Pesticide poisoning user story NIOSH PHRI 2014
advertisement

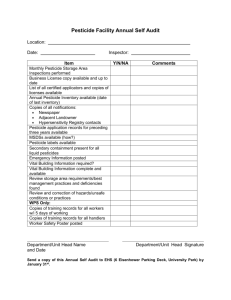
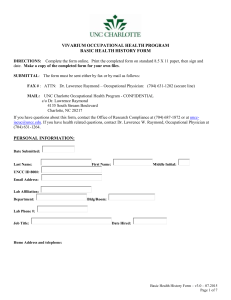
User Story: Occupational Pesticide Poisonings Contact Info: John R. Myers (jom5@cdc.gov, phone: 304.285.6005) – Supervisor Statistician, Division of Safety Research (DSR), National Institute for Occupational Safety and Health (NIOSH), US Centers for Disease Control and Prevention (CDC) E. Michael Goldcamp (ehg8@cdc.gov, phone: 304.285.5951) -- CDC/NIOSH/DSR 1.1 User Story Narrative This user story covers one setting in which data are collected: Hospital Emergency Department. A patient in his late teens presents with flu-like symptoms at a hospital emergency department in mid-August. The intake demographic data entered into the Electronic Health Record (EHR) includes date of birth, gender, home address, work address, current occupation, and current industry. Intake clinical data includes height and weight. The emergency room physician interviews the patient regarding the presenting symptoms and notes the youth is a farm worker. The physician inquires about the activities of the teen prior to the onset of the symptoms and learns that the patient was picking fresh fruit at a nearby orchard. Based on the symptomology and work activities of the youth, the physician suspects acute pesticide poisoning. This information is captured in the EHR. The electronic health record system indicates to the physician that suspected and confirmed pesticide poisonings are a reportable condition within his state and that he is to indicate if the current case is confirmed, or suspected. The physician marks the case as suspected and continues to provide symptomatic treatment to the teen. The ED information is forwarded to the state health department based on the “suspected” pesticide poisoning item marked in the EHR. The health department looks for similar EHR reports from other hospitals in the same area. Five additional “suspected” poisonings are identified that occurred on the same date. All individuals reported working for the same employer. Based on these reports, the health department contacts the state department of agriculture and initiates a full investigation of the cases. 1.1.1 Goal The goal of the initial exchange of case information to the health department is to provide timely information to public health about a pesticide chemical poisoning at a workplace. Healthcare provides details about a recent case of pesticide poisoning – e.g., within 30 days of diagnosis or treatment of the illness – to enable the health department to both follow up on individual cases and to identify workplaces or working conditions/practices that may present a current threat to the health of other workers. Further, the public health department uses data from the case reporting program to identify risk factors for occupational illness, identify populations at increased risk, and help estimate the incidence of pesticide-related illness. The resulting information is provided back to healthcare, often accompanied by information relevant to the prevention, diagnosis, treatment and referral of pesticide poisoning. Data from state pesticide poisoning surveillance programs may also be shared with NIOSH and aggregated in order to provide information about broader trends in occupational exposures and/or illness. Most states choose to use the case definition and common set of data elements provided by NIOSH for pesticide poisoning surveillance (see attached spreadsheet of data elements). 1.1.2 Data Reporting/Exchange Participants (Actors) and Events (Workflow) Events 1.The patient enters the Hospital Emergency Department (ED). 2. Initial chief complaint, demographic and expected payer information are obtained by an ED reception clerk or nurse in the ED and entered into the hospital clinical visit EHR system. Demographic and expected payer information is also used to initiate the Uniform Billing form for this ED visit. 3. Initial Chief Complaint information is forwarded to a triage nurse who determines when the patient will be summoned for further examination. 4. When summoned, the patient is taken to an examination room by a nurse, who obtains additional chief complaint information and basic medical information (temperature, blood pressure, etc…). These data are entered into the record initiated when the patient was admitted to the ED. 5. The attending physician looks at the information in the EHR, conducts the examination with the patient, orders additional tests as necessary, and enters evaluation and treatment information. 6. Based on data entered by the physician, the EHR system flags actionable items back to the physician, including clinical decision support options, or notes on reportable conditions. In this case, the system flags that suspected pesticide poisoning is a reportable condition in the physician’s state and provides the option to indicate “suspected” or “confirmed”. 7. Physician documents the reportable condition information using the EHR, which automatically sends the information to the state public health department directly or via the state data exchange system. 8. As needed, the state data exchange system forwards the reportable condition information to the appropriate State Health Department division. 9. As needed, the State Health Department queries the State data exchange system to identify similar cases that occurred on the same date as the sentinel case. 10. The state data exchange provides data on similar events to the Health Department. 1.2.3 Data See attached spreadsheet. 1.2.4 Standards Currently, health care providers (individual providers, hospitals etc.) submit data to public health departments in paper or electronic format; the method of submission varies by state and by condition. Following diagnosis by a health care provider, a report of occupational pesticide poisoning may be submitted via an emailed or faxed form or reported over the phone. (Case reports of occupational pesticide reporting are also generated by Poison Control Centers and may be sent in batches to state health departments with an occupational pesticide poisoning surveillance program; that scenario is not described here.) State public health laws set the requirements for occupational condition reporting; there are minor variations by state in the data elements collected. In general, required data elements include provider information, patient information (name, age, gender, race and ethnicity, address) patient employer and occupation, industry of employer, diagnosis, and details of incident such as place of injury, known or suspected exposures that caused the illness etc. A sample reporting form (New Jersey Department of Health) can be found at the following link: http://www.state.nj.us/health/forms/occ-31.dot At present, many of the data elements required by these reports (i.e., patient personal information and demographics, provider information) are captured in the EHR but may not be accessible from the clinical module, and interoperability standards exist to support exchange of these elements. A recent Institute of Medicine report details findings of a committee that studied the rationale for and feasibility of including occupational information in the EHR. The IOM report can be found at the following link: http://www.iom.edu/Activities/Environment/OccupationalHealthRecords.aspx. Efforts are currently underway to ensure useful inclusion of work information, including occupation and industry,, in the clinical module. NIOSH is preparing to publish a relational data model of work information for health IT. The model includes potential datasets, all of which have been coded. For example, the combination of Bureau of Census (BOC) I/O codes1 and NIOSH-added codes (e.g., for unpaid workers) – identified as the CDC_Census system in the Public Health Information Network Vocabulary Assignment and Distribution System (PHIN VADS) 2 – can be used to code patient I/O in the EHR. The CDC_Census code sets are used to classify the I/O information provided by respondents in most major U.S. health surveys. Employer information is typically present in current EHR Systems; however it may not appear in the clinical module. In addition, NIOSH has supported the development of an “Occupational Data for Health” (ODH) template for work information in the CDA social history section; the ODH template is available as a draft standard for testing with Integrating the Health Enterprise (iHE) and is being tested within the Healthy Weight profile at the 2014 Connectathon. The use of the International Classification for Disease 10th Revision Clinical Modifications (ICD-10-CM) will become the new required data standard for the Health Insurance Portability and Accountability Act (HIPAA)covered entities on or after October 1, 2014: http://www.cms.gov/Medicare/Coding/ICD10/downloads/ICD-10MythsandFacts.pdf Codes Classification systems exist to support the exchange of structured industry and occupation (I/O) and other work information data (data elements required for case reports of occupational conditions). Structured I/O data is not yet captured and managed by most EHRs but the capture of coded I/O data has been proposed as an EHR Certification Criterion for the 2017 Edition. However, fields for I/O data appear in cancer registries and death certificates. Additionally, I/O data are collected by many national surveys as text and subsequently coded. Code sets for the ICD-10CM systems, including the external cause rubric, are available at: http://www.cms.gov/Medicare/Coding/ICD10/Index.html. The ICD-10-CM External Cause Codes provide basic casual information for acute injuries and poisoning. The External Cause Codes include specific codes of the immediate cause of the injury or poisoning, activity at the time of the event, status of the person at the time of the event, and the location where the event occurred. The ICD-10-CM code source will be required for all medical facilities by CMS effective October 1, 2014. Work is currently ongoing to ensure harmonization of CDA-Release 2 and HL-7 concerning the use of the ICD-10CM code set. 1.2.4 Other Information Efforts to estimate work-related events indicates that nearly 16 workers in the United States die each day from injuries sustained at work, and 134 die from work-related diseases. Each day approximately 9,000 workers are treated in emergency departments for occupational injuries or disease. Work-related disease and injury account for a considerable fraction of total direct and indirect costs related to health outcomes. In 2005, workers’ compensation costs for employers totaled an estimated $89 billion. There are no systems in place to track occupational injuries, poisoning, or chronic conditions for the entire workforce, creating a gap in public health efforts at prevention. Electronic case reporting of occupational pesticide poisonings and other occupational conditions will remain a critical component of the public health surveillance of work-related conditions in the U.S. 1.3 Contact Information John R. Myers, MS Supervisory Health Statistician Division of Safety Research National Institute for Occupational Safety and Health (NIOSH) US Centers for Disease Control and Prevention (CDC) 1095 Willowdale Road Mail-Stop H-1808 Morgantown, West Virginia 26505 Ph: 304-285-6005 FAX: 304-285-5774 Email: jom5@cdc.gov E. Michael Goldcamp, Ph.D CDC/NIOSH/DSR Division of Safety Research National Institute for Occupational Safety and Health (NIOSH) US Centers for Disease Control and Prevention (CDC) 1095 Willowdale Road Mail-Stop H-1808 Morgantown, West Virginia 26505 Ph: 304-285-5951 FAX: 304-285-5774 Email: ehg8@cdc.gov