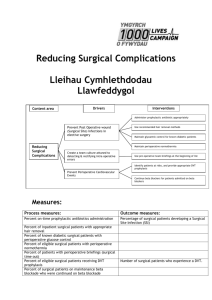
Prevention of SSI

Running head: NORMOTHERMIA 1
Normothermia and Prevention of Surgical Sites Infection
Nadezhda Litton
Ferris State University
NORMOTHERMIA 2
Normothermia and Prevention of Surgical Sites Infection
The Watson’s Theory of human Caring emphasizes the importance of a personalized
“healing” approach for nursing care. She brings that modern medicine is “hospital-centric, curecentric” (Watson, 2003). She writes that advancing care-healing practices into nursing and medicine will promote human dignity and integrity for both patient and caregiver. She developed a framework for transpersonal caring-healing nursing that incorporates her caritas into interactions between a patient and a nurse (Watson, 2206). One of the highlights of the model is understanding and accounting for “caring consciousness that transcends time, space, and physicaly,…goes beyond the given moment, and situation, and informs the future experiences”
(Watson, 2006). In this statement she underlines that the current actions of the nurse have affect on the future patient outcomes. In the article Watson (2006) uses data from Kristine Swanson’s comprehensive meta-analysis of 130 studies on caring. Swanson reports that when patients experienced caring it caused improvement of emotional-spiritual well-being, increase in safety, enhanced lives, decreased cost and increase in trust relationship (Watson, 2006).
Patient safety, comfort and well-being are parts of the nursing care. Wolf (1994) did a study of nurse caring behavior to determine what behavior of the nurse is perceive as caring by the patient and the nurse. She utilized Caring Behavior Inventory (CBI) that includes 43 categories. The results show that physical and emotional comfort is very important to the nurse and the patient (ranked 11 from 43 categories).
McNamara (1995) did study on how nurses practice caring in the perioperative settings.
One of the specifics of caring in the perioperative setting is the fact that patient unconscious or sedated. All nurses participated in the study reported safety, support, protection from harm, praying and contact with patient’s support system as a caring behavior (McNamara, 1995). In
NORMOTHERMIA 3 her study McNamara addressed that during itraoperative stage “nurses’ caring behavior shifted to attending to patients’ physical needs and maintaining safety precautions” (McNamara, 1995).
Another study by Parson (1993) indicated that patients perceive attention to their physical comfort during and post surgery as a caring behavior.
Both studies indicate that physical comfort is part of the caring behavior. Attending to the patient’s physical needs like warmth and positioning are part of the nurse caring behavior.
This behavior has immediate and delayed effect on patient outcome and overall experience. Skin integrity, wound healing, temperature control, infection, length of stay, financial and social intact on the patient could be affected by the caring behavior of the nurse in the operating room. The following evidence based practice (EBP) research project looks at nurse caring behavior as a non-pharmacological way to prevent and reduce incidence of the surgical site infection.
Wound infections are the most serious and common complications of surgery and anesthesia. Usually, they are detected five to nine days after surgery. According to CDC, surgical site infections (SSI) account for approximately 20 percent of all health-care associated infections in US hospitals (Klevens, 2007). It increases length of hospital stay and cost of medical care in the hospital and after discharge at home. Number of factors influence rate of surgical site infection-surgical technique, duration of the surgery, underlying conditions, degree of wound contamination and patient’s immune system status.
Various factors influence the host defense system. Among them are the magnitude of contamination, hemostasis, tissue perfusion, immune system function and antibiotic therapy
(Sessler, 2006). Effectiveness of the antibiotic therapy depends on time of administration and perfusion status. Magnitude of contamination could be affected by surgical technique as well as pre-existing host conditions. Bacterial wound contamination could occur from the skin or other
NORMOTHERMIA 4 sources within the patient (Sessler, 2006). Hemostasis, tissue perfusion and immune functions are factors that improve resistance to infections and facilitate healing. They could be greatly affected by vascular status and a body core temperature (Kurz, 2008).
Normothermia defined as 36.6 ±0.5°C. Anesthesia induction leads to impairment of thermoregulatory control. Body exposure, infusion of cold fluids and cold room temperature cause body heat lost and redistribution during the surgery. Unintentional hypothermia with body core temperature <36°C (96.8°F) is a common result seen in surgical patients (Unintended hyperthermia, 2007). Hypothermia causes thermoregulatory vasoconstriction and impairs immune system (Kurz, 2008). In double-blind, randomized study conducted by Dr. Kurz in
1996, 78 percent of patients with postoperative hypothermia had vasoconstriction that lasted through six hours of recovery period; and only 22 percent of patient with normal core temperature had developed vasoconstriction. Results of vasoconstrictions are impaired tissue perfusion and oxygenation that significantly could affect wound infection and healing (Allen,
2009). Hypothermia directly impairs T-cell-mediated antibody production and “non-specific” oxidative bacterial killing by neutrophils (Sessler, 2006). Kurz (1996) found that 19 percent of patients in the hypothermia group had developed surgical wound infection and only six percent in the normothermia group. In the same study, length of hospitalization had been increased due to the wound infection by six days. In another randomized study rate of SSI in normothermia group was 4-6 percent compare to 15 percent in the control group (Leaper, 2006). In the analysis conducted by Mahoney (Unintended hypothermia, 2007) it was estimated that hospitals spend
$2, 500-7,000 more per hospitalization due to increased length of hospitalization resulted from surgical site infection. This cost generally is not reimbursed by insurance companies and is a financial lost to the institution. Results of Kurz’s study (1999) indicate that intraoperative
NORMOTHERMIA 5 hypothermia triples number of the incidents of surgical site infection and prolongs hospitalization by 20 percent.
Hypothermia causes general discomfort to the patient in addition to the negative physiological impact. Shivering and feeling of being cold are common for the patients with hypothermia (Kurz, 1999). Prolonged hospital stay takes patients away from their normal life and families. Impaired wound healing requires increased use of home care and dressing supplies. It could cause delay in return to work, social life and disturbance of self and body image.
These factors have non-clinical nature, but they affect the person as a whole. The Theory of Human Care calls to take into consideration multiple non-clinical factors when we design and provide nursing care for patients. Genuine concern about the patient, including clinical outcomes and patient’s comfort, will promote earlier recovery and reduce health care cost.
NORMOTHERMIA 6
Reference
Allen, G.S. (2009). Intraoperative temperature control using the thermogard system during offpump Coronary Artery Bypass Grafting. Annals of Thoracic Surgery , 87 , 284-288.
Klevens, R.M., Edwards,J.R., Richards, C.L. Jr., Horan, T.C., Gaynes, R.P., Pollock, D.A.,
Cardo, D.M. (2007). Estimated health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Reports , 122 , 160-166. Retrieved from http://www.cdc.gov/ncidod/dhqp/pdf/hicpac/infections_deaths.pdf
Kurz, A. Sessler, D., & Lenhard, R. (1996). Study of wound infections and temperature group:
Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. New England Journal of Medicine, 19 , 1209-1216.
Kurz, A. (2008). Thermal care in the perioperative period. Best Practices and Research clinical
Anesthesiology, 4 , 627-644. doi: 10.1016/j.bpa.2007.10.004
Leaper, D. (2006). Effects of local and systemic warming on postoperative infections. Surgical
Infections , 7, 101-103.
McNamara, S.A. (1995). Perioperative nurses’ perceptions of caring behavior. AORN Journal , 2 ,
377-388.
Parsons, E.C., Kee, C.C., & Gray, D.P. (1993). Perioperative nurse caring behavior. AORN
Journal, 5 , 1106-1114.
Sessler, D. (2006). Non-pharmacologic prevention of surgical wound infection. Anesthesiology
Clinics , 2 , 279-297.
Unintended hyperthermia: The importance of maintaining normothermia. (2007). Continuing
Education Workbook.
Eden Prairie, MN: Arizant Healthcare.
NORMOTHERMIA 7
Watson, J., &Foster, R. (2003). The attending nurse caring model: integrating theory, evidence and advanced caring-healing therapeutics for transforming professional practice. Journal of Clinical Nursing, 12 , 360-365.
Watson, J. (2006). Caring theory as an ethical guide to administrative and clinical practices.
Nursing Administration Quarterly, 1 , 48-55.
Wolf, Z.R., Giardine, E.R., Osborn, P.A., & Ambrose, M.S. (1994) Dimensions of nurse caring.
Journal of Nursing Scholarship, 2 , 107-111.