Cont. on measures
advertisement
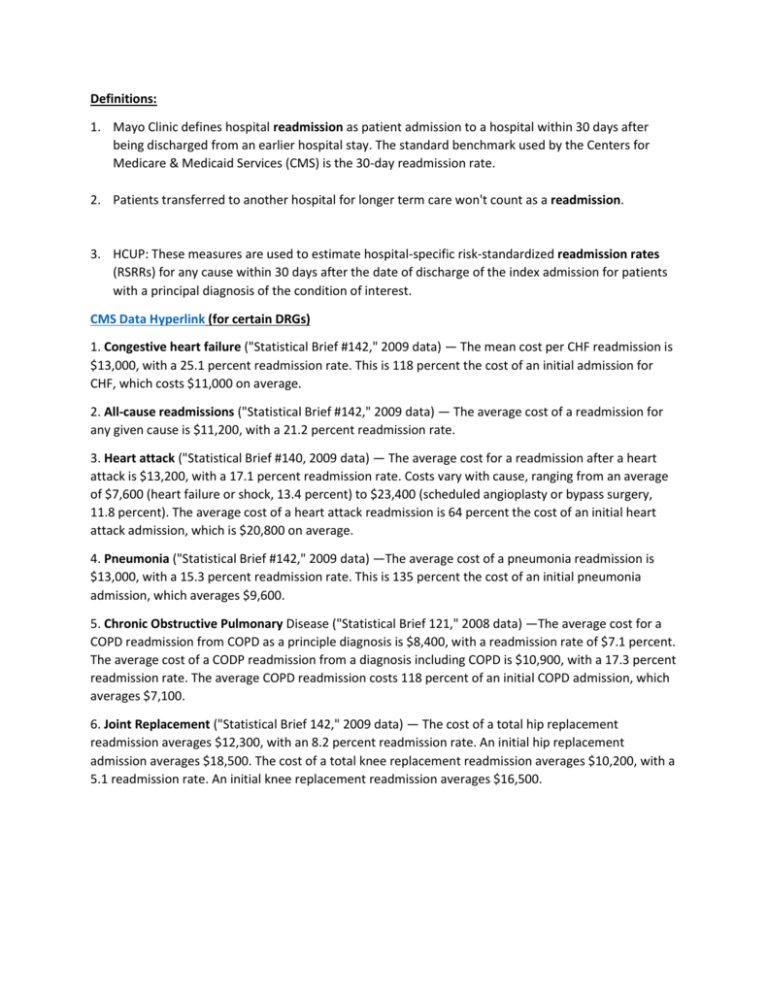
Definitions: 1. Mayo Clinic defines hospital readmission as patient admission to a hospital within 30 days after being discharged from an earlier hospital stay. The standard benchmark used by the Centers for Medicare & Medicaid Services (CMS) is the 30-day readmission rate. 2. Patients transferred to another hospital for longer term care won't count as a readmission. 3. HCUP: These measures are used to estimate hospital-specific risk-standardized readmission rates (RSRRs) for any cause within 30 days after the date of discharge of the index admission for patients with a principal diagnosis of the condition of interest. CMS Data Hyperlink (for certain DRGs) 1. Congestive heart failure ("Statistical Brief #142," 2009 data) — The mean cost per CHF readmission is $13,000, with a 25.1 percent readmission rate. This is 118 percent the cost of an initial admission for CHF, which costs $11,000 on average. 2. All-cause readmissions ("Statistical Brief #142," 2009 data) — The average cost of a readmission for any given cause is $11,200, with a 21.2 percent readmission rate. 3. Heart attack ("Statistical Brief #140, 2009 data) — The average cost for a readmission after a heart attack is $13,200, with a 17.1 percent readmission rate. Costs vary with cause, ranging from an average of $7,600 (heart failure or shock, 13.4 percent) to $23,400 (scheduled angioplasty or bypass surgery, 11.8 percent). The average cost of a heart attack readmission is 64 percent the cost of an initial heart attack admission, which is $20,800 on average. 4. Pneumonia ("Statistical Brief #142," 2009 data) —The average cost of a pneumonia readmission is $13,000, with a 15.3 percent readmission rate. This is 135 percent the cost of an initial pneumonia admission, which averages $9,600. 5. Chronic Obstructive Pulmonary Disease ("Statistical Brief 121," 2008 data) —The average cost for a COPD readmission from COPD as a principle diagnosis is $8,400, with a readmission rate of $7.1 percent. The average cost of a CODP readmission from a diagnosis including COPD is $10,900, with a 17.3 percent readmission rate. The average COPD readmission costs 118 percent of an initial COPD admission, which averages $7,100. 6. Joint Replacement ("Statistical Brief 142," 2009 data) — The cost of a total hip replacement readmission averages $12,300, with an 8.2 percent readmission rate. An initial hip replacement admission averages $18,500. The cost of a total knee replacement readmission averages $10,200, with a 5.1 readmission rate. An initial knee replacement readmission averages $16,500. HCUP Online Database: for 2012 HCUP Length of stay: 4.5 days Cost: $10,354 Readmitted within 30 days for ANY CAUSE (rehospitalization): ranges from $9,957 - $15,187 per stay Readmitted within 30 days for SAME DRGs (readmission): Ranges from $5,487 - $5,740 per stay o *Ranges is predicated on age, sex, payer, income, and residence* o *per stay is average out to be 4.5 days* Reinfection Rate / Hospital Acquired Infection: These healthcare-associated infections (HAIs) include central line-associated bloodstream infections, catheter-associated urinary tract infections, and ventilator-associated pneumonia. Infections may also occur at surgery sites, known as surgical site infections. Most Common Causes: Ventilator-associated pneumonia Staphylococcus aureus Methicillin resistant Staphylococcus aureus Candida albicans Pseudomonas aeruginosa Acinetobacter baumannii Stenotrophomonas maltophilia Clostridium difficile Tuberculosis Urinary tract infection Hospital-acquired pneumonia Gastroenteritis Vancomycin-resistant Enterococcus Legionnaires' disease Puerperal fever What does it cost to treat a HAI: Central line-associated bloodstream infections averaged about $45,000 per case. Pneumonia infections that strike patients who are put on ventilators to help them breathe cost about $40,000 per case. The most common infections, surgical site infections cost around $21,000 each to treat. There are about four C. difficile infections for every 1,000 patients who spend a day in the hospital, making them the second most common kind of infection, and those cost about $11,000 . Urinary tract infections associated with the use of catheters cost about $900 each. On average, each HAI costs the involved hospital $23,228. *GE Healthcare* o file:///C:/Users/Vanbpoun/Downloads/GE+HAI_Costs_WhitePaper.pdf o Overall depending on type and location of infection the cost can vary greatly. Average length of stay for a HAI: (PA Health care cost containment council) o 2006: ranges from 15.2 days – 25.3 days o 2007: 15.8 days – 36.2 days o *Ranges are variations of types* o http://www.phc4.org/reports/hai/07/docs/hai2007report.pdf#page=4&view=FitW,100 Adult Hospital Stays with Infections Due to Medical Care, 2007 o Jennifer Lucado, M.P.H., Kathryn Paez, Ph.D., M.B.A., R.N., Roxanne Andrews, Ph.D., and Claudia Steiner, M.D., M.P.H. o The average length of stay with an infection due to medical care was 24.4 days and resulted in a cost of $52,096. Other: DRGDescription NORMAL NEWBORN VAGINAL DELIVERY W/O COMPLICATING DIAGNOSES PSYCHOSES CESAREAN SECTION W/O CC HEART FAILURE & SHOCK NEONATE W OTHER SIGNIFICANT PROBLEMS MAJOR JOINT REPLACEMENT OR REATTACHMENT OF LOWER EXTREMITY CHEST PAIN SIMPLE PNEUMONIA & PLEURISY AGE >17 W CC SEPTICEMIA W/O MECHANICAL VENTILATION 96+ HOURS AGE > 17 Discharges AvgChgPerStay AvgChgPerDay ALOS Rank 425,649 323,156 $3,117 $11,846 $ 1,523 $5,926 2.0 2.0 1 2 159,857 141,531 82,261 79,125 $19,720 $21,836 $37,787 $7,489 $2,146 $6,365 $ 7,136 $2,837 9.2 3.4 5.2 2.6 3 4 5 6 75,428 $ 69,797 $17,699 3.9 7 70,661 64,373 $ 17,828 $38,681 $9,847 $6,723 1.8 5.6 8 9 59,683 $63,509 $8,520 7.3 10 Fractures of femur w mcc o 6.8 days @ $11,920 Fractures of femur w/o mcc o 3.0 days @ $5,538 Fractures of hip & pelvis w mcc o 5.4 days @ $9,916 Fractures of hip & pelvis w/o mcc o 3.6 days @ $5,876 Chronic obstructive pulmonary disease w mcc o 4.9days @ $8,603 Chronic obstructive pulmonary disease w cc o 4.0 days @ $7,030 Chronic obstructive pulmonary disease w/o cc/mcc o 3.2 days @ $5,616 Gastrointestinal hemorrhage o 4.2 days @ $9,479 Possible measures future measures that could optimize healthcare and decrease cost: Obesity / structured weightless regiment / nutritional guidelines o American Society of Actuaries, 2013, direct medical cost $190 billion dollars Number of hours/days/type of exercise o About 3.2 million deaths annually can be attributed to insufficient physical activity. (WHO) Health promotion o The findings of a recent health literacy costs study that was based on an analysis of US National data revealed that the cost of low health literacy to the U.S. economy is in the range of $106 billion to $238 billion annually (WHO, 2009) Early testing detectors (preventative vs diagnostic care) Use of costly new technologies and drugs (wasteful or unneeded) Correct diagnosis How much time did the physician spend with the patient GI Bleeding (nonsteroidal, Coumadin) Missed days of work o CDC, 2007: 18-64 year olds missed 4.0 days of work o AAFA, : For adults, asthma is the fourth leading cause of work absenteeism and “presenteeism,” resulting in nearly 15 million missed or lost ("less productive") workdays each year (this accounts for nearly $3 billion of the "indirect costs" shown above) Top reasons people go to the ER: 1. 2. 3. 7. 8. 9. Chest pain Shortness of breath / difficulty breathing Abdominal pain Syncope or fainting Motor vehicle accidents Fever 4. 5. 6. 10. 11. Headache Vomiting Fractures / sprains Cough Infections such as a cold or the flu What causes misdiagnosis? Premature closure occurs when a clinician arrives at an initial diagnosis that seems to fit the facts then does not consider other reasonable possibilities. Physician’s overconfidence in his or her diagnostic ability Fragmented in terms of continuity of care, and of storage and analysis of data Too little time to analyze patients Too specific of a specialist that lacks generalized training How much does misdiagnosis cost? Data not located yet. Adverse Events: Average number of AE: • 4.3% (FDA, 2004) Cost if you go to the ER: • $2,257 (FDA, 2004)