing and Residential Care Homes provide facilities for clients/patients requiring residential nursing care. Medical care continues to be the responsibility of the client/patient's GP. It is on a HPSS site, owned, managed or leased separately from any hospital.
32
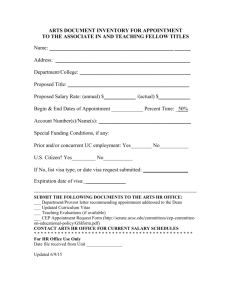
APPENDIX 7: CATEGORISING AND RECORDING OF ATTENDANCE SEQUENCE
FOR VIRTUAL AND FACE TO FACE APPOINTMENTS
Whilst virtual activity will be recorded separately from face to face activity, it should be noted that a patient may undergo a sequence of attendances that will involve a combination of the two.
Whether these will be counted as new or review attendances will depend on the precise sequence of attendances. The main scenarios (prior to discharge), and how and where these should be recorded, are discussed below.
(i) Following referral, a patient may be triaged to a core or a designated virtual clinic for a virtual new appointment. This will be recorded on the V-QOAR as a virtual new attendance. The patient may then be given a virtual review appointment, which will be recorded on the V-QOAR as a virtual review attendance. Any subsequent virtual attendances will also be recorded as virtual review attendances on the V-QOAR.
Virtual new → Virtual review → Virtual review
V-QOAR → V-QOAR → V-QOAR
(ii) Following referral, a patient may be triaged to a core or designated virtual clinic for a virtual new appointment. This will be recorded on the V-QOAR as a virtual new attendance. However, following this virtual new attendance it is decided that the patient requires a face to face appointment. This will be recorded on the QOAR as a review attendance. Any subsequent face to face attendances will also be recorded on the QOAR as review attendances.
Virtual new → Face to face review → Face to face review
V-QOAR → QOAR → QOAR
(iii) As (ii), but following the review face to face attendance that is recorded on the QOAR, the patient is given a virtual appointment. This third attendance will be recorded on the
V-QOAR as a virtual review attendance.
Virtual new → Face to face review → Virtual review
V-QOAR → QOAR → V-QOAR
(iv) Following referral, a patient is triaged to a clinic for a face to face appointment. This will be recorded on the QOAR as a face to face attendance. Following this face to face attendance the patient is given a virtual appointment. This will be recorded on the V-
QOAR as a virtual review attendance. Any subsequent virtual review attendances will also be recorded as virtual review attendances on the V-QOAR.
Face to face new → Virtual review → Virtual review
QOAR → V-QOAR → V-QOAR
(v) As (iv), but following the virtual review attendance, the patient is given a face to face appointment. This third attendance will be recorded on the QOAR as a review attendance.
Face to face new → Virtual review → Face to face review
QOAR → V-QOAR → QOAR
33
As well as the scenarios above, if patients have multiple review appointments, these could switch between virtual and face to face appointment types. Therefore, care must be taken to record this appropriately. Further information is given in the flowcharts that follow.
34
New Appointment
Referral Source 3 & 5 (NEW) &
Consultant Led. Referral triaged.
REVIEW
Face to Face
Appointment
Normal NEW Face to
Face Outpatient
Appointment
Treated as
REVIEW Virtual
Appointment
Discharged
Contact with referrer via
Letter, Email, Telephone
Discharge Referral using discharge code VADV
This code should only be
used if the referrer has been
given specific advice.
Discharged
Appointment Type
Letter - LR
Telephone– TR/RT
Email – ER
Video Link- VR
ATT
Discharged
VIRTUAL ACTIVITY includes review of Notes, Results & X-rays that are followed by contact with the patient/proxy virtually.
Treated as NEW Virtual
Appointment
Appointment Type
Letter - LN
Telephone– TN/NT
Email – EN
Video Link - VN
ATT
Treated as a
REVIEW Virtual
Appointment
REVIEW
Face to Face
Appointment
Discharged Appointment Type
Letter LR
Telephone– TR/RT
Email – ER
Video Link- VR
Discharged
Review Appointment
Normal REVIEW Face to
Face Outpatient
Appointment
REVIEW
Face to Face
Appointment
Treated as
REVIEW Virtual
Appointment
Discharged
Appointment Type
Letter - LR
Telephone –TR/RT
Email – ER
Video Link- VR
ATT
Discharged
Referral Source 2 (REVIEW) &
Consultant Led. Referral triaged.
Discharged
VIRTUAL ACTIVITY includes review of Notes, Results & X-rays that are followed by contact with the patient/proxy virtually.
Treated as REVIEW
Virtual Appointment
Appointment Type
Letter - LR
Telephone – TR/RT
Email – ER
Video Link - VR
ATT
REVIEW
Face to Face
Appointment
Discharged
Discharged
36