Relational Malpractice And the Transformation of Healthcare Law
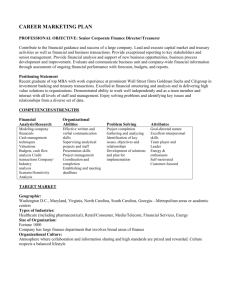
advertisement

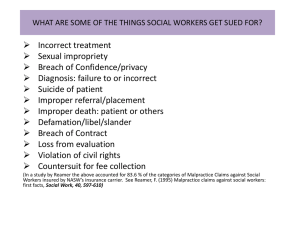
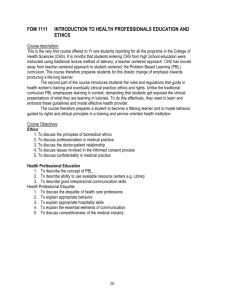
RELATIONAL MALPRACTICE AND THE TRANSFORMATION OF HEALTHCARE LAW Sagit Mor and Orna Rabinovich-Einy I. II. III. IV. V. VI. I. Introduction Relational Healthcare Law A. Situating Malpractice Within Healthcare Law B. The Search for Coherence in Healthcare Law C. Adopting a Relational Approach to Healthcare Law The Centrality of the Doctor-Patient Relationship under a Relational Approach A. The Nature of the Doctor-Patient Relationship B. The Benefits of a Collaborative Doctor-Patient Relationship Model C. The Law as a Barrier to a Collaborative Doctor-Patient Relationship Doctor-Patient Relationship in the Shadow of Malpractice A. Consumed by Malpractice: Doctor-Patient Interactions as a Battle Zone B. The Sources of Current Tensions in Doctor-Patient Relations C. Partial Measures for Improving Doctor-Patient Interaction No Fault as a Means for Transforming the Doctor-Patient Relationship A. The History of the No Fault Alternative: From Compensation to Learning B. Relationships as a New Justification for No Fault C. Designing An Alternative with Relationships in Mind Conclusion Introduction Legal scholarship in recent decades has devoted considerable attention to the "malpractice crisis." However, the vast majority of this literature has overlooked the essence of the problem. So far, mainstream legal writing on malpractice has tended to frame the problem as either an insurance crisis or a litigation crisis. The insurance crisis claim focuses on the rise in professional insurance premiums as a result of exceptionally high awards, while the problem of litigation stems from the ills of the court system—its high costs, unpredictability and the distorted incentives it provides. In this article, we offer an alternative understanding of the true nature of the malpractice predicament: the decline of the doctor-patient relationship. The framing of the problem in terms of relationships paves the way for a paradigm shift in the medico-legal analysis of malpractice specifically and of healthcare law more generally through the adoption of a relational approach. On one level this paper offers a fresh approach to malpractice reform highlighting the limitations of current approaches, which have failed to frame the problem and the solution in terms of a relationship crisis. On a deeper level, the article uncovers a fundamental organizing principle for healthcare law more generally—the centrality of relationships, most notably the doctor-patient relationship. As we show, the theme of relationships cuts across various controversies and debates that dominate the field, such as bioethical 1 dilemmas, informed consent and managed care, and has played a central role in the medical profession’s own understanding of what lies at the core of high quality medical services. The relational approach we adopt can contribute to the current efforts to characterize the field of healthcare law and draw its boundaries. So far, however, legal writing on healthcare law has largely neglected the role of relationships, focusing on other complementary themes, such as trust, that have historically characterized the field. While legal scholarship has rightly contributed to the disenchantment with old style professional medical paternalism, it has also been active in hampering the development of a viable alternative. We offer a relational understanding of malpractice, which highlights the fact that contemporary doctor-patient interactions resemble a battle zone: Most physicians view "every patient as a potential malpractice lawsuit," while patients complain that their physicians are driven by financial incentives, treat them brusquely and fail to provide honest and full information. Our findings reveal that these dynamics have colored the entire doctor-patient relationship, extending well beyond those discrete instances in which a medical error has occurred. While physician communication patterns have typically been tied to longstanding professional and organizational cultures, our research uncovers the role the law has played in cutting off communication channels between providers and patients. These developments have permeated the entire web of relations in the healthcare arena, but most notably the doctor-patient relationship, the major relational axis in this context. Our relational approach draws on the existing medical literature, which has long acknowledged the importance of the doctor-patient relationship as a fundamental component in the provision of healthcare services. Such literature has recognized the malpractice context, acknowledging the links among relationships, errors, and quality, and underscored the significance of a collaborative doctor-patient relationship for the quality of medical services delivered. We define a “collaborative relationship” as one that is premised on a mutual, open and cooperative discourse. Such a mode of interaction has been linked with enhanced physician ability to draw relevant medical information from patients, greater motivation by patients to seek treatment and to adhere to treatment, and increased patient satisfaction. Despite these findings, the dominant model of doctor-patient relations has been a defensive, hierarchical and closed mode of communication, which we refer to as "oppositional." Current research on the doctor-patient relationship proves that the existing malpractice regime does not allow for a collaborative relationship to evolve. To the contrary, it harms 2 the doctor-patient relationship by providing disincentives for open, free flowing communication by breeding distrust, conflict and defensiveness. Specifically, these studies have disclosed the manner in which torts law has shaped doctor-patient communication in the aftermath of an error: Doctors are driven to cut off communication following an adverse event, failing to supply patients and family members with basic information and emotional support. Paradoxically, this has actually motivated patients to sue their doctors, as research findings show that patients' decisions to sue are connected to their interaction with their healthcare providers rather than the pursuit of monetary compensation. Our research uncovers the deeper and more elusive nature of the impact of torts law on the doctor patient relationship, extending well beyond the moment of error and resulting in an overall relationship crisis. Such crisis has hampered doctor-patient communication along the entire continuum of care and has reduced the quality of healthcare services. Based on the above findings, this article advances the view that the law governing medical errors should adopt a relational perspective. The implications of such an approach are twofold. First, adopting a relational approach would entail examining the impact legal arrangements have on the doctor-patient relationship and the web of relations that surround it. Second, a legal regime concerned with relationships would promote a collaborative model of doctor-patient relationships. Efforts to transform the malpractice regime have taken the following principal forms: piecemeal tort reform, contractual liability, apology laws and disclosure conversations, and no fault liability schemes. In our article, we explain why none of the first three options can be expected to bring about a real transformation in the doctor-patient relationship and opt for the adoption of a no fault administrative regime. While the no fault alternative is by no means new, former proposals have sought to advance different goals. Earlier proposals focused on just compensation based on the larger pool of claimants and a better screening process for just complaints. Over time, a different justification has emerged focusing on error prevention and patient safety through systemic learning about the sources of errors. Learning would be facilitated by the removal of individual blame. A principal problem with these proposals was that they were unsuccessful in garnering the requisite political support. However, the recent Healthcare Reform grants project, which calls for the development of alternative liability schemes, may alter the political economic climate, generating a broader support-base for such reform and setting the stage for states to experiment with such regimes. No less important in our view is the fact that existing calls for adopting no fault schemes have failed to address the broader connection between medical errors and the doctor-patient relationship. Consequently, they have also failed to spot the root-cause of the crisis as well as the opportunity to address it effectively. 3 Our relational approach brings to the fore a new justification for the shift to no fault: the transformation of doctor-patient relations and a corresponding reduction in medical errors and enhancement of patient safety. This alternative assigns weight to the empirical findings on the connection between the doctor-patient relationship and quality of healthcare. Such reform would require setting the cultivation of collaborative relations as a goal, expanding the pool of disputes handled systematically, and establishing broad criteria for learning that cover the domain of relationships. This would allow for a more open and rigorous inquiry into the causes of medical errors, as well as lower conflict levels that are often a diversion for healthcare providers and serve to reduce patient trust. The significance of the new justification stems from the following: (1) it highlights the fact that the harm created by the current malpractice regime extends beyond the occurrence of medical mistakes infiltrating a broad range of physician-patient interactions, (2) it provides a more comprehensive explanation for the ways in which a no fault alternative can enhance prevention of medical errors, and (3) it more effectively addresses some of the critiques voiced against the no fault alternative in light of the cost savings and enhanced learning that will emerge from the study of a broader dispute base. We therefore argue that a transformation in the nature of doctor-patient relations can only be achieved by displacing the current malpractice regime and adopting a no-fault based solution centered on relationships. The paper proceeds to examine its principal theses as follows: Part II situates malpractice within the broader framework of healthcare law and delineates the contours of a relational approach to healthcare law-related issues. In Part III we establish the doctor-patient relationship as a central theme in healthcare law in general and in the malpractice area in particular. Part IV portrays the current state of doctor-patient relations as a battle zone, and underscores some of the historical sources that have contributed to the combative nature of the interaction between healthcare professionals and patients. We show that targeted efforts to transform such interaction have had a limited effect at best. In Part V we present the no fault alternative, highlighting the novelty of the relational justification presented in this article for choosing this particular regime: the need to do away with the malpractice system in order to improve doctor-patient relations. We then explain why the adoption of a no fault system for compensating victims of medical errors would not only be a better avenue for redressing such patients and preventing future mistakes, but also for bringing about a deep change in doctor-patient interaction. We conclude with some thoughts on the potential of a relational approach to malpractice to serve as a blueprint for a more radical transformation of the way we think about the field of healthcare law. 4